GMI Calculator
The formula for GMI is:
GMI=3.31+0.02392×AG
Where AG is the average glucose derived from CGM data in mg/dL.
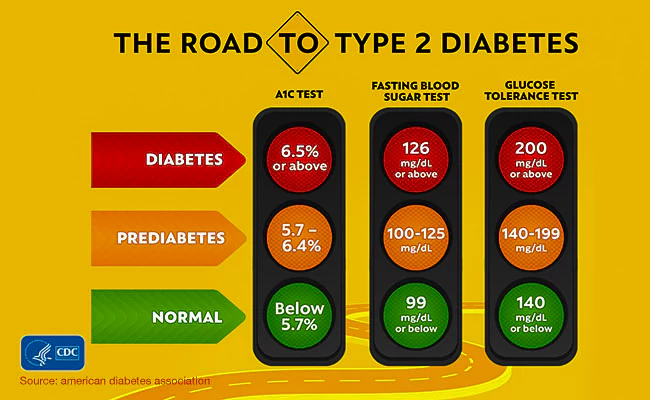
The target for GMI is the same as for A1C. The goal for most adults with diabetes is less than 7%.
- Normal – below 5.7%
- Prediabetes – between 5.7% and 6.5%
- Diabetes – 6.5% and higher
How To Use Glucose Management Indicator GMI (With Calculator) For Diabetes
CGM can help people with diabetes manage their blood sugar better, avoid highs and lows, and see the effects of food, exercise, and medication on their glucose levels.
Milos Pokimica
Written By: Milos Pokimica on October 10, 2023
Medically Reviewed by: Dr. Xiùying Wáng, M.D.
Updated October 12, 2023| GMI calculated for various CGM-derived mean glucose concentrations. | |
|---|---|
| CGM-derived mean glucose (mg/dL) | GMI (%)* |
| 100 | 5.7 |
| 125 | 6.3 |
| 150 | 6.9 |
| 175 | 7.5 |
| 200 | 8.1 |
| 225 | 8.7 |
| 250 | 9.3 |
| 275 | 9.9 |
| 300 | 10.5 |
| 350 | 11.7 |
| CGM-measured mean glucose (mmol/L) | GMI (mmol/mol)† |
| 5 | 36.2 |
| 6 | 40.9 |
| 7 | 45.7 |
| 8 | 50.4 |
| 9 | 55.1 |
| 10 | 59.8 |
| 12 | 69.2 |
| 14 | 78.6 |
| 16 | 88.0 |
| 18 | 97.4 |
†GMI (mmol/mol) = 12.71 + 4.70587 × [mean glucose in mmol/L]. Adapted by (Bergenstal et al., 2018).
How to Monitor Your Blood Sugar with New Technologies.
If you have type 1 diabetes, you know how important it is to keep your blood sugar levels under control. You also know how challenging it can be to do that. You need to check your blood sugar regularly, adjust your insulin doses, and balance your food, exercise, and other factors.
But what if there was a better way to monitor your blood sugar levels? A way that could give you more information, more feedback, and more convenience? A way that could help you improve your diabetes management and reduce your risk of complications?
That’s what this article is about. We will tell you about two new technologies that can help you monitor your blood sugar levels more effectively: continuous glucose monitoring (CGM) and flash glucose monitoring (FGM).
CGM and FGM are devices that can show you your current level, as well as trends, patterns, and alerts. They can also calculate an estimate of your HbA1c, which is a blood test that measures your average blood sugar level over the past 2 to 3 months.
CGM is a device that measures your glucose levels every few minutes using a sensor inserted under your skin. It is a system that tracks your blood sugar level every few minutes throughout the day and night. It can show you how your blood sugar changes over time, how different factors affect it, and how to avoid highs and lows.
CGM can help you track your glucose trends and patterns, and alert you when your glucose levels are too high or too low.
CGM can help people with diabetes manage their blood sugar better, avoid highs and lows, and see the effects of food, exercise, and medication on their glucose levels.

A CGM system consists of three main parts: a sensor, a transmitter, and a receiver. The sensor is a small device that is inserted under the skin, usually on the abdomen or the arm, and measures the glucose level in the interstitial fluid (the fluid that surrounds the cells in the body). The transmitter is attached to the sensor and sends the glucose data wirelessly to the receiver. The receiver can be a dedicated device, a smartphone app, or a smartwatch that displays the glucose readings, trends, and alerts.
There are different types of CGM systems available, but the most common one is called real-time CGM (rtCGM). This means that you can see your glucose levels at any time on the screen, and you can also set alarms to warn you when your levels are too high or too low.
RtCGM can help you make better decisions about your diabetes management, such as when to eat, how much to eat, when to take medication or insulin, and how to adjust your doses
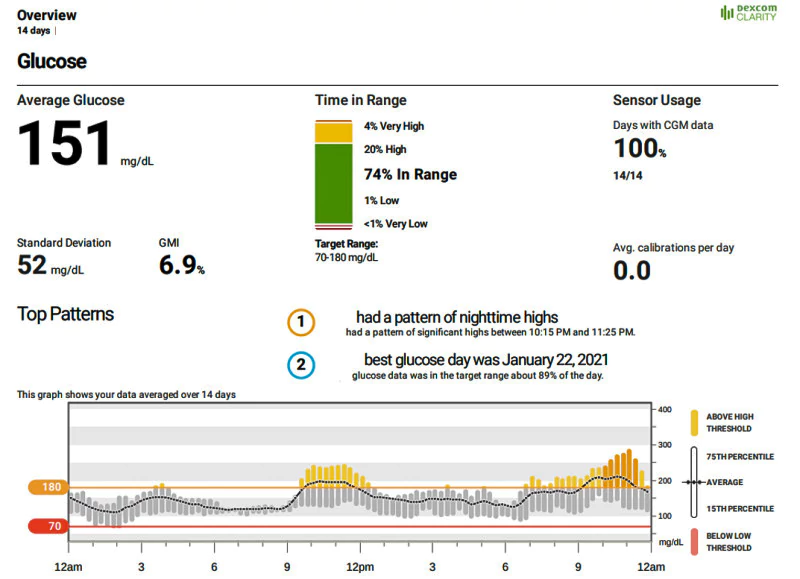
CGM can also calculate a number called GMI, which stands for glucose management indicator. It is similar to HbA1c, but it is based on your short-term average blood sugar level, rather than your long-term exposure (Gomez-Peralta, et al., 2021). It uses the same units as HbA1c (% or mmol/mol), but it can be different from it.
Why does this matter? Because sometimes HbA1c and GMI can disagree. They can show different results for the same person and the same blood sugar level. This can be confusing and misleading for you and your healthcare provider. It can also affect your treatment decisions and your outcomes.
Parameters for Glycemic Control.
Some experts recommend using other parameters that can utilize more information from your CGM data. CGM can provide these measurements. These parameters include (Pleus et al., 2021):
- Time in range (TiR): The percentage of time that your blood glucose is within a target range, usually between 70 and 180 mg/dL. This reflects how well your therapy is keeping your blood glucose stable and avoiding extremes.
- Time below range (TbR): The percentage of time that your blood glucose is below a certain threshold, usually 70 mg/dL or 54 mg/dL. This indicates how often you experience hypoglycemia, which can be dangerous and unpleasant.
- Time above range (TaR): The percentage of time that your blood glucose is above a certain threshold, usually 180 mg/dL or 250 mg/dL. This shows how often you experience hyperglycemia, which can damage your organs and increase your risk of complications.
- Glucose management indicator (GMI): A number that estimates your HbA1c based on your CGM data. This can help you track your progress and compare your results with other tests.
- Coefficient of variation (CV): A number that measures how much your blood glucose varies around the mean. This reflects how consistent or variable your blood glucose levels are.
These parameters can help you understand your glycemic control better than HbA1c alone. They can also help you set goals, adjust your therapy, and improve your outcomes.
From: The Management of Type 1 Diabetes
How Accurate is CGM Compared to Fingerstick Testing?
CGM and fingerstick testing are both methods to measure glucose levels, but they have different sources and accuracy. CGM measures glucose in the interstitial fluid, which is the fluid that surrounds the cells in the body, while fingerstick testing measures glucose in the blood. Interstitial glucose levels lag behind blood glucose levels by about 9 minutes on average, so CGM and fingerstick testing may show different readings, especially when glucose levels are changing rapidly.
The accuracy of CGM and fingerstick testing is measured by the mean absolute relative difference (MARD), which is the average percentage of error compared to a laboratory-measured glucose level. The lower the MARD, the more accurate the device. The typical MARD for commercially available CGMs ranges from 9% to 15%, while the typical MARD for commercially available fingerstick meters ranges from 5% to 10%. This means that fingerstick testing is generally more accurate than CGM, but both have a margin of error.
Therefore, CGM and fingerstick testing should not be used interchangeably, but rather as complementary tools to monitor glucose levels. CGM can provide continuous and real-time data, trends, and alerts, while fingerstick testing can provide more accurate and reliable readings. You should always confirm your CGM reading with a fingerstick test before making any changes to your diabetes treatment plan. You should also consult with your healthcare provider before starting or changing your diabetes care plan based on CGM or fingerstick data.
CGM vs Fingerstick Meter?
How do CGM and FGM compare with the traditional method of self-monitoring of blood glucose (SMBG) using a fingerstick meter? And how do they affect your diabetes outcomes, such as HbA1c, hypoglycemia, quality of life, and treatment satisfaction?
Here are the main findings of this review (Dicembrini et al., 2021):
- CGM can lower your HbA1c by about 0.2% to 0.3% compared to SMBG. It can also reduce your risk of severe hypoglycemia by about half.
- CGM can improve your quality of life and treatment satisfaction, but not all studies measured or reported these outcomes.
- FGM can reduce your episodes of mild hypoglycemia and increase your treatment satisfaction, but it may not lower your HbA1c significantly.
- CGM combined with an insulin pump can lower your HbA1c by about 0.5% compared to SMBG combined with multiple daily injections.
- CGM combined with an automated system can lower your HbA1c by about 0.2% compared to SMBG combined with an insulin pump, but only two studies have tested this so far.
These findings suggest that CGM and FGM are useful tools that can help you monitor your blood sugar levels better than SMBG. However, they are not perfect. They may not agree with your HbA1c test or each other. They may also have some limitations, such as cost, accuracy, or usability.
Therefore, you should always consult with your healthcare provider before using CGM or FGM. You should also follow your treatment plan, check your blood sugar levels regularly, and make healthy lifestyle choices. CGM and FGM can help you do that, but you are the one who makes it work.
How Accurate is GMI Compared to A1C?
HbA1c is a common measure of your average blood glucose level over the past 2 to 3 months. It is useful to monitor your long-term glycemic control and your risk of complications. However, HbA1c does not tell you everything. It does not show you how much your blood glucose fluctuates throughout the day, or how often you experience low or high blood glucose levels. These aspects are also important for your health and well-being.
GMI estimates your A1C level based on your CGM data, but it may not always match your laboratory-measured A1C.
This is because many factors can affect the accuracy of both CGM and A1C measurements, such as the type and quality of the CGM device, the frequency and duration of calibration and sensor changes, the presence of hemoglobin variants or conditions that affect red blood cell lifespan, the variability and distribution of glucose levels over time, and the time lag between interstitial fluid and blood glucose levels.
The difference between GMI and A1C varies widely among individuals. The study that reviewed this issue found that (Bergenstal et al., 2018):
- Only 11% of people showed less than a 0.1 percentage point difference between their A1C and GMI. This means if their GMI was 7.0%, their A1C was between 6.9-7.1%.
- 50% of people had differences of 0.5 percentage points or less. This means if GMI was 7%, actual A1C ranged from 6.5%-7.5%.
- 22% of people had a difference of 1 percentage point or greater. This means if GMI was 7%, actual A1C could be as low as 6% or as high as 8%.
The study also found that the differences between A1C and GMI were largely negative in people with lower A1C levels, meaning that GMI tended to overestimate A1C in this group.
Therefore, GMI should not be used to diagnose or treat diabetes, but rather as an educational tool to help you understand how your glucose management affects your A1C level. You should always consult with your healthcare provider before making any changes to your diabetes care plan based on GMI or CGM data.
Explaining GMI to individuals with diabetes (Bergenstal et al., 2018).
| GMI tells you what your approximate A1C level is likely to be, based on the average glucose level from your CGM readings for 14 or more days. | |
| • GMI gives you the A1C level that would usually be expected from a large number of individuals with diabetes who have the same average CGM glucose level as you. • However, your laboratory A1C might be similar to, higher than, or lower than your GMI. Your GMI is calculated from your average CGM glucose, which measures glucose in interstitial fluid (under the skin) every 1–5 min. ○ Laboratory A1C is a measure of how much glucose has attached to the hemoglobin in your red blood cells over the life of each red blood cell, ∼120 days. ○ Each person’s red blood cells may live for a slightly different number of days, and there may be differences in factors that affect how glucose attaches to your red blood cells. Therefore, we do not expect people with the same average glucose or calculated GMI to have the same laboratory A1C value. ○ There also are certain medical conditions that affect the life span of red blood cells that may explain differences between the GMI and laboratory A1C, including hemoglobinopathies and hemolytic anemia. | |
| Here is what having a difference in laboratory-measured A1C and GMI may mean: | |
| Laboratory A1C vs. GMI | |
| 8.0% vs. 7.8% | A1C measured from a blood test that is similar to your GMI means that your average CGM glucose level is about what would be predicted from the measured A1C. (Based on the average of values from many other people.) |
| 8.0% vs. 7.2% | A1C measured from a blood test that is higher than your GMI means that your average CGM glucose level is lower than would be predicted from the measured A1C. (Based on the average of values from many other people.) |
| 7.2% vs. 8.0% | A1C measured from a blood test that is lower than your GMI means that your average CGM glucose level is higher than would be predicted from the measured A1C. (Based on the average of values from many other people.) |
What are the Benefits of Using Both the A1C and the CGM Data?
The A1C and the CGM data can provide different information about your blood sugar levels. The A1C tells you your long-term average, while the CGM data tells you your short-term variations. The A1C reflects your overall diabetes control, while the CGM data reveals your daily patterns and trends.
By using both the A1C and the CGM data, you can get a more complete picture of your blood sugar levels. You can also set more realistic and personalized goals for your diabetes management. For example, you can discuss with your healthcare provider both an A1C target and a target range for your blood sugar levels based on your CGM data.
Using both the A1C and the CGM data can also help you make better decisions about your diabetes treatment. For example, you can adjust your medication or lifestyle based on your CGM feedback and alerts. You can also identify and address any problems or patterns that may affect your blood sugar levels, such as hypoglycemia, hyperglycemia, or glucose variability.
Using both the A1C and the CGM data can also improve your quality of life and treatment satisfaction. For example, you can feel more confident and empowered about managing your diabetes. You can also enjoy more flexibility and convenience in your daily activities.
Can we Use rtCGM for Type 2 Diabetes?
RtCGM is mainly used by people with type 1 diabetes who need to take multiple daily injections of insulin or use an insulin pump. However, some people with type 2 diabetes may also benefit from using rtCGM, especially if they:
- Use intensive insulin therapy (more than three injections per day or an insulin pump).
- Have frequent or severe hypoglycemia (low blood sugar) or hypoglycemia unawareness (not feeling the symptoms of low blood sugar).
- Have poor glycemic control (high HbA1c) despite following their treatment plan.
- Have high glucose variability (large swings in blood sugar levels).
- Want to improve their quality of life and self-management skills.
Not everyone with type 2 diabetes needs rtCGM. Some people may do well with self-monitoring of blood glucose (SMBG) using a fingerstick meter or a flash glucose monitoring (FGM) system that scans a sensor on the arm. These methods are cheaper and less invasive than rtCGM, but they do not provide continuous data or real-time feedback.
If you are interested in using rtCGM for type 2 diabetes, you should talk to your healthcare provider about the pros and cons, the costs and coverage, and the training and support you will need.
What Does the Evidence Say About rtCGM for Type 2 Diabetes?
Several studies have been conducted to evaluate the effectiveness and safety of rtCGM for type 2 diabetes. Most of these studies focused on people who use intensive insulin therapy, as they are more likely to benefit from rtCGM.
The results of these studies showed that rtCGM can help people with type 2 diabetes (Jackson et al., 2021):
- Lower their HbA1c by about 0.3% to 0.5% compared to SMBG or FGM.
- Reduce their time in hyperglycemia (high blood sugar) by about 1 to 2 hours per day.
- Increase their time in range (70 to 180 mg/dL) by about 1 to 3 hours per day.
- Reduce their time in hypoglycemia (low blood sugar) by about 15 to 30 minutes per day.
- Improve their quality of life, satisfaction, confidence, and well-being.
- Experience no serious adverse events or safety issues related to rtCGM.
These benefits were observed regardless of age, sex, duration of diabetes, education level, or baseline HbA1c. However, they were dependent on the frequency and duration of rtCGM use. The more often and longer people used rtCGM, the better their outcomes were.
There are fewer studies on the use of rtCGM for people with type 2 diabetes who do not use insulin or use less intensive insulin therapy. The evidence is limited and mixed, but some studies have suggested that rtCGM may also help these people improve their glycemic control and/or reduce their hypoglycemia. More research is needed to confirm these findings and to identify the best candidates and strategies for rtCGM in this population.
CGM Systems Available on the Market.
Not all CGM systems are the same. They have different features, accuracy, and performance.
This means that the same person using different CGM systems may get different results for the same parameters (Pleus et al., 2021). For example, one CGM system may show more time in range than another, even though the person’s blood glucose levels are the same. This can affect how you interpret your data and how you adjust your therapy.
Some of the most popular CGM systems are:
- Dexcom G6: This is a flash glucose monitoring system that does not require any fingerstick calibration and has a 10-day sensor life. It can send real-time glucose data and alerts to compatible devices via Bluetooth. It also has a feature called Dexcom Share that allows users to share their glucose data with up to five followers.
- FreeStyle Libre 2: This is another flash glucose monitoring system that does not require any fingerstick calibration and has a 14-day sensor life. It can also send real-time glucose data and alerts to compatible devices via Bluetooth. However, unlike Dexcom G6, users need to scan the sensor with their device to get the glucose readings.
- Medtronic Guardian Connect: This is a traditional CGM system that requires fingerstick calibration at least twice a day and has a 7-day sensor life. It can send real-time glucose data and alerts to compatible devices via Bluetooth. It also has a feature called Sugar.IQ that uses artificial intelligence to provide personalized insights and guidance.
- Eversense XL: This is an implantable CGM system that requires a minor surgical procedure to insert the sensor under the skin. The sensor lasts for up to 180 days and can be recharged wirelessly. It can send real-time glucose data and alerts to compatible devices via Bluetooth. It also has a feature called Eversense Now that allows users to share their glucose data with up to five followers.
If you use a CGM system to monitor your glycemic control, you should be aware that the type of system you use can affect the parameters you see. Different systems may give different results for the same person and the same blood glucose levels.
This does not mean that one system is better than another. It just means that you should be careful when comparing results from different systems or when switching from one system to another. You should also consult with your healthcare provider before making any changes to your therapy based on these parameters.
FAQ
References:
- Yari, Z., Behrouz, V., Zand, H., & Pourvali, K. (2020). New Insight into Diabetes Management: From Glycemic Index to Dietary Insulin Index. Current diabetes reviews, 16(4), 293–300. https://doi.org/10.2174/1573399815666190614122626
- Gomez-Peralta, F., Choudhary, P., Cosson, E., Irace, C., Rami-Merhar, B., & Seibold, A. (2022). Understanding the clinical implications of differences between glucose management indicator and glycated haemoglobin. Diabetes, obesity & metabolism, 24(4), 599–608. https://doi.org/10.1111/dom.14638
- Dicembrini, I., Cosentino, C., Monami, M., Mannucci, E., & Pala, L. (2021). Effects of real-time continuous glucose monitoring in type 1 diabetes: a meta-analysis of randomized controlled trials. Acta diabetologica, 58(4), 401–410. https://doi.org/10.1007/s00592-020-01589-3
- Bergenstal, R. M., Beck, R. W., Close, K. L., Grunberger, G., Sacks, D. B., Kowalski, A., Brown, A. S., Heinemann, L., Aleppo, G., Ryan, D. B., Riddlesworth, T. D., & Cefalu, W. T. (2018). Glucose Management Indicator (GMI): A New Term for Estimating A1C From Continuous Glucose Monitoring. Diabetes care, 41(11), 2275–2280. https://doi.org/10.2337/dc18-1581
- Jackson, M. A., Ahmann, A., & Shah, V. N. (2021). Type 2 Diabetes and the Use of Real-Time Continuous Glucose Monitoring. Diabetes technology & therapeutics, 23(S1), S27–S34. https://doi.org/10.1089/dia.2021.0007
- Pleus, S., Kamecke, U., Waldenmaier, D., Link, M., Zschornack, E., Jendrike, N., Haug, C., & Freckmann, G. (2021). Time in Specific Glucose Ranges, Glucose Management Indicator, and Glycemic Variability: Impact of Continuous Glucose Monitoring (CGM) System Model and Sensor on CGM Metrics. Journal of diabetes science and technology, 15(5), 1104–1110. https://doi.org/10.1177/1932296820931825
Related Posts
Do you have any questions about nutrition and health?
I would love to hear from you and answer them in my next post. I appreciate your input and opinion and I look forward to hearing from you soon. I also invite you to follow us on Facebook, Instagram, and Pinterest for more diet, nutrition, and health content. You can leave a comment there and connect with other health enthusiasts, share your tips and experiences, and get support and encouragement from our team and community.
I hope that this post was informative and enjoyable for you and that you are prepared to apply the insights you learned. If you found this post helpful, please share it with your friends and family who might also benefit from it. You never know who might need some guidance and support on their health journey.
- You Might Also Like -

Learn About Nutrition
Milos Pokimica is a doctor of natural medicine, clinical nutritionist, medical health and nutrition writer, and nutritional science advisor. Author of the book series Go Vegan? Review of Science, he also operates the natural health website GoVeganWay.com
Medical Disclaimer
GoVeganWay.com brings you reviews of the latest nutrition and health-related research. The information provided represents the personal opinion of the author and is not intended nor implied to be a substitute for professional medical advice, diagnosis, or treatment. The information provided is for informational purposes only and is not intended to serve as a substitute for the consultation, diagnosis, and/or medical treatment of a qualified physician or healthcare provider.NEVER DISREGARD PROFESSIONAL MEDICAL ADVICE OR DELAY SEEKING MEDICAL TREATMENT BECAUSE OF SOMETHING YOU HAVE READ ON OR ACCESSED THROUGH GoVeganWay.com
NEVER APPLY ANY LIFESTYLE CHANGES OR ANY CHANGES AT ALL AS A CONSEQUENCE OF SOMETHING YOU HAVE READ IN GoVeganWay.com BEFORE CONSULTING LICENCED MEDICAL PRACTITIONER.
In the event of a medical emergency, call a doctor or 911 immediately. GoVeganWay.com does not recommend or endorse any specific groups, organizations, tests, physicians, products, procedures, opinions, or other information that may be mentioned inside.
Editor Picks -
Milos Pokimica is a doctor of natural medicine, clinical nutritionist, medical health and nutrition writer, and nutritional science advisor. Author of the book series Go Vegan? Review of Science, he also operates the natural health website GoVeganWay.com
Latest Articles -
Random Posts -
Featured Posts -