Cooked meat bacteria endotoxemia- Inflammation and diet
Are humans omnivores in a true anatomical sense? There is a fundamental difference in the way the digestive tract works in plant vs meat-eating species.
Milos Pokimica
Written By: Milos Pokimica
Medically Reviewed by: Dr. Xiùying Wáng, M.D.
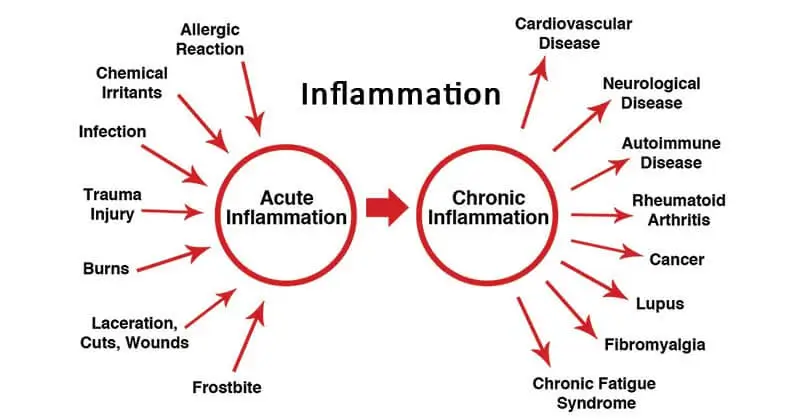
Updated June 9, 2023The emerging role of chronic inflammation in modern society’s major chronic diseases has sparked research into the impact of nutrition and dietary patterns on inflammatory status. The majority of human studies have linked dietary intake to systemic inflammation markers such as high-sensitivity C-reactive protein (HS-CRP), interleukin-6 (IL-6), and tumor necrosis factor-alpha (TNF-).
Significant dietary influences have been established for glycemic index (GI) and load (GL), fiber, fatty acid composition, magnesium, carotenoids, and flavonoids. Whole food plant-based diet or even a traditional Mediterranean dietary pattern, which typically has a high ratio of monounsaturated (MUFA) to saturated (SFA) fats and ω-3 to ω-6 polyunsaturated fatty acid (PUFAs) and supplies an abundance of fruits, vegetables, legumes, and grains, has shown anti-inflammatory effects when compared with typical North American and Northern European dietary patterns in most observational and interventional studies. There is a wide range of factors that influence inflammation caused by diet but a whole food antioxidant-rich, nutrient-rich diet may become the diet of choice for diminishing chronic inflammation in clinical practice.
Prolonged low-grade inflammation is linked to increased oxidative stress and altered glucose and lipid metabolism in fat (adipose) cells, muscle, and the liver. As a result, research indicates that certain dietary components can influence these key inflammatory pathways.
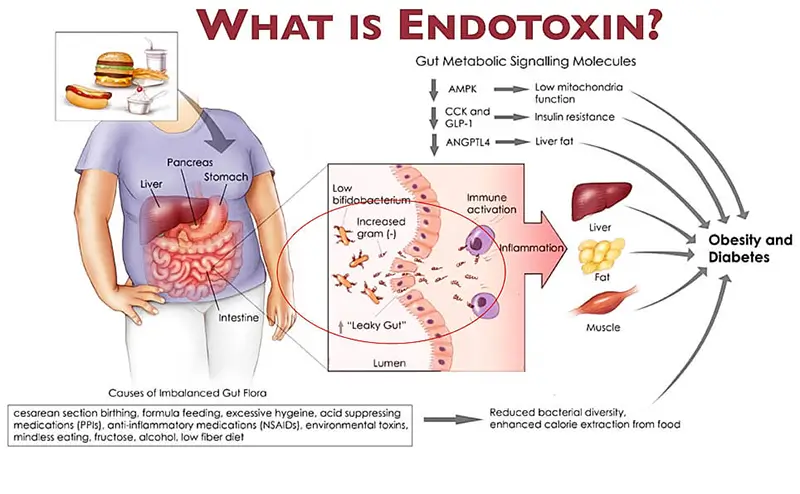
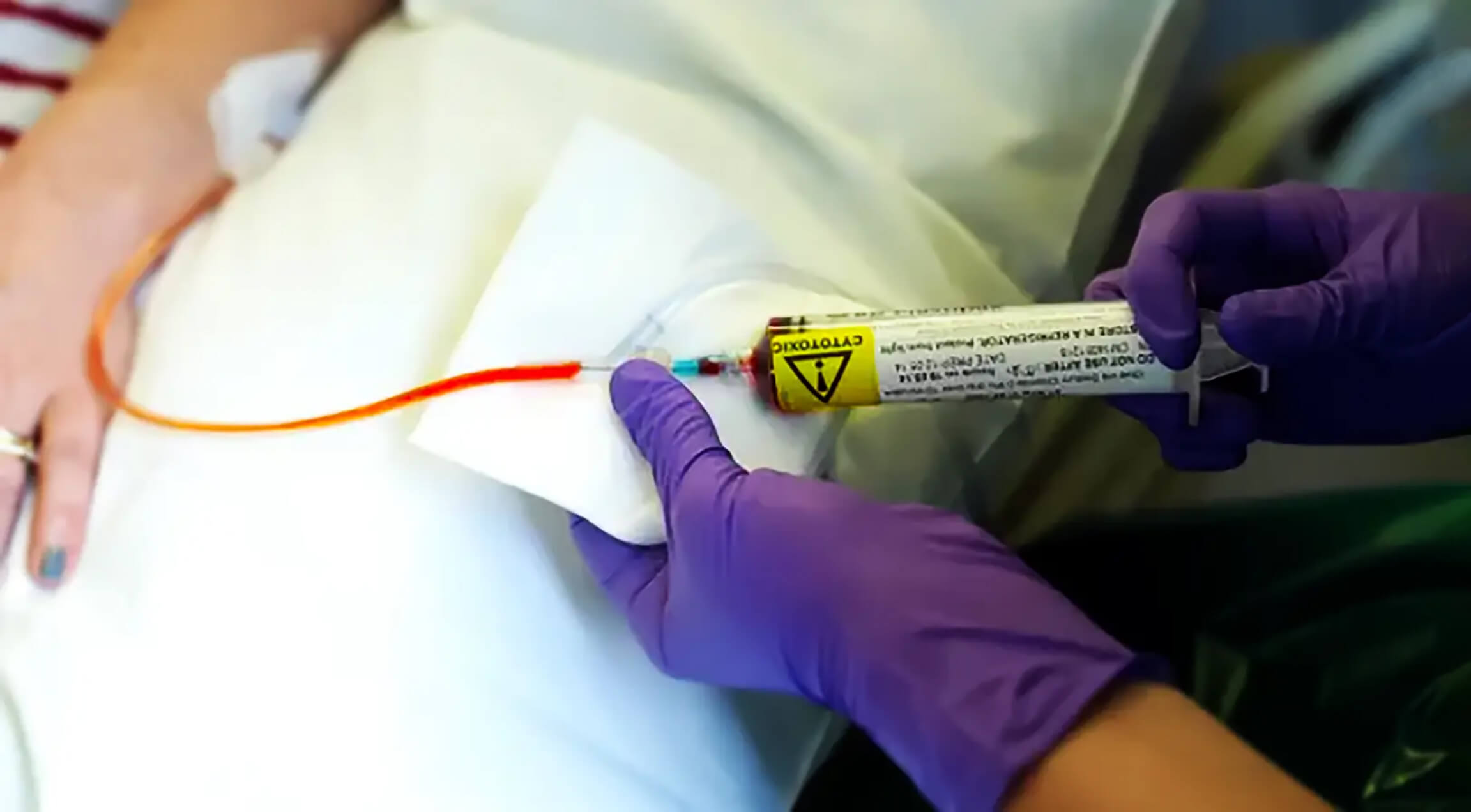
One of the factors that creates inflammation spikes after animal product consumption is a process known as endotoxemia. `Diet-induced metabolic endotoxemia has been proposed as a major root cause of inflammation, and these pathways appear to be detrimental to healthy aging.
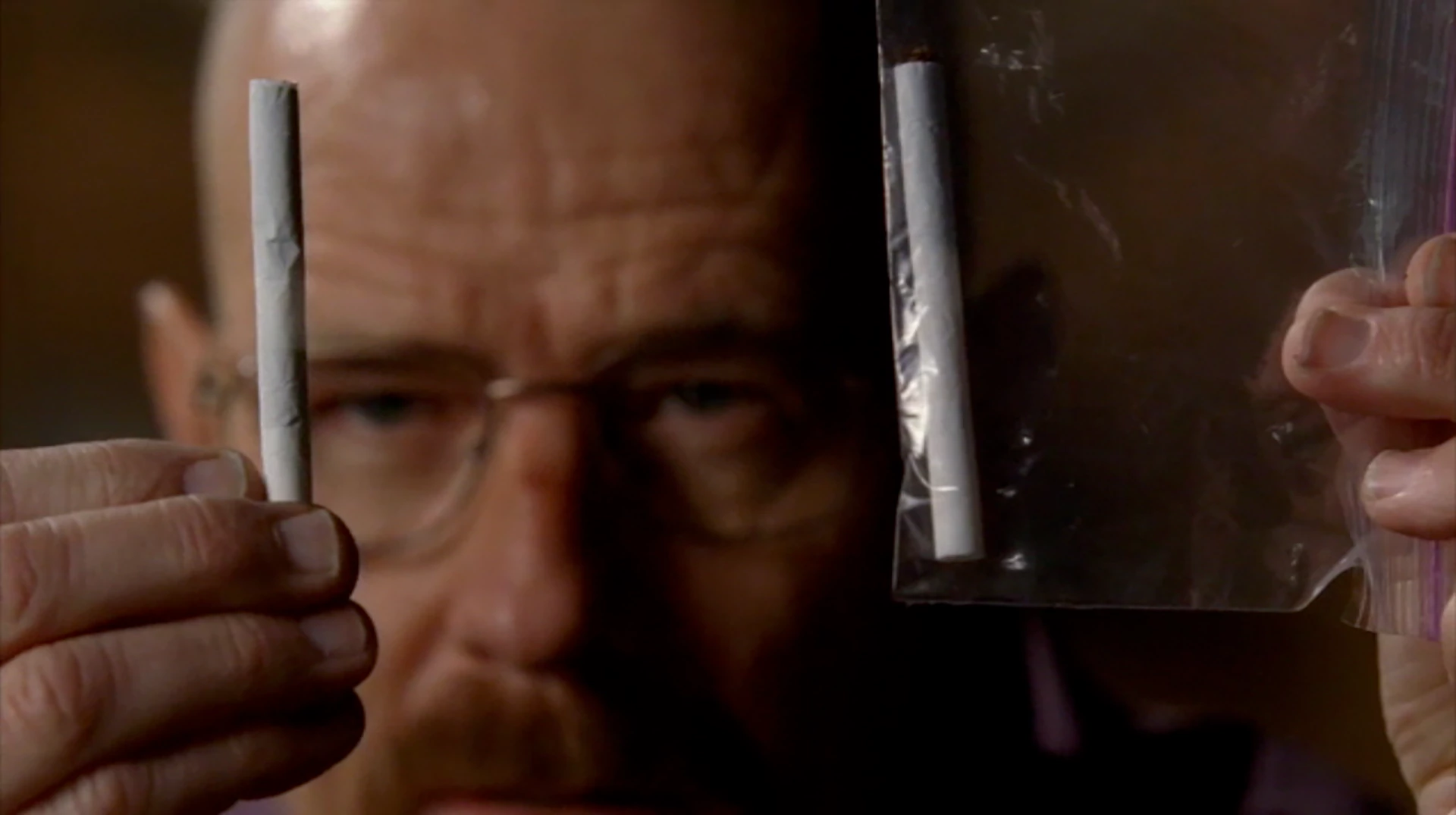
We as humans, unlike carnivores species, have very low resistance filters meaning any live bacteria we eat will be creating inflammation, and diet can kill us if bacteria is dangerous. We cannot eat uncooked meat. Carnivorous animals have extremely corrosive bile acids that are able to kill any living microorganism and their digestive system is practically sterile. We as any other plant eater have mild bile acid and low resistance filters and have to cook meat and any other food item that has the potential to spread an infectious disease. For example, pasteurization is mandatory.
What people don’t understand is that even if we do cook meat we do not magically dematerialize all of the bacteria that were present in there. We only kill them by heat but they are still in there. Microorganisms are still in the meat just dead. They will not pose any risk of infection anymore.
But that does not mean that they don’t pose a risk anymore.
Even dead non-probiotic bacteria do count as toxins.
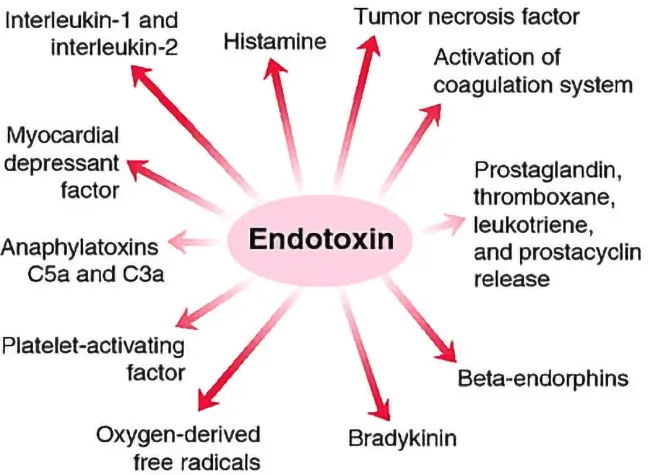
Some of the world’s most toxic substances are these dead meat bacteria endotoxins.
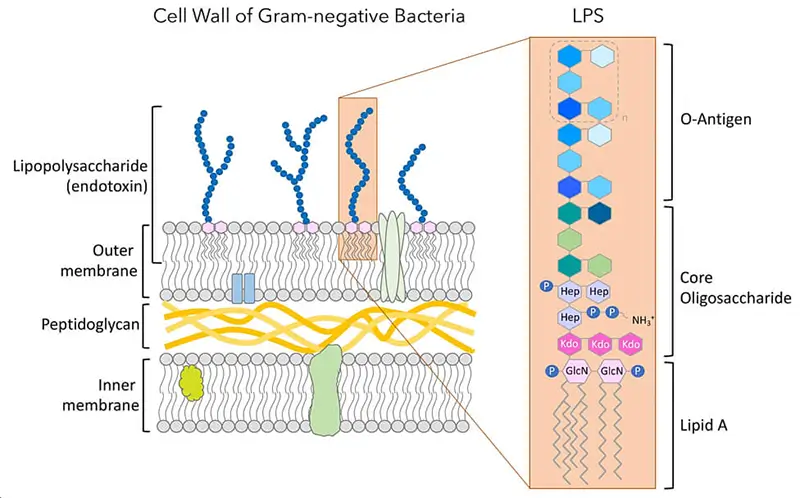
These substances known as endotoxins (Greek éndon within; cognate with Old Irish ind-) are thermally (250C) and chemically stable and extremely toxic. Endotoxin is a complex lipopolysaccharide (LPS) found in the outer cell membrane of gram-negative bacteria (E.coli, Salmonella typhi, Shigella).
Bacteria shed endotoxins in large amounts upon cell death creating an endotoxemia state in the body. Meaning, the bacteria can be dead or cooked for a long time, but their endotoxins are still there. Endotoxins are chemically very stable and can withstand our body’s best attempts at acid and enzyme degradation. One of the leading causes of hundreds of studies that display enlarged inflammation from animal foods, but not from most plant foods, maybe is a consequence of a toxic load of dead bacteria endotoxins in animal products. These bacteria shed endotoxins after death and then when we eat them they are absorbed into our system, leading to the endotoxemia inflammation we see after egg, meat, and dairy consumption, as well.
This would cause damage to our internal organs and the entire body and will increase the chances of chronic diseases (Ghosh et al., 1993).
If we already have an autoimmune disease such as atherosclerosis, for example, this will just agitate our immune system even worse and would create even more of an immune response (Stoll et al., 2004).
Here is one study that discovered a link between endotoxin exposure and diabetes type 2 (Harte et al., 2012).
What a low level of chronic endotoxemia inflammation does is that it causes damage like any other inflammation just in a prolonged period. What that translates to is faster and more noticeable DNA damage, a higher mortality rate from chronic diseases, and decreased longevity.
In contrast, plant foods do not show this trait, and actual consumption is correlated with the anti-inflammatory reaction after a meal because of the antioxidants and other anti-inflammatory phytochemicals. It would be interesting to see how much inflammation meat consumption causes in carnivorous species. So far I was unable to find research that looks into dead meat bacteria endotoxemia exposure in carnivorous species. This could be potentially interesting because if meat causes no inflammation in carnivorous animals, we might look at a way how to lower the same inflammation in our own bodies.
Consumption of meat, therefore, is associated with an increase in inflammation even if we disregard the risk of live infectious bacteria. This mechanism is natural and normal, and all of the carnivorous species had it to some extent but are more adept at coping with it.
A fresh hamburger contains approximately a hundred million bacteria per quarter pounder. Eating meals high in bacterial endotoxins could develop mild but systemic inflammatory episodes that predispose subjects to the development of chronic diseases.
The animal fat that comes in the same package may play a role in the pathogenesis of this after-meal inflammation. Endotoxins hold a powerful attraction for saturated fat, so they stick to it and then get absorbed through the gut wall and into the bloodstream (Erridge, 2011).
Would this happen if we eat food that is high in saturated fat from plant origin? It would, but the difference is that there are no high levels of these toxins in plant-based foods. For example, cocoa has a high fat content. It is one of the plants that has energy stored in a form of saturated fat, the same fat that is found in the animal kingdom. But cocoa also has a large number of antioxidants and in studies always decreases the level of C-reactive protein in subjects (a marker for inflammation) (Erridge et al., 2007), (Herieka et al., 2014).
The high antioxidant content of cocoa prevails and is able to neutralize the pro-inflammatory effects of endotoxins that are not present in the plants in high numbers, to begin with (Gu et al., 2014).
The problem with meat is a high concentration of bacteria. This means that eating a standard Western diet rich in animal protein and refined sugar and fat will require a much higher level of antioxidants to negate the bad pro-inflammatory effects.
The question will be where can we use these findings and can we diminish the bed proinflammatory effects of high animal protein meals with antioxidant-rich food. In other words, can we still eat meat but also add some high-antioxidant vegetables or fruits to the same meal to avoid the risk (Burton-Freeman, 2010).
There was a large number of studies done on a topic and the conclusion is yes, we can, but only to some extent. Avoidance of toxin exposure is our primary goal. If you really have to eat animal products then at least incorporate an adequate amount of anti-inflammatory food sources and calculate your optimal ORAC (Oxygen radical absorbance capacity) intake. You can find ORAC values here (ORAC Values). This would not completely negate the toxicity of dead meat bacteria endotoxemia exposure. These toxins are very potent and hard to detoxify. There are genetically susceptible individuals that have a harder time detoxifying these compounds. Antioxidant-rich food will lower the risk to a relevant degree and my advice is to optimize the antioxidant intake.
The best course of action would be to have a whole food plant-based diet that has an optimal level of ORAC units and a wide range of proinflammatory food sources with an adequate level of all essential micronutrients.
This is what the British Journal of Nutrition has to say about it.
“Postprandial (fed) state is a pro-oxidant state. The postprandial period is a time of active oxidative metabolism and formation of ROS (free radicals). There is increasing evidence that the postprandial state is an important contributing factor to chronic disease. Two main questions are posed: first, what is the role of plant foods, specifically fruits rich in complex and simple phenolic compounds in postprandial metabolic management; and second, does the evidence support consuming these fruits with meals as a practical strategy to preserve health and lower risk for disease? The collected data suggest that consuming phenolic-rich fruits increases the antioxidant capacity of the blood, and when they are consumed with high fat and carbohydrate ‘pro-oxidant and pro-inflammatory’ meals, they may counterbalance their negative effects. Given the content and availability of fat and carbohydrate in the Western diet, regular consumption of phenolic-rich foods, particularly in conjunction with meals, appears to be a prudent strategy to maintain oxidative balance and health.“
References:
- Ghosh, S., Latimer, R. D., Gray, B. M., Harwood, R. J., & Oduro, A. (1993). Endotoxin-induced organ injury. Critical care medicine, 21(2 Suppl), S19–S24. https://doi.org/10.1097/00003246-199302001-00005
- Stoll, L. L., Denning, G. M., & Weintraub, N. L. (2004). Potential role of endotoxin as a proinflammatory mediator of atherosclerosis. Arteriosclerosis, thrombosis, and vascular biology, 24(12), 2227–2236. https://doi.org/10.1161/01.ATV.0000147534.69062.dc
- Harte, A. L., Varma, M. C., Tripathi, G., McGee, K. C., Al-Daghri, N. M., Al-Attas, O. S., Sabico, S., O’Hare, J. P., Ceriello, A., Saravanan, P., Kumar, S., & McTernan, P. G. (2012). High fat intake leads to acute postprandial exposure to circulating endotoxin in type 2 diabetic subjects. Diabetes care, 35(2), 375–382. https://doi.org/10.2337/dc11-1593
- Erridge C. (2011). The capacity of foodstuffs to induce innate immune activation of human monocytes in vitro is dependent on food content of stimulants of Toll-like receptors 2 and 4. The British journal of nutrition, 105(1), 15–23. https://doi.org/10.1017/S0007114510003004
- Erridge, C., Attina, T., Spickett, C. M., & Webb, D. J. (2007). A high-fat meal induces low-grade endotoxemia: evidence of a novel mechanism of postprandial inflammation. The American journal of clinical nutrition, 86(5), 1286–1292. https://doi.org/10.1093/ajcn/86.5.1286
- Herieka, M., & Erridge, C. (2014). High-fat meal induced postprandial inflammation. Molecular nutrition & food research, 58(1), 136–146. https://doi.org/10.1002/mnfr.201300104
- Gu, Y., Yu, S., Park, J. Y., Harvatine, K., & Lambert, J. D. (2014). Dietary cocoa reduces metabolic endotoxemia and adipose tissue inflammation in high-fat fed mice. The Journal of nutritional biochemistry, 25(4), 439–445. https://doi.org/10.1016/j.jnutbio.2013.12.004
- Burton-Freeman B. (2010). Postprandial metabolic events and fruit-derived phenolics: a review of the science. The British journal of nutrition, 104 Suppl 3, S1–S14. https://doi.org/10.1017/S0007114510003909
Related Posts
Do you have any questions about nutrition and health?
I would love to hear from you and answer them in my next post. I appreciate your input and opinion and I look forward to hearing from you soon. I also invite you to follow us on Facebook, Instagram, and Pinterest for more diet, nutrition, and health content. You can leave a comment there and connect with other health enthusiasts, share your tips and experiences, and get support and encouragement from our team and community.
I hope that this post was informative and enjoyable for you and that you are prepared to apply the insights you learned. If you found this post helpful, please share it with your friends and family who might also benefit from it. You never know who might need some guidance and support on their health journey.
– You Might Also Like –

Learn About Nutrition
Milos Pokimica is a doctor of natural medicine, clinical nutritionist, medical health and nutrition writer, and nutritional science advisor. Author of the book series Go Vegan? Review of Science, he also operates the natural health website GoVeganWay.com
Medical Disclaimer
GoVeganWay.com brings you reviews of the latest nutrition and health-related research. The information provided represents the personal opinion of the author and is not intended nor implied to be a substitute for professional medical advice, diagnosis, or treatment. The information provided is for informational purposes only and is not intended to serve as a substitute for the consultation, diagnosis, and/or medical treatment of a qualified physician or healthcare provider.NEVER DISREGARD PROFESSIONAL MEDICAL ADVICE OR DELAY SEEKING MEDICAL TREATMENT BECAUSE OF SOMETHING YOU HAVE READ ON OR ACCESSED THROUGH GoVeganWay.com
NEVER APPLY ANY LIFESTYLE CHANGES OR ANY CHANGES AT ALL AS A CONSEQUENCE OF SOMETHING YOU HAVE READ IN GoVeganWay.com BEFORE CONSULTING LICENCED MEDICAL PRACTITIONER.
In the event of a medical emergency, call a doctor or 911 immediately. GoVeganWay.com does not recommend or endorse any specific groups, organizations, tests, physicians, products, procedures, opinions, or other information that may be mentioned inside.
Editor Picks –
Milos Pokimica is a doctor of natural medicine, clinical nutritionist, medical health and nutrition writer, and nutritional science advisor. Author of the book series Go Vegan? Review of Science, he also operates the natural health website GoVeganWay.com
Latest Articles –
Plant Based News
-
Frozen Tofu Just Got A Summer Makeover In This Eggplant Gratin
on July 2, 2025
-
A Day Of High-Protein Vegan Meals – Featuring Homemade Seitan
on July 2, 2025
-
These Raw Apple Pie Bars Are Gluten-Free And Vegan
on July 2, 2025
-
Califia Farms Expands Oat Barista Range With Two New Nut-Flavored Blends
on July 2, 2025
-
Vegan Marathoner To Run Length Of UK For His 60th Birthday
on July 1, 2025
-
These Easy Plant-Based Enchiladas Are Oil-Free
on July 1, 2025
-
‘This Is Our Most Popular Vegan Salad After 20 Years In Business’
on July 1, 2025
Top Health News — ScienceDaily
- A midlife MRI that spots rapid aging and signals disease long before symptomson July 2, 2025
A new brain scan tool shows how quickly your body and mind are aging. It can spot early signs of diseases like dementia, long before symptoms begin. The scan looks at hidden clues in your brain to predict future health.
- The pandemic pet boom was real. The happiness boost wasn’ton July 2, 2025
Locked-down Hungarians who gained or lost pets saw almost no lasting shift in mood or loneliness, and new dog owners actually felt less calm and satisfied over time—hinting that the storied “pet effect” may be more myth than mental-health remedy even in extreme isolation.
- Tiny gut “sponge” bacteria found to flush out toxic PFAS “forever chemicals”on July 2, 2025
Cambridge scientists have spotted gut bacteria that greedily soak up PFAS “forever chemicals,” then ferry them safely out of the body in animal tests, removing up to three-quarters of the toxins within minutes. Their findings hint at probiotic pills that could shield people from PFAS-linked cancers, fertility issues, and heart disease while lawmakers scramble to rein in 4,700 widespread compounds.
- Researchers tested 200 toddlers — 96 chemicals were lurking in their bodieson July 2, 2025
Researchers testing urine from 2- to 4-year-olds in four U.S. states uncovered 96 different chemicals, many of them unmonitored and linked to hormone and brain disruption. Legacy toxins like triclosan are slowly declining, yet replacements such as DINCH plasticizer and modern pesticides are rising. Toddlers—especially the youngest, later-born, and those from minority groups—often carried higher levels than their own mothers. Scientists urge expanded biomonitoring and stricter regulations […]
- Ultrafast 12-minute MRI maps brain chemistry to spot disease before symptomson July 2, 2025
Illinois engineers fused ultrafast imaging with smart algorithms to peek at living brain chemistry, turning routine MRIs into metabolic microscopes. The system distinguishes healthy regions, grades tumors, and forecasts MS flare-ups long before structural MRI can. Precision-medicine neurology just moved closer to reality.
- Synthetic storm: What’s really in your teen’s vape — and why scientists are alarmedon July 1, 2025
Teen vaping is changing fast — and not in a good way. A large national study found that more adolescents are vaping THC, CBD, and especially synthetic cannabinoids, which are often unregulated and far more dangerous. Even more troubling, many teens don’t know what’s in their vape pens at all. Researchers also found that girls are now more likely than boys to vape these substances. As these mysterious and risky chemicals gain popularity, scientists are sounding the alarm about the urgent […]
- Is that really ADHD? Why flawed trials may be misleading millionson July 1, 2025
Researchers reviewing nearly 300 top-tier ADHD drug trials found that half skipped the rigorous, expert-led evaluations needed to rule out other conditions like depression or schizophrenia. With diagnoses often made by unqualified staff—or even by computer—many participants may not have actually had ADHD, casting doubt on study outcomes that shape treatment guidelines.
PubMed, #vegan-diet –
- Exploring the role of gut microbiota in rheumatoid arthritis: the effects of diet and drug supplementationon July 2, 2025
Rheumatoid Arthritis (RA) is a chronic autoimmune disease that mostly breaks out at the joints. It further causes bone erosion and decreased life quality due to severe pain. Current drugs are mainly focused on reducing pain, but unable to terminate the disease progression. This study aims to determine the effect of diet types (Western, Vegan and Mediterranean) on RA progression. Some dietary supplements and drug administration (Huayu-Qiangshen-Tongbi formula or Leflunomide plus Methotrexate) […]
- Blood biomarkers of Alzheimer’s disease in Australians habitually consuming various plant-based dietson June 30, 2025
BackgroundEvidence suggests that plant-based diets (PBDs) may be protective against neurodegenerative diseases such as Alzheimer’s disease (AD).ObjectiveThis study examined associations between blood-based AD biomarkers in individuals 30-75 years without current or diagnosed cardiovascular disease following different PBDs versus regular meat-eating diets (RMEs).MethodsThis secondary analysis of the Plant-based Diets study measured Aβ(1-42)/Aβ(1-40), p-tau181, NFL, and GFAP in 237 plasma […]
- Zinc supplementation among zinc-deficient vegetarians and vegans restores antiviral interferon-α response by upregulating interferon regulatory factor 3on June 28, 2025
CONCLUSION: We identified zinc-dependent IRF3 expression as an essential cellular mechanism behind impaired IFNα response in zinc-deficient subjects. This may contribute to disturbed antiviral immunity and cause increased susceptibility to virus infections in vivo. Oral zinc supplementation effectively restored IRF3 and IFNα levels. Hence, nutritional interventions may become increasingly important in order to prevent health implications from micronutrient deficiencies among vegetarians and…
- Micronutrient intake and nutritional status in 16-to-24-year-olds adhering to vegan, lacto-ovo-vegetarian, pescatarian or omnivorous diets in Swedenon June 26, 2025
CONCLUSION: Youth, regardless of dietary practice, need support to ensure adequate micronutrient intakes, particularly for vitamin D and selenium. Further research is required to evaluate iodine nutrition in Swedish youth.
- Integrating comparative genomics and risk classification by assessing virulence, antimicrobial resistance, and plasmid spread in microbial communities with gSpreadCompon June 26, 2025
CONCLUSIONS: The gSpreadComp workflow aims to facilitate hypothesis generation for targeted experimental validations by the identification of concerning resistant hotspots in complex microbial datasets. Our study raises attention to a more thorough study of the critical role of diet in microbial community dynamics and the spread of AMR. This research underscores the importance of integrating genomic data into public health strategies to combat AMR. The gSpreadComp workflow is available at…
Random Posts –
Featured Posts –

Latest from PubMed, #plant-based diet –
- Optimizing Aedes albopictus rearing: effects of insect- and bacteria-based larval diets on immature and adult performanceby Eleni C Savvidou on July 2, 2025
Mass production of Aedes albopictus for Sterile Insect Technique (SIT) requires cost-effective and nutritionally balanced larval diets to ensure high survival, optimal development and competitive adult fitness. This study evaluates the potential of insect-derived meals and dead autoclaved bacteria as the main protein sources in mosquito larval diets. Four isoproteinic diets were studied, each one incorporating different protein sources: Brewer’s yeast (CAA), Tenebrio molitor meal (UTH-YM),…
- Association between adherence to Mediterranean-DASH intervention for neurodegenerative delay diet and disease severity in patients with ulcerative colitisby Zeinab Nikniaz on July 2, 2025
Considering the importance of induction and maintenance of remission in patients with ulcerative colitis (UC), different studies investigated the association between adherence to healthy dietary patterns and disease severity. This cross-sectional study investigated the association between Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) diet score and disease severity in patients with UC. In this study, 158 patients with UC were included. Disease severity was determined by a…
- Pace of adoption of alternatives to animal-source foods is an important factor in reaching climate goalsby Galina Hale on July 2, 2025
The global food system is a significant contributor to greenhouse gas emissions that drive climate change. Animal agriculture accounts for a large share of food-system emissions, both directly and through the production of animal feed. Global population growth and rising incomes imply a further increase in demand for animal-source foods if current trends persist. Limiting global warming to the targets set by the international community will not be possible without the rapid reduction of a…
- Exploring nudging strategies for plant-based dietary choices in hospital patients: a quasi-experimental studyby Kristin Hünninghaus on July 2, 2025
CONCLUSION: Centrally implemented nudging is a simple and effective strategy that can increase patients’ choice of plant-based menus, which in turn may promote patient health and contribute to positive environmental outcomes.
- Association between vegetarian diet and risk of frailty in Chinese older adults: a prospective studyby Yilun Huang on July 2, 2025
CONCLUSIONS: In this prospective study, vegetarian diets were observed to be associated with higher frailty risk, compared to the omnivorous diet in Chinese older adults. Future research is needed to confirm our observations.
- Whole grain and refined grain consumption and the risk of hypertension: a systematic review and meta-analysis of prospective studiesby Dagfinn Aune on July 1, 2025
A high intake of whole grains has been associated with a reduced risk of hypertension, however, studies have not been entirely consistent. Findings regarding refined grains and hypertension have also been inconsistent. We conducted a systematic review and meta-analysis of prospective cohort studies on whole grain and refined grain consumption and hypertension risk. PubMed and Embase databases were searched up to 25th of July 2024. Random effects models were used to estimate summary relative…