High Protein Diet- Health Risk Correlations
Scarcity is the rule of protein in nature. In evolutionary terms, anthropologists have proven that hominids lived an average of 15 to 25 grams of protein a day. In the modern western type of high-protein diet, we would consume that amount for breakfast only.
Milos Pokimica
Written By: Milos Pokimica
Medically Reviewed by: Dr. Xiùying Wáng, M.D.
Updated January 3, 2026Key Takeaways:
– Excess protein consumption can lead to an increased risk of cardiovascular disease, osteoporosis, inflammation, metabolic acidosis, elevated phosphorus levels, increased risk of cancer, autoimmune diseases, and kidney problems.
– High dietary protein consumption leads to higher levels of urea and other harmful metabolic byproducts, which can have negative health correlations. Elevated BUN levels are correlated with serious health conditions like oxidative stress, inflammation, cancer, immune diseases, cardiovascular disease, neurological diseases, premature aging, etc.
– Eating a high-protein diet will not necessarily help you lose weight or build muscle.
– Excessive protein consumption has been linked to an increase in inflammation and oxidative stress, as well as an increase in cholesterol and saturated fat consumption.
– Studies have shown that animal-based proteins may cause an imbalance in the gut microbiome and offer a pro-inflammatory profile. Plant-based proteins may be a better choice for overall health.
– Individuals who have medical conditions such as kidney failure, liver disease, diabetes, or cancer may need to monitor their protein intake to avoid exacerbating their condition.
High Protein Diet.
All of the science showed us repeatedly and conclusively with no doubt that if you eat less protein, you will be healthier and if you eat whole food plant-based diet you will be the most healthier of all, and you will live longer. Most people reading this sentence would have an immediate negative response. I am sorry but you have been lied to your entire life and in real science that you would learn in this article you would understand the real truth. After reading this article you can do your own research and I would recommend that you reconsider your beliefs that had been systematically and deliberately embedded into your subconscious mind by your MD and by the industry.
You might even suffer from food-related anxiety if you don’t consume an excessive amount of protein during the day. It is a form of Nervosa in the same psychological category as anorexia nervosa just this type of phycological disorder is never recognized and treated because industry and medicine want you to have it for reasons that you would understand if you read correlated articles about allopathic medicine and big pharma. High protein diets are not healthy just because of the protein alone plus protein comes with baggage if you eat a high protein animal products-dominated diet. If you eat a plant-based high protein diet it is still bad nonetheless if you constantly add protein powders everywhere.
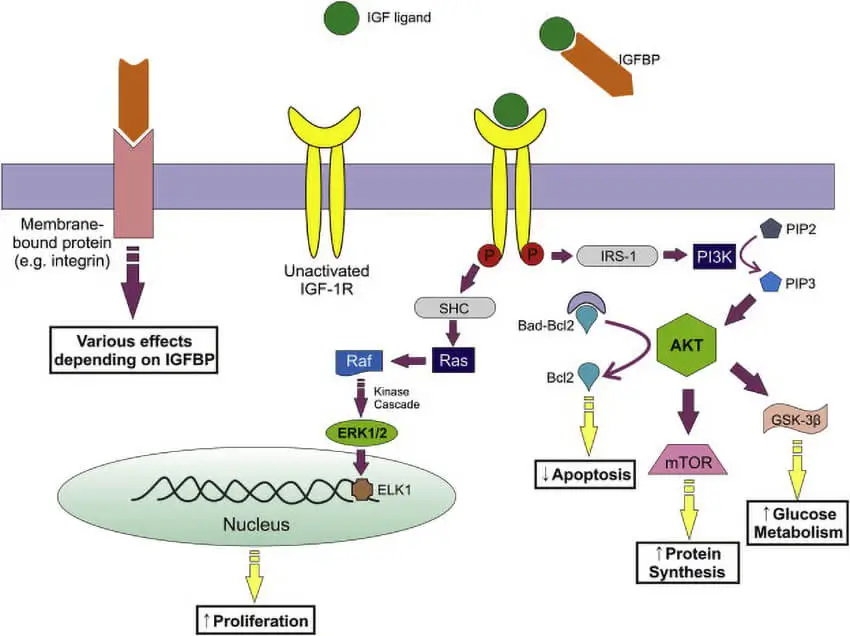
A high protein diet will not help you lose weight, it might help you to lower the catabolism of your mule tissue by increasing IGF-1 but it would also help you to accumulate DNA damage. A high protein diet is not congruent with the last 50 million years of hominin evolution and it has health risk correlations that you would learn in this article with all of the scientific references you need to further do your own research outside of mainstream propaganda. I want to say this again.
All of the science showed us repeatedly and conclusively with no doubt that if you eat less protein, you will be healthier and if you eat whole food plant-based diet you will be the most healthier of all, and you will live longer.
That is what science has repeatedly shown us through experiments. However, what is the main reason for this state of being?
When you eat plant-based, you get less, and you get less complete protein. Now that is the one reason that was shown with extensive research to be the main culprit in longevity and health. Eating much less protein than the standard American diet eaters do. And if you don’t want to believe and don’t care keep reading.
When you avoid excessive food intake and eat mostly starch or other plant-based products, what is the side effect of that?
The side effects are that simply you eat much less protein, and that is the secret industry knows but doesn’t want to tell you. Science is here and had been here for a long period of time. When all of those scientists went to the blue zones of longevity to research indigenous people to find the reason why people there are so long living and healthy, they could just tell you the truth. They eat much less protein. But they did not.
Why is it so hard for Western Civilization to accept that protein is poison in excessive amounts?
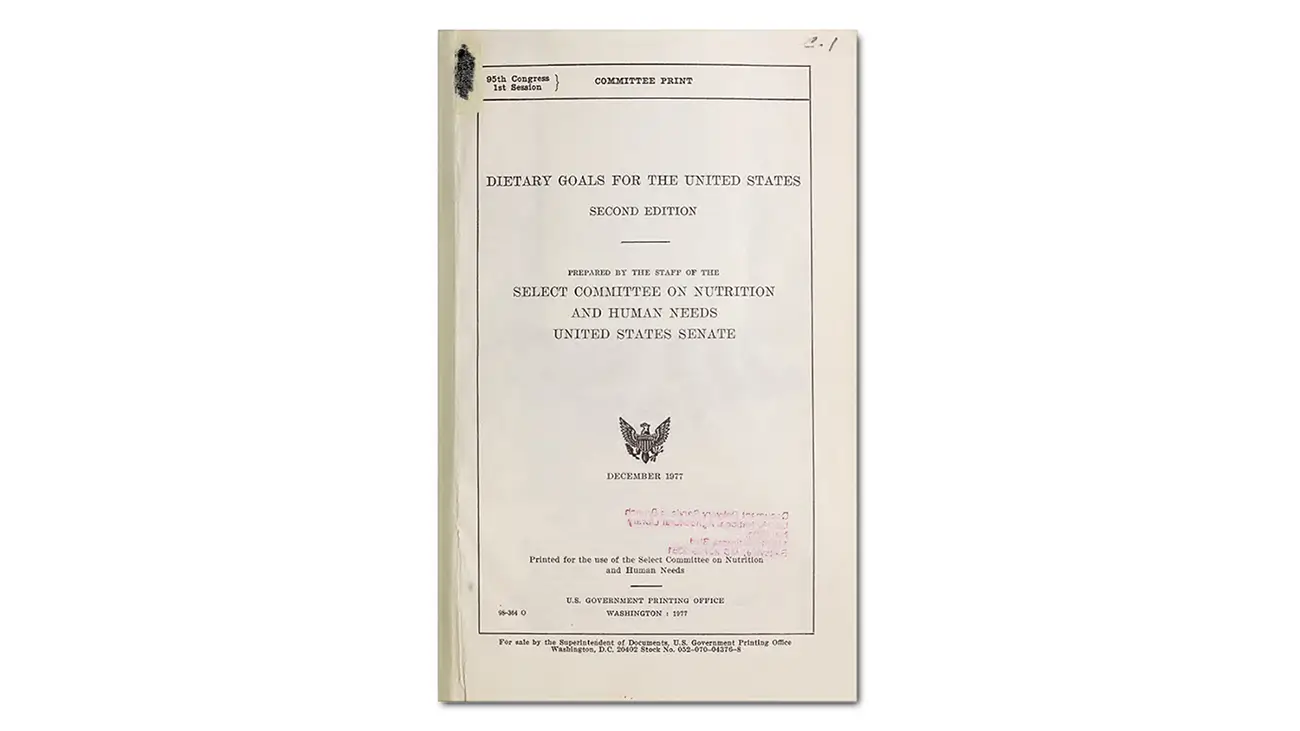
Because you will have to eat less pizza? If you eat fewer animal products you will automatically eat less protein. For the reason that you will understand by the end of this article, protein has become “the holy cow“ of nutrition, and not by accident.
It is politically, morally, and in any other way bad to talk the real truth about protein. Just look at the nutrition and medical doctors of today. For them it is easy to say eat less fat and add more carbs or starches or eat healthier fats and fewer starches but what about the real truth? Why do all of those nutrition experts, doctors, and scientist don’t tell you the real truth?
And that is eating less protein.
Where did the Chinese in the rural part of China get the protein? They eat just white rice.
What about the rural part of India or Nepal? Where is protein there?
I am not saying these people are as healthy as they can be, they are not eating optimal diets by a long shot but where is their protein deficiency? If you get most of the calories from rice surely by the American standard, you will be long gone from protein deficiency. However, guess what, these people are still there, and they do not have any, not just protein but any individual amino acid deficiency and their children don’t have Kwashiorkor.

Someone lied to you, and that someone is your regular MD.
These people that get no protein in their diet by Western standards live a very long life, and they are very healthy. Well as long as they do not move to big cities to work in factories or moved to the west and increased their protein or in other words animal products consumption. Then they start to have a chronic disease. So it has nothing to do with the fat or carb levels they ate from plant sources. Just about the levels of complete animal proteins, they ate. And that is the truth, the elephant in the living room, that no one likes to talk about or even mention.
Autophagy.
I already mention the mechanism known as autophagy (self-eating in ancient Greek)( Calorie restriction, Autophagy, Longevity, and Muscle loss).
Imagine this you don’t lose any protein.
Let me write this again, you, your body has evolutionarily adapted to save anything that it can be saved including your dead cells. Every cell that dies in your body no matter what it is, if it is not infectious, will be recycled. You eat yourself every day. You even eat like a vampire your own blood. The color of the stool is a consequence of hemoglobin digestion. Any cells that die in your body will be recycled. A red blood cell, any other immune cell any organ cell, and so on. Let me write this again for all of those let’s get some gains bodybuilders out there, you don’t lose any protein, it just gets recycled over and over and over and over again until you die.
Why there are obligatory 25 grams, well because you do lose some but only when you eat.
If you do not eat, you don’t lose anything but when you eat some of your own cells in the digestive tract will be lost. Your poop is the marker and when measured the average man of 150 pounds loses about 25 to 35 grams a day of his own protein from the intestinal lining as a consequence of digestion of food or other factors. The average man will also lose some of the protein in the growth of nails, hair, and skin. But that is in a range of a couple of grams a day. That is the accepted medical school line of thinking today.
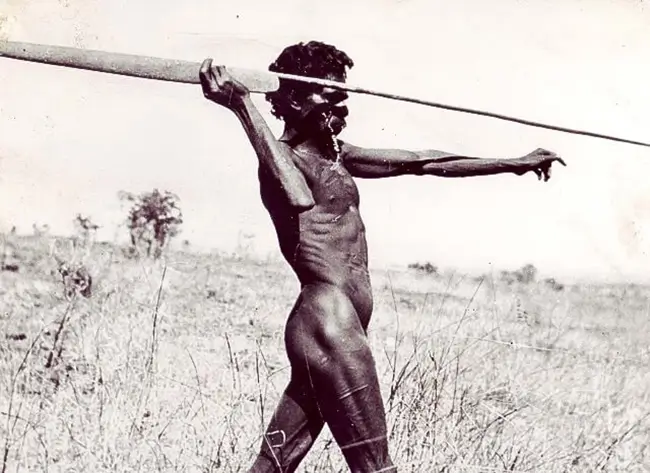
Everything more than 25-gram needs to go to energy production, and there is your nitrogen. However, also I want to mention this, many indigenous people eat much less protein and live a full healthy life. 25 grams that you will lose in excrement is for a standard American unhealthy diet. There are some indigenous people in Africa able to live their entire life on 15 to 20 grams of protein a day. The truth is, the healthier the diet, the less you lose. Recycling is the real answer. You eat less you recycle more. You eat more you lose more. Our body is smart, and it knows how to keep us in balance.
When you read 25 to 35 grams, even that is extremely generous. In reality, we need even less than that. It would be best if you told this to your gym 200 grams of protein a day manipulated frat boys. Protein has a much more toxic effect on our bodies than you can even believe. It can even give you cancer. However, wait proteus comes from ancient Greek and means the first or primary, and everybody you know always told you that protein is one of the most important macronutrients. The scientist will tell you that every cell in your body is made of proteins and what is the result. The result is that we start to think that the more protein, the better, and that we must consume it in large amounts and of course eat all the food products that have a high percentage of protein like meat and dairy.
However, if you recycle protein almost to 100 percent extent and lose only a small amount then what is going to happen with all of that extra protein you eat?
Your body does not need it, so it is going to be transformed into fat for later energy use. To make things even worse proteins that are made of amino acids are one of the most scarce things in nature, so our bodies have adapted special mechanisms to extremely well absorb all of that protein. More than 80 percent of protein in the food you eat is going to be absorbed, and that is because the amino acids are the one thing that our body actively absorbs. What does that mean?
Well, it means our bodies will do anything that they can to absorb every amino acid they can.
We are not able to downregulate protein absorption. We never had this problem in our evolution until now. In contrast minerals, for example, are passively absorbed into the bloodstream. They are just going thru the intestines, and our body does nothing except let some of them naturally pass through the inner line. They have a hard time being absorbed. It is because in nature in normal conditions million years ago food was filled with minerals, and our bodies didn’t need to develop any mechanism for mineral absorption. They even compete with each other for absorption, and our bodies do nothing to absorb them. Minerals through diffusion only are absorbed into the circulation. However, now when we eat produce from land that is mineral deficient and only has a small number of minerals that are from artificially dropped fertilizers and we do not have a mechanism for mineral absorption but have all of the animal products we can eat the situation is going to be bad.
We will have an abundance of protein in our diet like never before and lack most of the minerals we need. We are now or at least most of us completely deficient in most of the trace and some of the essential minerals and overburdened with too much pro-actively absorbed protein that our bodies need to deal with.
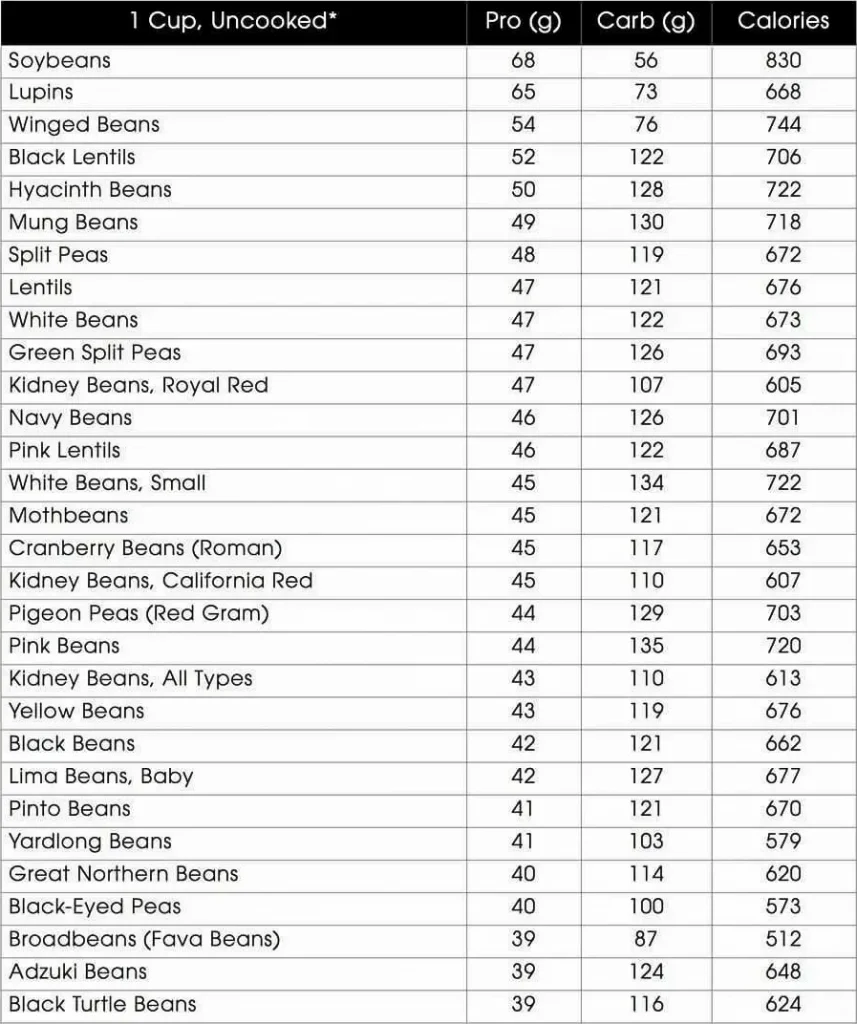
Scarcity is the rule of protein in nature.
Now how much protein, for example, does one cup of kale has? It has 5 grams of protein. And this protein is complete as any animal protein or any other “complete“ protein you can imagine. There is no such entity as an incomplete protein. Every protein on earth from any food source has all essential amino acids. When there is talk about the completeness of protein, there is talk about similarities of the source of protein to our own. Every protein has all essential amino acids but in different proportions. So when there is talk about completeness is just how much of the proportion of amino acids in the protein match proportion of amino acids in our own cells. This can have health correlations but as long as you eat more than two different things in your life and are not chronically malnourished you would be fine.
The entire story about the completeness of protein is a complete lie. Every food you eat that is correct will have a different profile of amino acids.
If you eat different foods you will get different profiles of amino acids what is that called? It is called a complete protein. Why? Because our body has a reserve, a pull of essential amino acids that are filled with various essential amino acids when they are in excess.
What is the first problem with protein?
Nitrogen.
The first problem is that our metabolism is very efficient in converting carbs to fats and another way around, but when it comes to protein, it is a whole different story. Proteins are unique macronutrients that are different from the two others.
Why is protein so different?
It is because it contains an atom called nitrogen. All proteins have nitrogen in them.
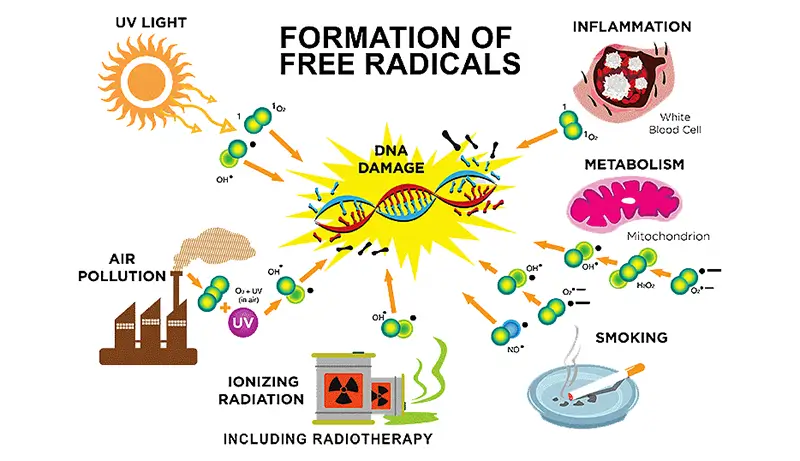
What is a big deal then with this nitrogen? Well, the body needs to do something with that nitrogen so that it can use protein as energy. What that nitrogen does is pollute the entire process sort of speaking. We want to burn clean and remain toxin free. Nitrogen is a dirty byproduct that the body needs to deal with. Our cells don’t need to be overburdened with toxic byproducts of energy production. It will burden them and create damage.
If we have too much nitrogen in our bodies, we will suffer the toxic effects of it. We might don’t feel the immediate pain, but the damage will be there. For comparison initially, you don’t feel cancer cells growing inside you either. In terms of amino nitrogen excretion, the animal kingdom can be classified into ammonotelic (ammonia), ureotelic (urea), and uricotelic (uric acid) organisms depending on the nature of the discharged substance. This process of nitrogen elimination is known as nitrogen balance.
Nitrogenous wastes include ammonia, uric acid, urea, and creatinine.
The nitrogen-containing amino group is removed and converted to ammonia. Urea, the principal nitrogenous waste product of amphibians and mammals, is synthesized in the liver from ammonia and carbon dioxide by a sequence of reactions, known as the urea cycle. Urea is produced as a non-hazardous soluble vehicle for the removal of excess nitrogen originating from the catabolism of amino acids. A major function of the liver is urea biosynthesis.
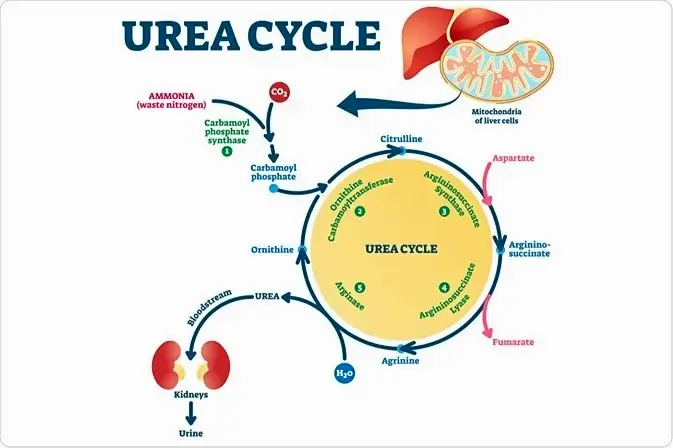
This metabolic waste is basically what we force our body to do so when we eat more than 30 grams of protein in a day. If you have renal disease or a problem with the kidneys you would have to work harder to get rid of the extra nitrogen and waste products of protein metabolism.
These harmful metabolic complications in protein metabolism are in addition to all other health correlations that a high-protein diet has.
When we have a high dietary intake of protein we will also have higher levels of urea and other nitrogenous waste products.
This is a consequence that we would not be able to avoid. Numerous studies have shown that high dietary protein consumption is associated with higher blood urea nitrogen (BUN) concentrations. For instance, there was a crossover study of 24 healthy young men who consumed a high protein diet of 2.4 g/kg per day, versus a diet with a “normal” level of protein of 1.2 g/kg per day (Frank et al., 2009). This normal protein diet was actually by itself a high protein diet. They had a diet for 7 days each and BUN concentrations were measured. BUN concentrations were significantly higher during the period of higher protein intake than during the period of normal protein intake. In this study (Weiner et al., 2015) there was a reduction in BUN with dietary protein restriction. If there is one thing that you don’t want is elevated urea. It has so many negative health correlations that it is terrible. It is by itself correlated to a large degree of serious health conditions. Almost everything that is correlated to chronic inflammation from cancer to immune diseases to cardiovascular disease by endothelial dysfunction to neurological diseases to premature aging to whatever you want you can add here…. The theory holds that high circulating BUN levels, by enhancing protein carbamylation ( protein carbamylation is a hallmark of aging) generate reactive oxygen species or in other words free radicals. An increase in ROS leads to increased oxidative stress and inflammation.
Metabolic acidosis.
A diet with high protein intake might also lead to metabolic acidosis, particularly among patients with chronic kidney disease (CKD) that already have impaired acid excretion and generation of bicarbonate. The situation is even worse if the source of the protein is animal-based foods. Additionally, dietary acid might also be a risk factor for CKD through intra-renal mechanisms that include stimulation of the production of aldosterone, the production of angiotensin II and endothelin-1, as well as the generation of ammonia. All of these promote kidney injury through inflammation and fibrosis (Wesson et al., 2020). The SAD diet (standard American diet), where protein comprises in the best case scenario of no less than 15% of calories, is estimated to produce a dietary acid load of approximately 1 mEq/kg per day which is a lot or much more than our body is used to. The majority of that acid comes from the metabolism of foods from animal sources such as meats, eggs, and especially cheeses (Lennon et al., 1966).
In contrast, by including a higher proportion of foods with natural alkali, such as fruits and vegetables, a vegan diet is nearly acid-neutral. Plant-based foods can be used to reduce both the dietary acid load and the severity of metabolic acidosis (Scialla & Anderson, 2013). Similarly, a low protein intake in patients with advanced nondialysis CKD has also been shown to attenuate the severity of metabolic acidosis.
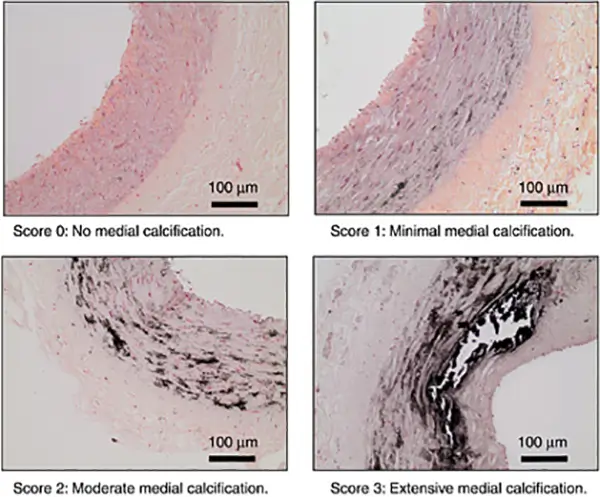
Phosphorus levels.
Dietary protein intake is also strongly correlated with phosphorus intake. Protein consumption may account for 84% of dietary phosphorus intake. Elevated phosphorus or (Hyperphosphatemia) is a serious or one of the major factors for mortality in patients with CKD. If you have issues with the kidneys, consumption of dietary phosphorus has to be controlled. Several large epidemiologic studies have also found other correlations with hyperphosphatemia. Higher phosphorus levels (even those within the normal range) are also associated with an increased risk of mortality in cardiovascular disease even in individuals with normal kidney function. Why this happens is because of calcifications in the arteries and it is a complicated science that you probably won’t be interested to know. Dietary phosphate will increase the expression of fibroblast growth factor 23 and elevated FGF-23 levels are associated with vascular calcifications among patients with CKD and left ventricular hypertrophy in experimental animals with uremia.
IGF-1.
There is a higher level of correlation between a high protein diet and cancer than that is between smoking and lung cancer.
One of the reasons why one in four people will die from cancer is not genetics but a high-protein diet. A high protein diet is the number one level cancerogenic substance in existence and the main driving force behind the cancer epidemic. I already wrote about the correlation between high-protein diets and autophagy so I won’t go into details here. You can read correlated articles.
Stressing our organs and creating acidity and inflammation is a separate problem of protein-rich diets. The number one problem is that this diet is not congruent with our evolution. Constant hunger is congruent with our evolution and scarcity of amino acids. What this means is that our body would not repair damaged cells as long as there is a high protein in the diet.
In evolutionary terms, anthropologists have proven that hominins lived on an average of 15 to 25 grams of protein a day. In the modern Western type of diet, we would consume that amount for breakfast only. And the consequence is a complete shutdown of autophagy.
When we eat too much protein especially if the protein is “high quality” protein from animal origin with high levels of essential amino acids our body will excrete the IGF-1 hormone. What IGF-1 does is bind to receptors in the cells and give a signal to the cells that there are amino acids in the blood. This is a signal for cell division. In normal cells, it would do much but in cancer cells, it would ignite a rapid division. Even worse than this if there is such a thing, is that if there are already damaged cells they won’t be destroyed as long as there is a high level of IGF-1.
Our body would not cannibalize precancerous and mutated cells if there is a higher level of IGF-1 in the blood. Our body learned through evolution that famine is around the corner and to preserve nutrition it would leave all of the cells for later use. In times of fasting, only then, autophagy will be triggered. How this works, in reality, is that If there is one damaged cell and one normal cell and some of the cells need to go to energy, first on the line to be destroyed are the damaged cells. But if there is a high-quality protein and constant eating autophagy will never going to happen. This leads to accumulations of DNA damage in time. These mutations are correlated to a wide range of diseases, not just cancer.
High protein diet correlation to cancer is unbreakable and I have to say I am sorry but it is not even a subject for debate. It is one of the main reasons for the cancer epidemic.
Molecular mimicry.
Did you know that identical twins rarely manifest the same autoimmune disease?
Autoimmune diseases have nothing to do with genetics. Molecular mimicry provides an explanation for the documented epidemiologic evidence that microbial and/or viral infections often precede autoimmune disorders. Also, some autoimmune diseases are a consequence of the consumption of “high quality” protein from animal origin.
I won’t go into a high-depth analysis here. There are correlated articles you can read about this topic. The most simplistic explanation is this.
Humans are herbivores species like any other primate species on this planet. The difference between omnivores and herbivores in one aspect is a biological resistance to meat putrefying bacteria known as resistance filter. This means that if an animal eats meat that meat comes with putrefying bacteria. These bacteria species will not just eat rotting flesh but live flesh as well. Our meat is on the menu too. Bacteria are very specialist species in the type of energy they are able to consume. One eats meat other ferments fiber and all of them are not probiotic. That is a reason why more than 80 percent of our immune system or more than 80 percent of lymph nodes are in our gut. A network is known as GALT, gut-associated lymphoid tissue. Bacteria that ferment fiber are not going to hurt us. These types of bacteria are unable to do us any harm. So all talk about probiotics and gut microbiota is because we consume meat and other animal products and that feeds evil bacteria that putrefy corpses. The way true omnivores and carnivores deal with this is that they have very short transit time and very short colon. Omnivores in their colon do not ferment anything and basically, just dehydrate the remains of digestion before they empty everything. We and other herbivores extract energy from fermentation and we have long colons with long transit times. Also, true omnivore species have very high resistance filter. This means their upper digestive system is basically sterile.
They have an enormous ability to excrete stomach acids so much so that they can eat rotting flesh with no problem. Carnivores and true omnivores are able to digest not just bones but metal as well. The reason we can eat animal products is because we use thermal energy or fire to kill off all bacteria before we eat. It is the reason why it is mandatory by law to have everything pasteurized. We have to have pasteurization because we are not omnivores but herbivores species that use technology. But even if we are able to consume meat by hating it that still does not mean we are able to digest it properly.
Because we have low acid levels we might end up with some undigested proteins in our bloodstream.
When protein gets destroyed by acid the only thing that is left is individual amino acids. But in some cases where protein is not digested completely due to low acid levels, these amino acids can go through the intestinal lining into the bloodstream. If we have leaky gut or Crone disease or inflammation in the gut due to food allergies or infections undigested protein will end up in the blood.
When this happens our immune system doesn’t know that this chain of amino acids is just an undigested protein. It might also be a foreign invader. When there is more than one individual amino acid floating in the blood our immune system creates antibodies to that sequence of amino acids. If the sequence of amino acids is the same as the sequence of amino acids in some of our living cells the horror of never-treatable autoimmune disease is born.
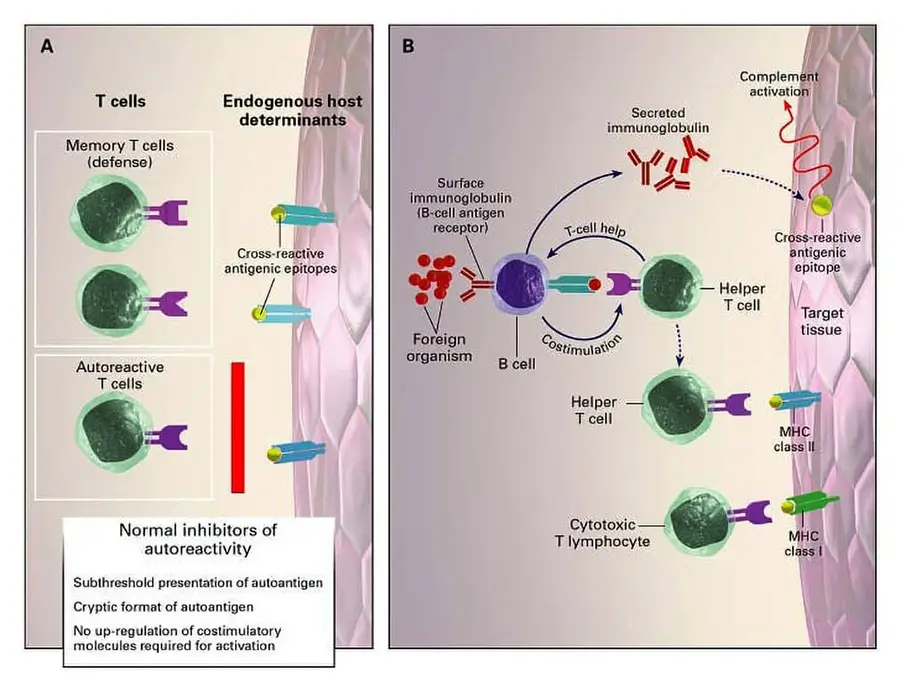
This is especially problematic if we consume flesh because in some sense all flesh is the same to some extent. We don’t have to eat human flesh to get an autoimmune disease. Plant proteins have very different amino acids profile and even if we have some of the undigested proteins that are leaked into the bloodstream the chances of developing autoimmune conditions are low. But with animal protein, the chance is much higher. A good example would be the consumption of A1 beta-casein milk from a standard European cow that has the same amino acid sequence as insulin-producing beta cells in the pancreas.

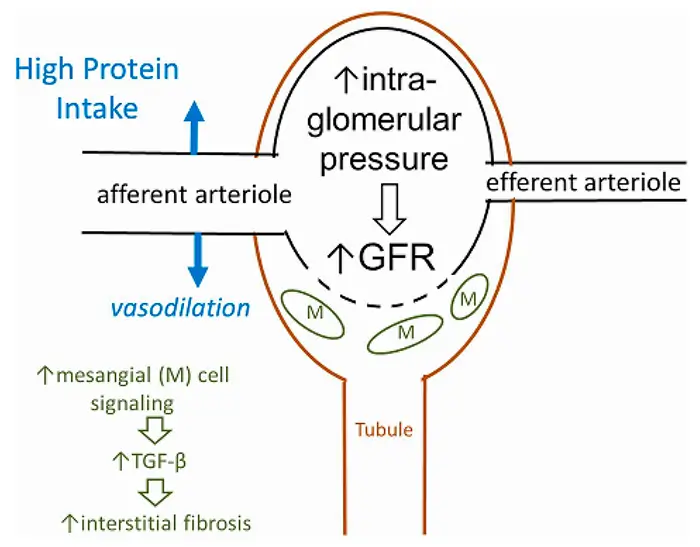
Kidney problems.
Even back in 1928, it was noted in a frog model that amino acids could increase blood flow to the kidneys (Watzadse, 1928). When we talk about excess protein and possible renal damage it has a hundred years of history. It is not a topic that a local gym guru is capable of debunking. And it is not just in frogs.
Following studies in mammalian species like rats and dogs also had similar findings (O’Connor & Summerill, 1976), (Hostetter et al., 1986), (Kamper & Strandgaard, 2017). In one study of dogs, the increase in the GFR (a marker of hyperfiltration) was dose-dependent with meat consumption. The maximum increase reached nearly 80% (MOUSTGAARD, 1947). Even in carnivorous species like dogs, this stressing of the kidneys happens. What it would do then to herbivores species that never had a protein-rich diet like in the case of primates including humans?
Human data and this is accepted science it is just not talked about too much outside of medical circles, also shows hyperfiltration with high protein consumption (Kamper & Strandgaard, 2017). There is a correlation between steroid users and bodybuilders that traditionally consume more than 200 grams of protein per day that had died from or have renal complications. It is one of the things that bodybuilders have a risk of, that comes with a lifestyle, but don’t usually talk about much outside of the community, especially because there are steroids that are acutely toxic to renal cells like Boldenone (Equipoise) (Bodybuilding With Steroids Damages Kidneys, 2009), (Almukhtar et al., 2015).

The largest short-term (<6 months) trial that I was able to find showed that a high-protein diet (this means that protein is comprising no less than 25% of calories) had increased nephrotoxicity after just 6 weeks (rise in GFR) compared with a lower protein diet. It takes less than two months of a high-protein diet to show nephrotoxicity in people with no preexisting renal conditions. A low-protein diet is defined as a diet that has a maximum of 15% of calories from protein sources (Kalantar-Zadeh et al., 2020), (Knight et al., 2003). In the early stages, glomerular hyperfiltration occurs as a rise in GFR but that in time leads to a loss of kidney function. It starts as acute stress that if continued leads to permanent damage.
Unlike liver cells, kidneys are unable to regenerate. Once damaged it is permanent damage for an entire lifetime.
That is a reason why you don’t want to even think about stressing your kidneys, net ever, not even once. You are playing with a permanent disability. Even worse if you already had a problem then this loss of kidney function is particularly pronounced. In those people with underlying chronic kidney disease or at risk for chronic kidney disease loss of kidney function is particularly pronounced (Kalantar-Zadeh et al., 2020).
For a long time, this was just a taboo topic even mentioning it to people that have standard high-protein diets was met with ridicule especially because there are studies that did not show any correlations. Even when proven today by long-term observational studies and placebo-controlled trials it is still not accepted in some of the medical circles and in the general public because again there were studies that did not show a correlation. It takes a couple of studies to serve as an excuse for the entire industry to be able to ignore all of the rest of the science. End result is that talking about this topic is just ignored.
By now there are hundreds of long-term observational studies done in humans and all of them have shown an association between the consumption of high-protein diets and kidney function decline.
This is not just in people with existing or preexisting chronic kidney disease but in all individuals. Two of the big ones would be the Gubbio Population Study and the Nurses’ Health Study (Knight et al., 2003), (Cirillo et al., 2014). Nurses’ Health Study lasted for 11 years and was an observational study. In Nurse’s study for women experiencing mild renal insufficiency, every 10-g increase in protein intake was significantly associated with a significant change in renal markers which was not observed in the population with normal renal function.
Gubbio study was a population-based study of 1522 participants aged 45–64 years (Cirillo et al., 2014). Higher protein intake was associated with lower renal function after 12 years, including among participants with or without preexisting chronic kidney disease.
Other long-term observational studies have found a similar association between high protein intake with a decline in kidney function. Recently one big Iranian study of 1800 people that lasted for 6 years showed that those consuming excess protein in the form of a low-carbohydrate, high-protein diet also had a higher risk of chronic kidney disease (Farhadnejad et al., 2019).
This is still a big problem to get accepted because there are again studies that have shown no effect of high protein diets on kidney function. And the industry loves those.
There is a possible explanation for why that is. This is my personal view as well. The insignificant effects observed in some of the long-term studies may be credited to the counterbalancing effects of hyperfiltration (an increase in renal function) and kidney damage from hyperfiltration (a decrease in renal function). This is a little tricky to understand if you do not have a scientific background.
For example, a randomized clinical trial of participants who have been prescribed the Atkins diet (protein content of around 30% of total energy intake) versus a control diet (protein content of around 15% of total energy intake) for 12 months reported a rise in creatinine clearance among participants in the Atkins diet arm, suggesting hyperfiltration (Cirillo et al., 2014).
However, the differences in creatinine clearance between the Atkins versus control diet groups were attenuated after 24 months of observation, which may indicate that the short-term rise in GFR with high protein intake may be followed by a decline in GFR over time, possibly as a result of renal injury (Cirillo et al., 2014).
Hyperfiltration may also lead to an increased risk of proteinuria. Proteinuria is the presence of excess proteins in the urine.
If you have elevated protein in the urine it is not a good indicator of renal function. There is a long line of different studies that have shown a link between high protein intake and increased proteinuria and/or albuminuria as an early indicator of kidney damage. Several observational studies have also demonstrated an increased risk of elevated protein in the urine with high dietary protein intake even when corrected for other health markers like smoking, physical activity, and medication use (Møller et al., 2018), (Almeida et al., 2008), (Lin et al., 2011), (Lin et al., 2010). However, again there are some studies that did not observe an association in healthy individuals but only in people with diabetes and hypertension. There are long-term studies that also did not show a correlation as well and the effect of a high-protein diet on proteinuria still needs further investigation in long-term trials.
But wait what if you have diabetes or prediabetes or higher blood pressure and eat the standard 80 grams of protein standard Western diet?
In these situations, the certified dietitian will most centrally limit your protein intake or he or she would risk a lawsuit. All talk about the magic properties of protein and all of the propaganda goes out of the window when there is a real possibility for you to end up in a court of law. The glory of protein is only preached on the internet and in lifestyle magazines until you end up with a disability.
One consequence of a diet rich in proteins that is always present is increases in kidney volume and weight in humans (Skov et al., 1999). This is not debatable. What is debatable is does this increase in size leads to some form of permanent damage and if it does to what extent.
Why this increase in size is happening is not truly understood yet. There are some speculations. One of the theories is that it is an evolutionary feedback mechanism facilitating the excretion of increased amounts of protein-derived nitrogenous waste. Other theories are that it is induced by the rising of glucagon and IGF-1 which would lead to vasodilation or even a neurohormonal response within the kidney (Kalantar-Zadeh et al., 2017).
Protein comes with baggage.
Protein is not just protein. It is one nutrient from many nutrients that comes along as a package meal. To have a high-protein diet we would have to eat food items that have high levels of protein meaning flesh, eggs, and milk… and as a consequence, we will consume much more than just protein.
With protein comes cholesterol, saturated fat, environmental toxins…
Eating low-fat chicken breast and fish would not help you. Actually, the most inflammation-causing meat is number one fish, number two chicken. Two of the “healthy” meat sources. This is a very complex subject and it would be analyzed in correlated articles.
Don’t get me wrong protein by itself without any baggage even if we eat pure protein from plant-based sources will increase inflammation and acidity but not to the same extent.
Studies have demonstrated that when compared with the intake of plant protein, the intake of animal protein causes an imbalance in the composition of the gut microbiome in addition to all processes already mentioned by producing more ammonia and sulfur-based materials and having a pro-inflammatory profile. Inflammation is correlated to basically all known chronic diseases and especially is dangerous to people with reduced kidney function and an increased risk of cardiovascular disease (Tomova et al., 2019), (Mafra et al., 2018), (Barros et al., 2015), (Black et al., 2018). Finally, high meat intake has been associated with an increase in inflammation and oxidative stress, including upregulated inflammatory mediators such as NF-κB and inflammatory cytokines (Derry et al., 2013)[35], (Montonen, Jukka et al., 2013).
These differences between the effects of animal-based protein versus plant-based protein may favor the use of the latter but again high protein diet is not desirable regardless of the protein source.
If we disregard inflammation that is subject to itself and we just look at acidity, the body would need to use minerals to buffer that excess acidity. However, recent findings suggest the effect of protein on bone health remains uncorrelated because the body would just use more of the calcium from the food.
However, If you eat nothing but an inflammation-promoting diet and don’t have an adequate intake of antioxidants, this pro-inflammatory metabolic effect can have a correlation to overall health. Also if you have any medical condition affecting any of the internal organs that are involved with nitrogen metabolisms such as kidney failure, liver disease, diabetes, cancer, or medical conditions that need close monitoring of protein intake, the amount of protein in your diet needs to be monitored by a certified dietitian. This means that if you consume the standard amount of 80 grams of protein a day or 1 gram per kg that somehow became a recommended phantasy, you are oversteering your kidneys.
One gram per kilo was the amount that the industry calculated would have no impact on any form of meaningful dietary change in the overall population. That one gram then became a “recommendation” that is pushed in every lifestyle magazine and every M.D. office.
Only if you have or when you develop a medical condition that is correlated with excessive protein consumption that number is lowered to a more normal value by certified dietitians. If dietary recommendations promote lowering protein intake that automatically means promoting a more plant-based diet and that is something that never is going to happen. Not now, not ever, as long as there is industry and deep state around. They might be concerned about excessive nitrogen pollution in U.S. waters as pee problem pollution from protein-rich diets.
How much protein are we able to consume?
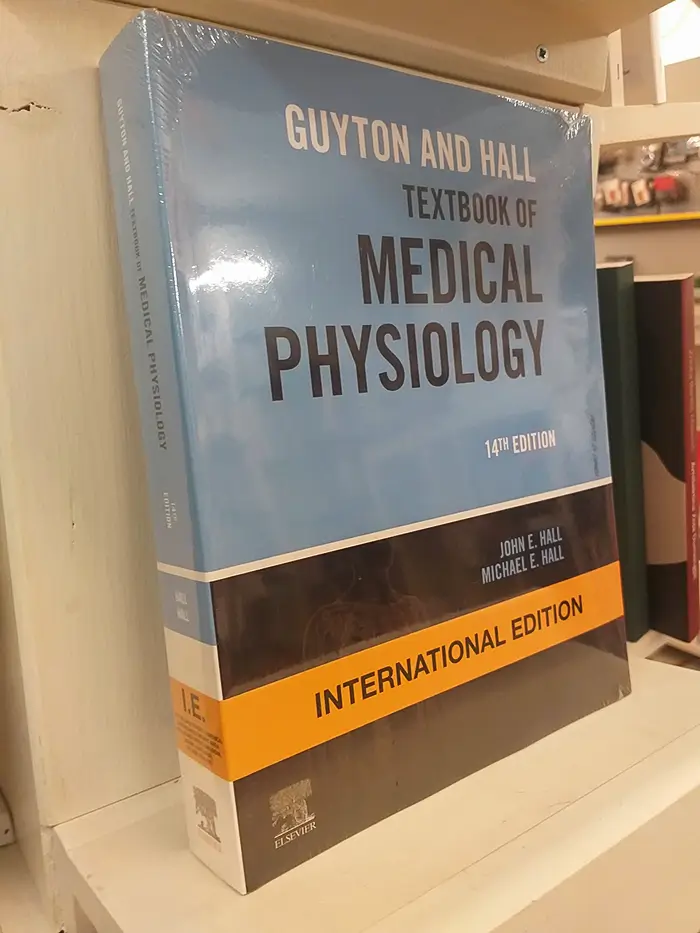
The most used textbook for students and in other areas of human physiology is Guyton and Hall’s Textbook of Medical Physiology. When describing the obligatory use of protein, even there they say from 25 to 35 grams of protein a day just to stay even. And that is when you eat three times a day and don do a diet. If you are on a diet obligatory, (just to stay even) amount of protein you need can come close to zero. But why do you need obligatory 25 grams of protein according to the book?
In medical practice, meaning for population scale recommendation it was estimated that the average requirement for protein intake is 0.6 g of protein per kilogram of ideal body weight per day. This is on a population scale, which corresponds to the amount of protein required to avoid a negative nitrogen balance for half of a population. Now, this is currently accepted medical recommendation. The key in this sentence is per kilogram of ideal body weight. And what is ideal body weight? Let’s say you are a man that weighs 70kg and you are considered a normal man that is not overweight your protein requirement is 70kg multiplied by 0.6g, to reach 42grams of protein in a day.
If you gain 15 more kilograms what would be your new protein requirement?
It is still 42. You just gain fat, nothing else, you are not at your ideal body weight anymore and this calculation of 0.6 grams of protein per kilogram doesn’t apply anymore. Actually even that 70kg male probably does not have visible abdominal muscles. When you have 6-pack abs you are at your ideal weight. That is conditioning congruent with human evolution.
That 70kg man would probably still be able to lose some of the weight to get 6-pack abs to let’s say 65kg ideal weight with a protein requirement of less than 40 grams per day. And if you are a woman your requirement would be 35 grams. And this is also too excessive as a recommendation but it is a recommendation as high as the industry could get away with.
The recommended daily allowance, for protein intake, is 0.83 g/kg per day and is calculated to meet the requirements of 97%–98% of the population (World Health Organization, 2007c). And this is how the statistic is used to trick you. This recommendation is not a recommendation that is “recommended” or optimal for you. It is a recommendation that is calculated to meet the requirements entire population and this includes, for example, breastfeeding babies and young children.
And this is how 1 gram per kilo turns into a marketing trick. That man that used to have 65kg six-pack abs now is at 85kg with a “recommended” protein intake of 90 grams per day. This is how industry with their MDs trick people without “breaking” the science. And then they will even go one step further and will put ideas of incomplete protein sources and high-quality protein sources and complementary proteins into your subconscious mind.

And where did we end up because of this? Data from the National Health and Nutrition Examination Survey (NHANES) showed that the current average consumption of protein in the United States is estimated to be approximately 1.2-1.4 g/kg per day (Moore et al., 2013). And this is per kg of weight, not ideal weight. By now, because you are learning about nutrition, you should understand what this means. And if you really want to lose weight or join the gym, then you would need even higher amounts of protein while restricting the number of carbohydrates. In other words, Atkins or keto meat-dominated diets. And if I, as a nutritionist, say to you that all of them are lying to you and that restricting carbohydrates has nothing to do with losing weight and that in real science, we consider the keto diet as a marketing trick to make money, then what? Most people start talking about studies that, in reality, are all based on the assumption that all carbohydrates are undesirable. The assumption has been refuted in the literature not once or twice or by plain observational statistics (for example, rural vegan starch-dominated diets in Asia) but for decades now (Joshi et al., 2019), and the industry is still pushing this agenda.
While the ketogenic diet has received ample funding and backing from the industry with claims that it would help treat obesity and type 2 diabetes, evidence that it actually offers such benefits is nonexistent; quite the opposite. Long-term randomized trials have failed to show a clinically significant benefit over comparator diets, and this is accepted science, not my personal opinion (Joshi et al., 2019). Actually, because this is basically a carnivore diet that your cat might be thriving upon, we as primates that are herbivorous, with this type of diet will have worsening health effects.
The only question is, is this type of diet better than the processed food standard Western diet? In this comparison, it is better because basically, nothing can be worse than a sugar and fat-nutrition-deprived, processed food diet, even keto.
But as a diet, it is an evolutionary non-congruent diet that is not without consequence: it may produce adverse effects in the average dieter, such as hyperlipidemia, vitamin and mineral deficiencies, and fatigue. For patients with or at high risk for kidney disease, the ketogenic diet is absolutely forbidden.
A ketogenic diet is basically a carnivore diet that restricts the intake of carbohydrates as an energy source. Carnivores don’t have enzymes for the digestion of carbohydrates, unlike humans. Instead, the emphasis is on the use of fat as an energy source, resulting in the production of ketones. The name comes from ketones. It is also a high-protein diet with 1.2–2.0 g/kg of protein per day. This type of diet is absolutely forbidden for patients that have kidney disease and will accelerate the progression of their kidney disease (Kasiske et al., 1998).
Of equal concern for those without CKD is the high amount of fat in the ketogenic diet. Lipotoxicity is correlated to diabetes, and high cholesterol is correlated to cardiovascular disease, as well as high saturated fat intake. Personally, if I wanted to create a diet that would shorten someone’s lifespan, I would choose a standard Western processed food-dominated diet as number one, and keto as number two.
High-protein diets should be avoided, if possible in all situations.
Given the rise in popularity of high-protein diets as an alternative to the standard American diet and the high prevalence of chronic diseases in the United States and the rest of the developed world and all of the propaganda behind it, I personally don’t see a bright future in regard to health and prevalence of chronic diseases.
Dr. Tel Oren (MD): The Truth about Protein. Talk at the 2011 World Vegetarian Festival Weekend in San Francisco California sponsored by the San Francisco Vegetarian Society.
FAQ
References:
Passages selected from a book: Pokimica, Milos. Go Vegan? Review of Science Part 3. Kindle ed., Amazon, 2020.
- Watzadse, G. (1928). Über die Harnbildung in der Froschniere. Pflügers Archiv: European Journal of Physiology, 219(1), 694–705. https://doi.org/10.1007/bf01723451
- Ko, G. J., Obi, Y., Tortorici, A. R., & Kalantar-Zadeh, K. (2017). Dietary protein intake and chronic kidney disease. Current opinion in clinical nutrition and metabolic care, 20(1), 77–85. https://doi.org/10.1097/MCO.0000000000000342
- World Health Organization. (2007b). Protein and amino acid requirements in human nutrition : report of a joint FAO/WHO/UNU expert consultation. https://apps.who.int/iris/handle/10665/43411
- Moore, L. W., Byham-Gray, L. D., Scott Parrott, J., Rigassio-Radler, D., Mandayam, S., Jones, S. L., Mitch, W. E., & Osama Gaber, A. (2013). The mean dietary protein intake at different stages of chronic kidney disease is higher than current guidelines. Kidney international, 83(4), 724–732. https://doi.org/10.1038/ki.2012.420
- Joshi, S., Ostfeld, R. J., & McMacken, M. (2019). The Ketogenic Diet for Obesity and Diabetes-Enthusiasm Outpaces Evidence. JAMA internal medicine, 179(9), 1163–1164. https://doi.org/10.1001/jamainternmed.2019.2633
- O’Connor, W. J., & Summerill, R. A. (1976). The effect of a meal of meat on glomerular filtration rate in dogs at normal urine flows. The Journal of physiology, 256(1), 81–91. https://doi.org/10.1113/jphysiol.1976.sp011312
- Hostetter, T. H., Meyer, T. W., Rennke, H. G., & Brenner, B. M. (1986). Chronic effects of dietary protein in the rat with intact and reduced renal mass. Kidney international, 30(4), 509–517. https://doi.org/10.1038/ki.1986.215
- Kamper, A. L., & Strandgaard, S. (2017). Long-Term Effects of High-Protein Diets on Renal Function. Annual review of nutrition, 37, 347–369. https://doi.org/10.1146/annurev-nutr-071714-034426
- MOUSTGAARD J. (1947). Variation of the renal function in normal and unilaterally nephrectomized dogs. American journal of veterinary research, 8(28), 301–306. [PubMed]
- Juraschek, S. P., Appel, L. J., Anderson, C. A., & Miller, E. R., 3rd (2013). Effect of a high-protein diet on kidney function in healthy adults: results from the OmniHeart trial. American journal of kidney diseases : the official journal of the National Kidney Foundation, 61(4), 547–554. https://doi.org/10.1053/j.ajkd.2012.10.017
- Kamper, A. L., & Strandgaard, S. (2017). Long-Term Effects of High-Protein Diets on Renal Function. Annual review of nutrition, 37, 347–369. https://doi.org/10.1146/annurev-nutr-071714-034426
- Bodybuilding With Steroids Damages Kidneys. (2009, October 9). ScienceDaily. https://www.sciencedaily.com/releases/2009/10/091029141202.htm
- Almukhtar, S. E., Abbas, A. A., Muhealdeen, D. N., & Hughson, M. D. (2015). Acute kidney injury associated with androgenic steroids and nutritional supplements in bodybuilders. Clinical Kidney Journal, 8(4), 415-419. https://doi.org/10.1093/ckj/sfv032
- Kalantar-Zadeh, K., Kramer, H. M., & Fouque, D. (2020). High-protein diet is bad for kidney health: unleashing the taboo. Nephrology, dialysis, transplantation : official publication of the European Dialysis and Transplant Association – European Renal Association, 35(1), 1–4. https://doi.org/10.1093/ndt/gfz216
- Knight, E. L., Stampfer, M. J., Hankinson, S. E., Spiegelman, D., & Curhan, G. C. (2003). The impact of protein intake on renal function decline in women with normal renal function or mild renal insufficiency. Annals of internal medicine, 138(6), 460–467. https://doi.org/10.7326/0003-4819-138-6-200303180-00009
- Cirillo, M., Lombardi, C., Chiricone, D., De Santo, N. G., Zanchetti, A., & Bilancio, G. (2014). Protein intake and kidney function in the middle-age population: contrast between cross-sectional and longitudinal data. Nephrology, dialysis, transplantation : official publication of the European Dialysis and Transplant Association – European Renal Association, 29(9), 1733–1740. https://doi.org/10.1093/ndt/gfu056
- Farhadnejad, H., Asghari, G., Emamat, H., Mirmiran, P., & Azizi, F. (2019). Low-Carbohydrate High-Protein Diet is Associated With Increased Risk of Incident Chronic Kidney Diseases Among Tehranian Adults. Journal of renal nutrition : the official journal of the Council on Renal Nutrition of the National Kidney Foundation, 29(4), 343–349. https://doi.org/10.1053/j.jrn.2018.10.007
- Cirillo, M., Lombardi, C., Chiricone, D., De Santo, N. G., Zanchetti, A., & Bilancio, G. (2014). Protein intake and kidney function in the middle-age population: contrast between cross-sectional and longitudinal data. Nephrology, dialysis, transplantation : official publication of the European Dialysis and Transplant Association – European Renal Association, 29(9), 1733–1740. https://doi.org/10.1093/ndt/gfu056
- Friedman, A. N., Ogden, L. G., Foster, G. D., Klein, S., Stein, R., Miller, B., Hill, J. O., Brill, C., Bailer, B., Rosenbaum, D. R., & Wyatt, H. R. (2012). Comparative effects of low-carbohydrate high-protein versus low-fat diets on the kidney. Clinical journal of the American Society of Nephrology : CJASN, 7(7), 1103–1111. https://doi.org/10.2215/CJN.11741111
- Møller, G., Rikardt Andersen, J., Ritz, C., P Silvestre, M., Navas-Carretero, S., Jalo, E., Christensen, P., Simpson, E., Taylor, M., Martinez, J. A., Macdonald, I., Swindell, N., Mackintosh, K. A., Stratton, G., Fogelholm, M., Larsen, T. M., Poppitt, S. D., Dragsted, L. O., & Raben, A. (2018). Higher Protein Intake Is Not Associated with Decreased Kidney Function in Pre-Diabetic Older Adults Following a One-Year Intervention-A Preview Sub-Study. Nutrients, 10(1), 54. https://doi.org/10.3390/nu10010054
- Almeida, J. C., Zelmanovitz, T., Vaz, J. S., Steemburgo, T., Perassolo, M. S., Gross, J. L., & Azevedo, M. J. (2008). Sources of protein and polyunsaturated fatty acids of the diet and microalbuminuria in type 2 diabetes mellitus. Journal of the American College of Nutrition, 27(5), 528–537. https://doi.org/10.1080/07315724.2008.10719735
- Lin, J., Fung, T. T., Hu, F. B., & Curhan, G. C. (2011). Association of dietary patterns with albuminuria and kidney function decline in older white women: a subgroup analysis from the Nurses’ Health Study. American journal of kidney diseases : the official journal of the National Kidney Foundation, 57(2), 245–254. https://doi.org/10.1053/j.ajkd.2010.09.027
- Lin, J., Hu, F. B., & Curhan, G. C. (2010). Associations of diet with albuminuria and kidney function decline. Clinical journal of the American Society of Nephrology : CJASN, 5(5), 836–843. https://doi.org/10.2215/CJN.08001109
- Skov, A. R., Toubro, S., Bülow, J., Krabbe, K., Parving, H. H., & Astrup, A. (1999). Changes in renal function during weight loss induced by high vs low-protein low-fat diets in overweight subjects. International journal of obesity and related metabolic disorders : journal of the International Association for the Study of Obesity, 23(11), 1170–1177. https://doi.org/10.1038/sj.ijo.0801048
- Kalantar-Zadeh, K., & Fouque, D. (2017). Nutritional Management of Chronic Kidney Disease. The New England journal of medicine, 377(18), 1765–1776. https://doi.org/10.1056/NEJMra1700312
- Frank, Helga et al. “Effect of short-term high-protein compared with normal-protein diets on renal hemodynamics and associated variables in healthy young men.” The American journal of clinical nutrition vol. 90,6 (2009): 1509-16. doi:10.3945/ajcn.2009.27601
- Weiner, I. D., Mitch, W. E., & Sands, J. M. (2015). Urea and Ammonia Metabolism and the Control of Renal Nitrogen Excretion. Clinical journal of the American Society of Nephrology : CJASN, 10(8), 1444–1458. https://doi.org/10.2215/CJN.10311013
- Wesson, D. E., Buysse, J. M., & Bushinsky, D. A. (2020). Mechanisms of Metabolic Acidosis-Induced Kidney Injury in Chronic Kidney Disease. Journal of the American Society of Nephrology : JASN, 31(3), 469–482. https://doi.org/10.1681/ASN.2019070677
- Lennon, E. J., J Lemann, J., & Litzow, J. R. (1966). The effects of diet and stool composition on the net external acid balance of normal subjects. Journal of Clinical Investigation, 45(10), 1601-1607. https://doi.org/10.1172/JCI105466
- Scialla, J. J., & Anderson, C. A. (2013). Dietary acid load: a novel nutritional target in chronic kidney disease?. Advances in chronic kidney disease, 20(2), 141–149. https://doi.org/10.1053/j.ackd.2012.11.001
- Tomova, A., Bukovsky, I., Rembert, E., Yonas, W., Alwarith, J., Barnard, N. D., & Kahleova, H. (2019). The Effects of Vegetarian and Vegan Diets on Gut Microbiota. Frontiers in nutrition, 6, 47. https://doi.org/10.3389/fnut.2019.00047
- Mafra, D., Borges, N. A., Cardozo, L. F. M. F., Anjos, J. S., Black, A. P., Moraes, C., Bergman, P., Lindholm, B., & Stenvinkel, P. (2018). Red meat intake in chronic kidney disease patients: Two sides of the coin. Nutrition (Burbank, Los Angeles County, Calif.), 46, 26–32. https://doi.org/10.1016/j.nut.2017.08.015
- Barros, A. F., Borges, N. A., Ferreira, D. C., Carmo, F. L., Rosado, A. S., Fouque, D., & Mafra, D. (2015). Is there interaction between gut microbial profile and cardiovascular risk in chronic kidney disease patients?. Future microbiology, 10(4), 517–526. https://doi.org/10.2217/fmb.14.140
- Black, A. P., Anjos, J. S., Cardozo, L., Carmo, F. L., Dolenga, C. J., Nakao, L. S., de Carvalho Ferreira, D., Rosado, A., Carraro Eduardo, J. C., & Mafra, D. (2018). Does Low-Protein Diet Influence the Uremic Toxin Serum Levels From the Gut Microbiota in Nondialysis Chronic Kidney Disease Patients?. Journal of renal nutrition : the official journal of the Council on Renal Nutrition of the National Kidney Foundation, 28(3), 208–214. https://doi.org/10.1053/j.jrn.2017.11.007
- Derry, M. M., Raina, K., Agarwal, C., & Agarwal, R. (2013). Identifying molecular targets of lifestyle modifications in colon cancer prevention. Frontiers in oncology, 3, 119. https://doi.org/10.3389/fonc.2013.00119
- Montonen, J., Boeing, H., Fritsche, A., Schleicher, E., Joost, H. G., Schulze, M. B., Steffen, A., & Pischon, T. (2013). Consumption of red meat and whole-grain bread in relation to biomarkers of obesity, inflammation, glucose metabolism and oxidative stress. European journal of nutrition, 52(1), 337–345. https://doi.org/10.1007/s00394-012-0340-6
- Kasiske, B. L., Lakatua, J. D., Ma, J. Z., & Louis, T. A. (1998). A meta-analysis of the effects of dietary protein restriction on the rate of decline in renal function. American journal of kidney diseases : the official journal of the National Kidney Foundation, 31(6), 954–961. https://doi.org/10.1053/ajkd.1998.v31.pm9631839
Related Posts
Do you have any questions about nutrition and health?
I would love to hear from you and answer them in my next post. I appreciate your input and opinion and I look forward to hearing from you soon. I also invite you to follow us on Facebook, Instagram, and Pinterest for more diet, nutrition, and health content. You can leave a comment there and connect with other health enthusiasts, share your tips and experiences, and get support and encouragement from our team and community.
I hope that this post was informative and enjoyable for you and that you are prepared to apply the insights you learned. If you found this post helpful, please share it with your friends and family who might also benefit from it. You never know who might need some guidance and support on their health journey.
– You Might Also Like –

Learn About Nutrition
Milos Pokimica is a doctor of natural medicine, clinical nutritionist, medical health and nutrition writer, and nutritional science advisor. Author of the book series Go Vegan? Review of Science, he also operates the natural health website GoVeganWay.com
Medical Disclaimer
GoVeganWay.com brings you reviews of the latest nutrition and health-related research. The information provided represents the personal opinion of the author and is not intended nor implied to be a substitute for professional medical advice, diagnosis, or treatment. The information provided is for informational purposes only and is not intended to serve as a substitute for the consultation, diagnosis, and/or medical treatment of a qualified physician or healthcare provider.NEVER DISREGARD PROFESSIONAL MEDICAL ADVICE OR DELAY SEEKING MEDICAL TREATMENT BECAUSE OF SOMETHING YOU HAVE READ ON OR ACCESSED THROUGH GoVeganWay.com
NEVER APPLY ANY LIFESTYLE CHANGES OR ANY CHANGES AT ALL AS A CONSEQUENCE OF SOMETHING YOU HAVE READ IN GoVeganWay.com BEFORE CONSULTING LICENCED MEDICAL PRACTITIONER.
In the event of a medical emergency, call a doctor or 911 immediately. GoVeganWay.com does not recommend or endorse any specific groups, organizations, tests, physicians, products, procedures, opinions, or other information that may be mentioned inside.
Editor Picks –
Milos Pokimica is a health and nutrition writer and nutritional science advisor. Author of the book series Go Vegan? Review of Science, he also operates the natural health website GoVeganWay.com
Latest Articles –
Top Health News — ScienceDaily
- The overlooked nutrition risk of Ozempic and Wegovyon February 4, 2026
Popular weight-loss drugs like Ozempic and Wegovy can dramatically curb appetite, but experts warn many users are flying blind when it comes to nutrition. New research suggests people taking these medications may not be getting enough guidance on protein, vitamins, and overall diet quality, increasing the risk of muscle loss and nutrient deficiencies.
- A 25-year study found an unexpected link between cheese and dementiaon February 4, 2026
A massive Swedish study tracking nearly 28,000 people for 25 years found an unexpected link between full-fat dairy and brain health. Among adults without a genetic risk for Alzheimer’s, eating more full-fat cheese was associated with a noticeably lower risk of developing the disease, while higher cream intake was tied to reduced dementia risk overall. The findings challenge decades of low-fat dietary advice but come with important caveats.
- MIT’s new brain tool could finally explain consciousnesson February 4, 2026
Scientists still don’t know how the brain turns physical activity into thoughts, feelings, and awareness—but a powerful new tool may help crack the mystery. Researchers at MIT are exploring transcranial focused ultrasound, a noninvasive technology that can precisely stimulate deep regions of the brain that were previously off-limits. In a new “roadmap” paper, they explain how this method could finally let scientists test cause-and-effect in consciousness research, not just observe […]
- Why heart disease risk in type 2 diabetes looks different for men and womenon February 4, 2026
Scientists are digging into why heart disease risk in type 2 diabetes differs between men and women—and sex hormones may be part of the story. In a large Johns Hopkins study, men with higher testosterone had lower heart disease risk, while rising estradiol levels were linked to higher risk. These hormone effects were not seen in women. The results point toward more personalized approaches to heart disease prevention in diabetes.
- Sound machines might be making your sleep worseon February 4, 2026
Sound machines may not be the sleep saviors many believe. Researchers found that pink noise significantly reduced REM sleep, while simple earplugs did a better job protecting deep, restorative sleep from traffic noise. When pink noise was combined with outside noise, sleep quality dropped even further. The results suggest that popular “sleep sounds” could be doing more harm than good—particularly for kids.
- This unexpected plant discovery could change how drugs are madeon February 3, 2026
Plants make chemical weapons to protect themselves, and many of these compounds have become vital to human medicine. Researchers found that one powerful plant chemical is produced using a gene that looks surprisingly bacterial. This suggests plants reuse microbial tools to invent new chemistry. The insight could help scientists discover new drugs and produce them more sustainably.
- A hidden cellular process may drive aging and diseaseon February 3, 2026
As we age, our cells don’t just wear down—they reorganize. Researchers found that cells actively remodel a key structure called the endoplasmic reticulum, reducing protein-producing regions while preserving fat-related ones. This process, driven by ER-phagy, is tied to lifespan and healthy aging. Because these changes happen early, they could help trigger later disease—or offer a chance to stop it.
PubMed, #vegan-diet –
- Diet type and the oral microbiomeon February 2, 2026
CONCLUSION: The diet-oral microbiome-systemic inflammation axis is bidirectional and clinically relevant. Understanding both direct ecological regulation and indirect metabolic effects is essential to support precision nutrition strategies aimed at maintaining oral microbial balance and systemic inflammatory risk mitigation.
- Consensus document on healthy lifestyleson January 22, 2026
Proteins are a group of macronutrients that are vital to our lives, as they perform various functions, including structural, defensive and catalytic. An intake of 1.0-1.2 g/kg/body weight per day would be sufficient to meet our needs. Carbohydrate requirements constitute 50 % of the total caloric value and should be obtained mainly in the form of complex carbohydrates. In addition, a daily intake of both soluble and insoluble fiber is necessary. Regular consumption of extra virgin olive oil […]
- Vitamin B12 and D status in long-term vegetarians: Impact of diet duration and subtypes in Beijing, Chinaon January 21, 2026
CONCLUSIONS: This study reveals a dual challenge among Beijing long-term vegetarians: vitamin B12 deficiency was strongly associated with the degree of exclusion of animal products from the diet (veganism), while vitamin D deficiency was highly prevalent and worsened with longer diet duration. The near-universal vitamin D deficiency observed in this study suggests that, in the Beijing context, the risk may extend beyond dietary choice, potentially reflecting regional environmental factors;…
- Nutritional evaluation of duty meals provided to riot police forces in Germanyon January 13, 2026
Background: The primary role of the German riot police is maintaining internal security. Due to challenging working conditions, riot police forces face an elevated risk of various diseases. During duty, forces are provided with meals. A balanced diet can reduce the risk of some of these diseases and contribute to health-promoting working conditions. Aim: First evaluation of the nutritional quality of duty meals in Germany based on German Nutrition Society recommendations (DGE). Methods: In…
- Iodineon January 1, 2006
Iodine is an essential trace nutrient for all infants that is a normal component of breastmilk. Infant requirements are estimated to be 15 mcg/kg daily in full-term infants and 30 mcg/kg daily in preterm infants.[1] Breastmilk iodine concentration correlates well with maternal urinary iodine concentration and may be a useful index of iodine sufficiency in infants under 2 years of age, but there is no clear agreement on a value that indicates iodine sufficiency, and may not correlate with […]
Random Posts –
Featured Posts –
Latest from PubMed, #plant-based diet –
- From paddy soil to dining table: biological biofortification of rice with zincby Lei Huang on February 4, 2026
One-third of paddy soils are globally deficient in zinc (Zn) and 40% of Zn loss in the procession from brown rice to polished rice, which results in the global issue of hidden hunger, e.g., the micronutrient deficiencies in the rice-based population of developing countries. In the recent decades, biofortification of cereal food crops with Zn has emerged as a promising solution. Herein, we comprehensively reviewed the entire process of Zn in paddy soil to human diet, including the regulatory…
- Molecular Characterization of Tobacco Necrosis Virus A Variants Identified in Sugarbeet Rootsby Alyssa Flobinus on February 3, 2026
Sugarbeet provides an important source of sucrose; a stable, environmentally safe, and low-cost staple in the human diet. Viral diseases arising in sugarbeet ultimately impact sugar content, which translates to financial losses for growers. To manage diseases and prevent such losses from occurring, it is essential to characterize viruses responsible for disease. Recently, our laboratory identified a tobacco necrosis virus A variant named Beta vulgaris alphanecrovirus 1 (BvANV-1) in sugarbeet…
- Nutrition in early life interacts with genetic risk to influence preadult behaviour in the Raine Studyby Lars Meinertz Byg on February 3, 2026
CONCLUSIONS: Nutrition in early life and psychiatric genetic risk may interact to determine lasting child behaviour. Contrary to our hypothesis, we find dietary benefits in individuals with lower ADHD PGS, necessitating replication. We also highlight the possibility of including genetics in early nutrition intervention trials for causal inference.
- Effect of the gut microbiota on insect reproduction: mechanisms and biotechnological prospectsby Dilawar Abbas on February 2, 2026
The insect gut microbiota functions as a multifunctional symbiotic system that plays a central role in host reproduction. Through the production of bioactive metabolites, gut microbes interact with host hormonal pathways, immune signaling, and molecular regulatory networks, thereby shaping reproductive physiology and fitness. This review summarizes recent advances in understanding how gut microbiota regulate insect reproduction. Accumulating evidence demonstrates that microbial metabolites…
- Rationale and design of a parallel randomised trial of a plant-based intensive lifestyle intervention for diabetes remission: The REmission of diabetes using a PlAnt-based weight loss InteRvention…by Brighid McKay on February 2, 2026
CONCLUSIONS: This trial will provide high-quality clinical evidence on the use of plant-based ILIs to address the epidemics of obesity and diabetes to inform public health policies and programs in Canada and beyond.
- Diet type and the oral microbiomeby Daniel Betancur on February 2, 2026
CONCLUSION: The diet-oral microbiome-systemic inflammation axis is bidirectional and clinically relevant. Understanding both direct ecological regulation and indirect metabolic effects is essential to support precision nutrition strategies aimed at maintaining oral microbial balance and systemic inflammatory risk mitigation.