Nutrient Deficiencies in Vegan Diet: Prevention Strategies
Learn about the common nutrient deficiencies in vegan diets and how to prevent them with proper supplementation and food choices.
Milos Pokimica
Written By: Milos Pokimica
Medically Reviewed by: Dr. Xiùying Wáng, M.D.
Updated June 10, 2023Key Takeaways:
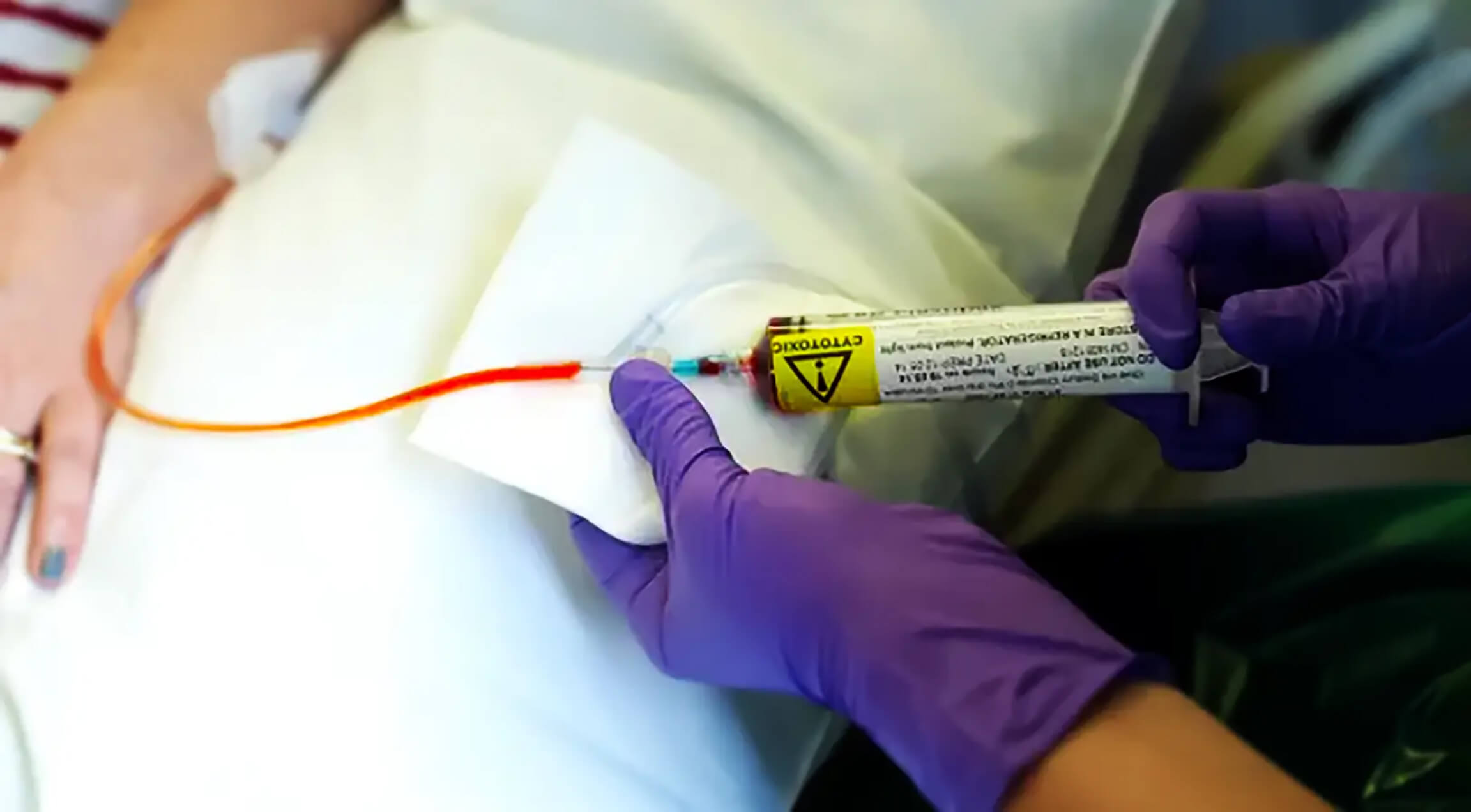
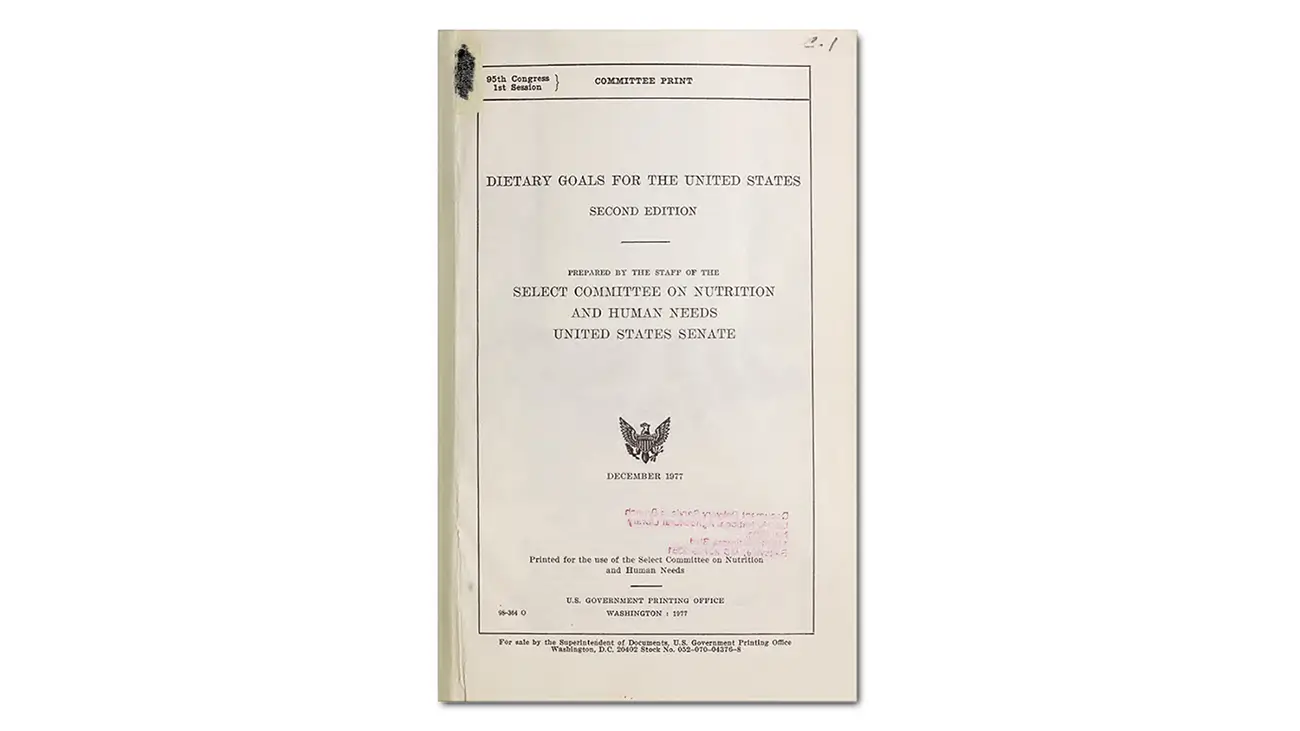
– During the last decades, especially from the late 70s and the time of Mc Govern report onward standard Western diet has been acknowledged as a main source of all diseases of affluence like heart disease and stroke, cancer, and diabetes (Sinha et al., 2009).
– A whole food plant-based diet has been proven to be associated with several beneficial health outcomes and can prevent diseases of affluence.
– Nutrients such as vitamin B12, iodine, and vitamin D may be lacking if a vegan diet is not appropriately planned.
– Excess iron is pro-inflammatory and can lead to cell death and inflammation-related diseases.
– Anemia in vegans is most likely caused by B12 deficiency number one then Zinc deficiency number two then iron deficiency number three. To treat anemia caused by low iron levels you should take one vitamin C pill or 500 mg after the meal only after you have normalized your zinc and B12 levels first and still have iron levels below low normal value.
– Vegans may need up to 50% more zinc than omnivores due to lower bioavailability.
– Idea that a vegan diet lacks protein has been debunked by scientific research. Our bodies recycle dead cell proteins through a process called autophagy.
– Constant overfeeding on high-quality proteins can have serious health implications, including cancer, as it elevates amino acid levels and increases the release of IGF-1 hormones. Overconsumption of certain plant proteins such as soy can negate some of the benefits of a vegan diet on cancer prevention and longevity due to elevated levels of IGF-1 hormones.
– Osteoporosis is not a calcium deficiency disease but rather a chronic vitamin D deficiency disease. However, magnesium deficiency is also prevalent in non-vegan diets and can contribute to osteoporosis.
– It is not recommended to consume high amounts of calcium supplements or fortified foods as they can cause spikes in the bloodstream leading to calcifications in the arteries and potentially lead to cardiovascular issues. It’s best to get your daily calcium intake from whole food sources only.
– Vitamin K2 is not actually a vitamin, but our bodies can make it from vitamin K1 found in plants. It can also be found in fermented foods like natto, sauerkraut, and kimchi.
– Vegans have to take B12 supplements to ensure they are receiving adequate levels of the vitamin. Plant-based sources of B12 are not considered reliable or sufficient.
– Plant-based dieters do not consume any creatine in their diet and may benefit from taking a creatine supplement to decrease homocysteine levels.
– DHA stands for docosahexaenoic acid and it is an omega-3 fatty acid found in animal products that plays a key role in the development of eye and nerve tissues. One can consume plant-based omega-3 fatty acid, alpha-linolenic acid (ALA), which the body will convert to EPA and DHA. Another option is to take an algae-based DHA supplement or eat a tablespoon of freshly ground flax seeds a day.
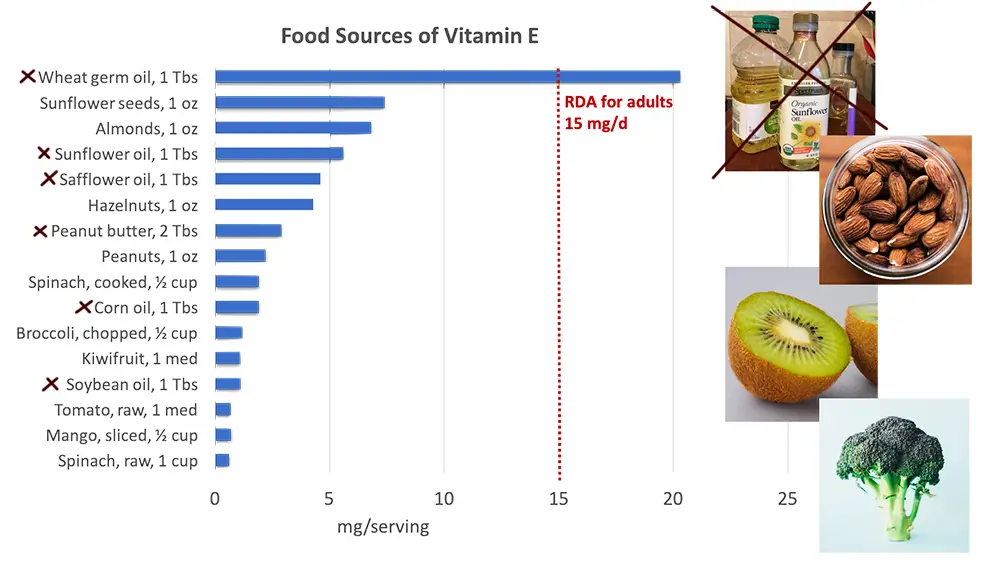
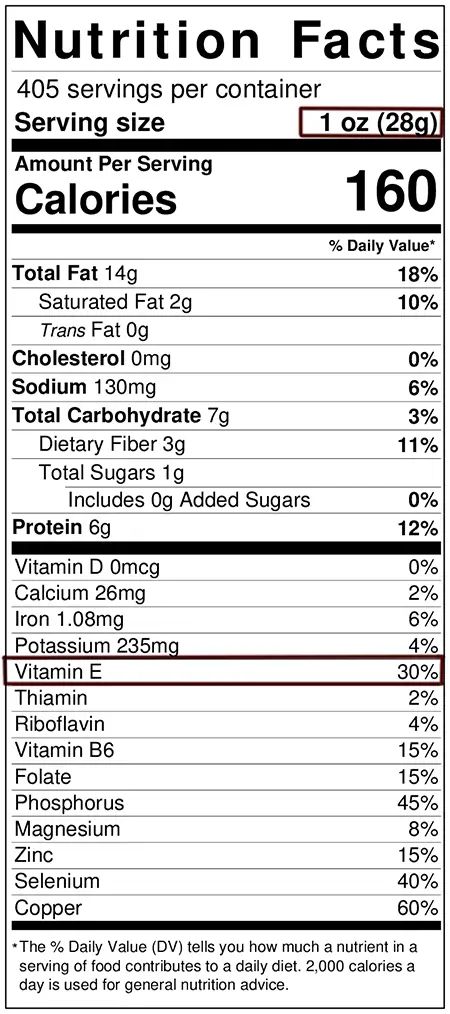
– Vitamin E is difficult to obtain as it only exists in fat, which is predominantly found in nuts and seeds. Additionally, exposure to air quickly oxidizes vitamin E making it unusable. The best option is to consume raw, whole, fresh nuts or seeds that are high enough in vitamin E as a source. Grounding these seeds should be done immediately before consumption without exposing them to oxygen. Sunflower seeds and almonds are good sources of vitamin E.
Diseases of affluence.
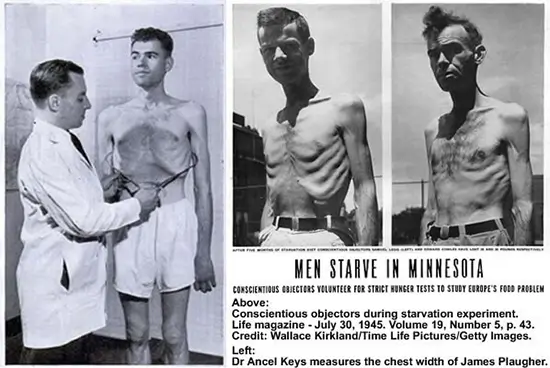
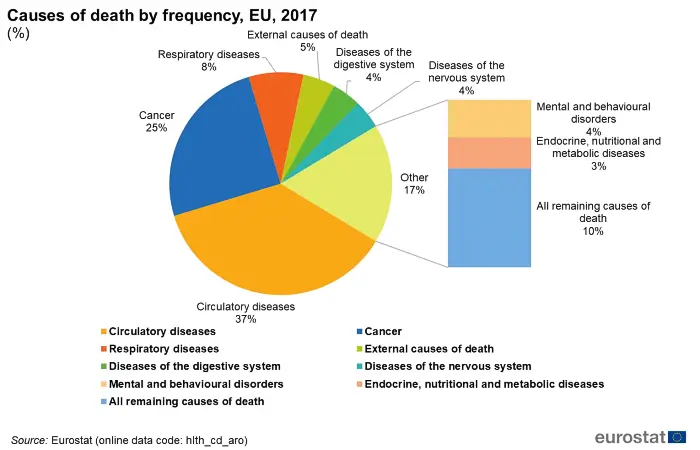
During the last decades, especially from the late 70s and the time of Mc Govern report onward standard Western diet has been acknowledged as a main source of all diseases of affluence like heart disease and stroke, cancer, and diabetes (Sinha et al., 2009).
Plant-based diet was proven to be associated with several beneficial health outcomes and in the last couple of decades has been adopted by an increasing portion of the population and individuals in Western societies, especially in times of chronic illness as a form of medicinal intervention.
A whole food plant-based diet is a diet that is congruent with the last 50 million years of our evolution. For 48 and something million years of our evolution, our body evolved on only fruits and green leaves.
A whole food plant-based diet is a diet that all of our hominin ancestors had and a diet that shaped our entire physiology. The influx of a couple of percent of calories from insects or some bone marrow is not enough to induce epigenetic changes that would translate into meaningful physiological adaptation in evolutionary terms.
Incongruent modern all-meat-you-can-eat diet was scientifically acknowledged to be a source of all, and I would repeat this because it is still a big problem for most people to hear.
Non-congruent evolutionary maladapted diet, meaning flesh and dairy and processed food, is the only, besides pollution, nutrient-depleted soil, and some other environmental factors, is the primary source of the epidemic of all of the diseases of affluence we have in the modern world.
For example, if you have a heart disease first thing you would or should do is to go on a full-scale plant-based diet and not take a statin. The same is for cancer or any inflammatory condition or autoimmune disease, chronic kidney disease, metabolic syndrome, or diabetes…. Today there are an ever-increasing number of individuals that have adopted a plant-based diet as a prevention from diseases of affluence and especially in the last decade or so influenced by the increasing availability of non-censored information provided by independent scientists and by publicly accessible databases like pubmed.gov. This is something that your doctor, allopathic medicine and big pharma cannot or are unable to suppress.
Nonetheless, there are still a lot of individuals that shifted to a vegan diet as a moral or philosophical issue. In this article, I would analyze common deficiencies in regard to whole food plant-based or vegan diets and not any type of other vegetarian-style diets. A plant-based diet can be a diet that may potentially include seafood (pescetarianism), eggs (ovo-vegetarianism), dairy products (lacto-vegetarianism), or both (ovo-lacto-vegetarianism). We also have to keep in mind that a vegan diet can be a junk food diet as well. Sugar is vegan so is refined oil.
Nevertheless, the number of individuals that truly adhere to a whole food plant-based diet is still almost insignificant compared to the rest of the population. Although the percentage of vegans has raised in the last decade dramatically, it has increased by 350% in the last ten years, still today it is only around 2 percent in Norden America. In Europe for example in Germany, it is only 0.1% to 1% of the adult population. Other studies involving countries worldwide have yielded inconstant prevalence rates within the general population: 0.77% in China, 0.79% in Italy, 1.5% in Spain, 3.8% in Norway, 4.1% in Finland, up to 11.2% in Australia, and 15.6% in Sweden. The highest percentage worldwide is in South Asia where around 33% of the population is vegan and this is influenced by both poverty and religious beliefs.
Plant-based diet
The vegan diet does not include products made out of animals and would have a much or completely different nutrition profile from the standard American diet. This is not some minor difference but an essential one.
First, the nutritional composition of macro and micronutrients would be completely different. This might not be such a big deal and would be beneficial for you if you eat more complex carbohydrates and starch and nutrient-dense food instead of sugar and fat.
Secondly and more importantly there are some nutrients that are only found or are found in not adequate amounts in one type of diet. There are nutrients that only exist in animal products or vice versa. This means that a plant-based diet would lack nutrients found in animals or would be lacking in them in optimal amounts if there are such nutrients.
This is actually good news because we are not omnivores physiologically only behaviorally. For example, real omnivores and carnivores do not produce their own cholesterol like plant eaters.
For carnivores and omnivores, cholesterol is an essential nutrient but not for us (Liscum et al., 2008).
We produce all cholesterol we would need our entire life. Any dietary cholesterol is an excess that needs to be detoxified. So a plant-based diet, for example, would be totally lacking cholesterol and in this case, because our number one killer is heart disease it would actually be a good thing. A cat as a carnivore for example would never be able to develop heart disease no matter how much cholesterol it consumes. On the other hand, the cat would produce their own vitamin C in their liver unlike us which is not a vitamin for them or any carnivore. Some other examples would be heme iron only found in flesh. On another hand, there are some other nutrients that are only found in animals that are essential and not found in plants and this is where we have a problem like vitamin B12 for example.
On the other side, there are nutrients only found in plants that are completely lacking in the animal kingdom, like already mentioned vitamin C, and this is a big problem for people eating the standard American diet.
Apart from the macronutrients, plants contain numerous phytochemicals (phyto means plant in ancient Greek), and some of them are essential for life like carotenoids, polyphenols, and other antioxidants.
Animal products are completely deprived of any type of antioxidants and are severely pro-inflammatory.
That is the reason why for example average goat is able to produce as much as 10 grams of vitamin C in their liver in one day if there is any type of stress to the body and the goat is a ruminant. There are thousands of different phytochemicals and all of them are biochemically active in the human body. Polyphenols found in grapes, berries, and nuts, indole-3-carbinol in cruciferous vegetables such as sprouts, cabbage, and cauliflower, isoflavones found in legumes, including clover, soy, and lupine, lycopene in tomatoes…. In general, these substances, are considered to have no additive nutritional value by allopathic medicine and are not considered to be vitamins, but they do have various metabolic pathways in the body, providing multiple health benefits. Lacking them always creates conditions such as chronic inflammation that can then lead to other conditions like cancer for example. More on deficiencies in the standard American diet can be found in this article (Micronutrient deficiency in Standard American Diet- The optimization strategies).
However, if a vegan diet is not appropriately planned and this mostly occurs in people that eat a vegan diet for moral reasons, reduction of caloric intake and nutritional deficiency of some vitamins like B12, and some minerals may appear. There are common deficiencies that affect both plant-based and standard American diets like iodine and vitamin D for example, and then there are deficiencies that are only affecting plant-based diets because of veganism itself, like B12 deficiency.
Vitamin D
Vitamin D is a common deficiency. It will affect everyone on this planet that do not run naked in the middle of the day in African savannas. If you wear clothes and live indoors you have vitamin D deficiency or insufficiency. Vitamin D is not a dietary vitamin at all. It does not have anything to do with diet. We can get some amount from the diet but in most cases, we will need to supplement. Vitamin D is not a vitamin but a steroid hormone that affects more than 2000 genes in our body and is produced when we expose our skin to strong and only strong sunlight. Sunbathing in five afternoons would do nothing even for pale-skinned individuals. This is a common deficiency and not specific to a plant-based diet. Depending on your weight and sun exposure you should take from 4000 to 5000 I.U. daily.
Iodine
This is one more universal deficiency. The theory goes that our ancestor hominin species survived by living close to the seashore and river deltas and have been eating a lot of greens from the sea instead of regular greens in Africa’s dry climate conditions after the shift.
As a consequence, we have an extraordinary requirement for iodine.
So much so that it is mandatory to be added to salt. The problem is that the amount you would get from salt is so minuscule that it would only prevent blatant iodine deficiency. That amount of iodine we consume from salt would be enough to only prevent blatant goiter and cretinism and nothing else. It is far from the optimal level of iodine intake. And what if you have heart disease or some other condition and your doctor tells you to avoid salt? Or what if you are pregnant?
The reason why iodine is deficient in most of the vegans and in the rest of the population is that vegans do tend to eat a lot of greens but do not eat a lot of sea green leafy vegetables.
Our body can hold a reserve of 1500mg of iodine.
That is milligrams, not micrograms. RDA for iodine is 140 micrograms. Our body would want to have a reserve of 1,500,000.00 micrograms and your doctor asks you to eat 140 micrograms in a day. It is a big subject that I would analyze in some of the upcoming articles. Most MDs have iodine phobia because they are scared of lawsuits and would rather let you suffer than let you know the truth and risk losing their license if something goes wrong. That is a reason they recommend the micro-dosing of iodine which has very little health effects except preventing blatant deficiency. You can start by watching this lecture.
Dr. Jorge Flechas – Total Body Iodine Sufficiency. Restorative Medicine, Portland, Oregon Conference 2011
Iron
Vegans have the opportunity to consume as much iron as non-vegans daily but because it is in hemoglobin the people subconsciously think that if they do not eat flesh they will be deficient in iron because they subconsciously believe that they are meant to eat meat because ‘humans are omnivores’.
Humans are behavioral omnivores, the same as chimpanzees, and not real anatomical ones with more than 50 million years on a green leafy vegetable diet and iron is exactly the proof of it.

Because we as vegan primates in our evolution had never consumed animal form of iron also known as heme iron our body never developed any enzymatic mechanism for controlling its levels. What this means is that our body does not have a control mechanism for removing it or not absorbing it. This is actually a selling point for paleo diet people. Heme iron or animal type of iron is more bioavailable because we did not evolve controlling mechanisms for its absorption not because it is somehow a superior form of iron. Our body is able to tightly control our iron blood levels when we eat green leafy vegetables only but when we eat meat all of that heme iron will go into the bloodstream even if it is not needed.
And you will say ok more iron what is the problem?
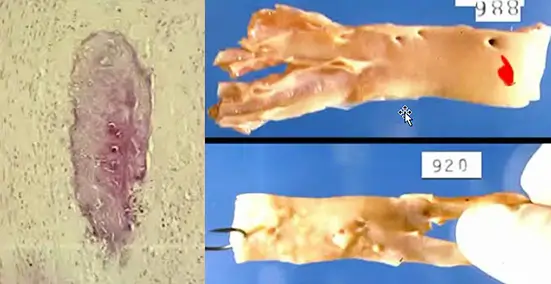
And there is a big problem. Excess iron is an inflammatory substance that acts in the same manner as any free radical (Emerit et al., 2001). Its main goal is to oxidase and carry oxygen in the first place. In recent years ferroptosis (excess iron-induced cell death) is correlated with many diseases as inflammation-induced cell death (Yu et al., 2021).
- Ferroptosis is closely related to iron and lipid metabolism and triggered by various physiological conditions and pathological stresses in human beings and animals.
- Ferroptosis connecting oxidative stress and inflammation play a key role in the pathogenesis of cardiovascular diseases such as atherosclerosis, stroke, ischemia-reperfusion injury, and heart failure.
Having excess iron or iron levels that are above the minimum required levels is not optimal, it is pro-inflammatory and inflammation is correlated to a vast range of diseases including cancer.
Our body will also have a hard time removing excess of that animal heme iron out once it gets forcibly and unnaturally absorbed from the meat. At a population scale, both iron and ferritin levels in the blood are lower in vegans than in non-vegans and this is actually a good thing, not a nutrient deficiency (Pawlak et al., 2016). Most nutritionists and doctors do not understand that having more iron is just having more inflammation and that our bodies have for millions of years developed mechanisms that allow us to not absorb excess plant-based iron if not necessary. The absorption of iron derived from heme is significantly higher compared to non-heme iron intake from plant foods and that is somehow turned into a selling pitch for we are omnivores propaganda. There is an easy fix for this if you believe that you need more iron for some reason.
In most cases, anemia is not caused by iron deficiency but this would be a subject for another article. Anemia in vegans is most likely caused by B12 deficiency number one, then zinc deficiency number two, and only then iron deficiency number three (Bachmeyer et al., 2019).
If you take a vitamin C pill or eat some products that contain ascorbic acid (citrus, strawberries, kiwi) you will increase iron absorption (Teucher et al., 2004), leading to uncontrollable all-you-can-get iron into the bloodstream.
If you have low iron in the bloodwork the cure is not to start eating meat or take an iron supplement. Iron as a supplement is iron oxide or in other words just regular rust or some other type of inorganic chelated iron that doctors will prescribe you to take. It is non-organic, non-bioabsorbable or even if you trick your body into absorbing it by chelation it would still be a nonbioavailable source of iron even if absorbed.
Legumes, beans, whole grains, integral cereals, dark-green leafy vegetables, fruits, seeds, and nuts can be used as sources of real organic iron. Avoid iron-fortified products as well.
The treatment is to take one vitamin C pill or 500mg after the meal and only after you had normalized your zinc and B12 levels first and still have iron levels below low normal value.
Watch the video below to learn how to extract iron from your morning cereals.
Zinc
Zinc is one other mineral besides iron that is not as easily absorbed from plant sources as it is from animal products. Vegans have shown the lowest zinc intake when compared to groups with different dietary habits (Bakaloudi et al., 2021). This still does not mean blatant zinc deficiency but it is somewhat consistent in plant eaters. A vegan diet is not necessarily zinc deficient, but it may require more attention to ensure adequate intake and absorption of this mineral.
In vegans, low plasma zinc levels can lead to iron deficiency anemia because zinc acts as a catalyst in iron metabolism (Kondaiah et al., 2019).
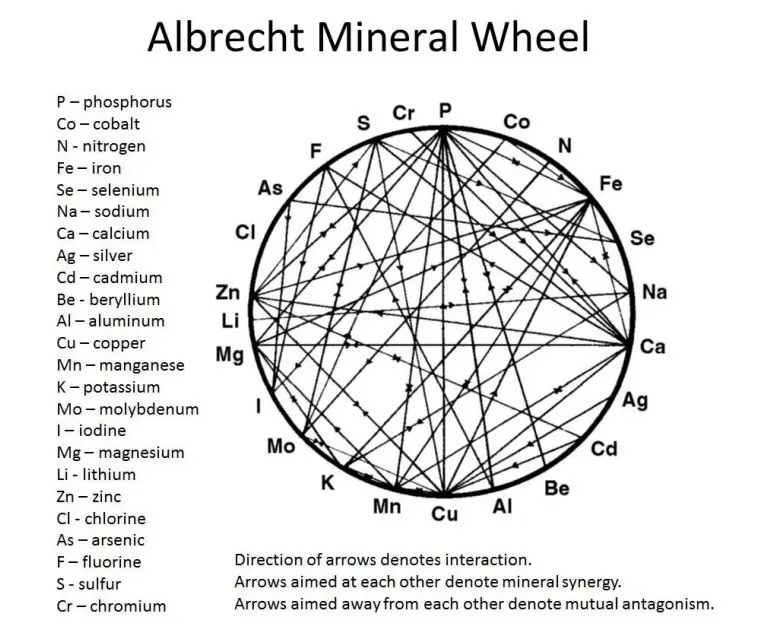
Mineral deficiencies always come as a complex mineral package that is not so easily corrected. In nature, food is a package deal.
Minerals never act alone but as a complex of different substances. Every mineral has opposing minerals and other synergetic minerals. All minerals also compete for absorption.
This is nature’s way of regulating mineral balance. But with eroded topsoil, everything is wrong and cannot be so easily corrected. You should first understand the mineral wheel if you want to correct mineral deficiencies. It is a vast subject. It should always be corrected with food, and not just any food but food is grown on mineral-rich topsoil with no synthetic fertilizers.
Zinc-rich plant foods are wholemeal bread, peas, corn, nuts, carrots, whole grains, wheat germs, soybeans, cabbage, radish, watercress, and legumes. Pumpkin seeds are good and one of the best sources of zinc. Eating pumpkin seeds for zinc is an easy solution especially because they are neutral tasting and can be added to any muesli or salad. In a normal situation one to two tablespoons a day would be enough to correct zinc deficiency.
However, in a situation where zinc deficiency is more severe, it might be necessary to take pumpkin seeds every day as a regimen. Although supplements can help correct deficiencies zink is inorganic non bioavailable metal, and it is important to remember that the best way to get the minerals your body needs is through eating a balanced diet. Eating a variety of nutrient-dense foods will help ensure you are getting all the essential minerals your body needs. Additionally, eating foods that are grown in mineral-rich soil is important too, as this will help increase the mineral content of the food. Eating organic is beneficial, as the mineral composition of topsoil would not be depleted by the use of synthetic fertilizers.
Some strategies to improve zinc intake and absorption on a vegan diet include:
- Eating a variety of zinc-rich foods throughout the day.
- Soaking, sprouting, or fermenting legumes, grains, and seeds to reduce phytate content (Saunders et al., 2013).
- Consuming foods high in vitamin C with zinc sources to enhance absorption.
- Using fortified foods or supplements if not recommended or needed.
The recommended dietary allowance (RDA) for zinc is 11 mg per day for men and 8 mg per day for women. However, some experts suggest that vegans may need up to 50% more zinc than omnivores due to lower bioavailability (Foster et al., 2013).
Therefore, a safe and adequate intake range for vegans could be 12-16.5 mg per day for men and 9-12 mg per day for women.
| Food | Serving size | Zinc (mg) | %DV(15 mg) |
|---|---|---|---|
| Pumpkin seeds | 1/4 cup unsalted, raw | 2.75 | 18.33% |
| Tofu | 1/2 cup | 2.4 | 16% |
| Lentils | 1 cup cooked | 2.3 | 15.33% |
| Sesame seeds | 1/4 cup unsalted, raw | 2.16 | 14.4% |
| Wild rice | 1 cup cooked | 2.1 | 14% |
| Oatmeal | 1 cup cooked | 2.1 | 14% |
| Cashews | 1/4 cup unsalted, raw | 1.82 | 12.13% |
| Chia seeds | 2 tbsp | 1.7 | 11.33% |
| Hemp seeds | 2 tbsp | 1.62 | 10.8% |
| Peanuts | 1/4 cup unsalted, raw | 1.61 | 10.73% |
| Sunflower seeds | 1/4 cup unsalted, raw | 1.33 | 8.87% |
Protein
One of the major non-concerns about the vegan diet is the lack of protein intake compared to the standard American diet. This was debunked repeatedly more than 50 years ago and ever since the “great protein fiasco” it was proven to be false in the scientific community. Still to this day allopathic medicine and media refuse to talk about real science and use protein as a holy cow of nutrition just to push for nonscientific forms of agenda and food pyramid.
And when this fails there is a second line of defense called the quality of a protein or its completeness and the content of essential amino acids.
Then the third line of defense is called digestive efficiency.
Majority of the vegetable products are characterized by low digestibility. It has been well documented that the presence of plant cell walls and antinutritional agents (enzyme inhibitors, tannins, phytates, glucosinolates, isothiocyanates), as well as food processing and heat treatment, may be inhibitory factors in protein digestibility. The only problem is that we do not need high dietary protein intake because we recycle all of our dead protein in the body. It is a process called autophagy (meaning self-eating).
When anthropology studies revealed that hominins could survive on an average of 15 to 20 grams of protein per day, this dealt the first blow to the cult of protein worship.
And some of these hominids were bigger and stronger than modern humans.
In evolutionary terms, protein requirements were much lower than those identified by modern science. There were just two choices available at that time. Either the protein requirements labeled by modern science are completely wrong or research in the field of anthropology about the protein requirements of hominids was completely incorrect.
In the 1970s, this led to the infamous “Great Protein Fiasco” (McLaren et al., 1974).
Big pharma and allopathic medicine did not like that. Human protein requirements underwent significant revisions and reductions. The alleged “world protein gap” was no longer mentioned (Semba, 2016). It vanished as if it had never existed. The daily protein requirement for an infant, for instance, was 13 percent of calories in 1948 and 5.4 percent of calories in 1974. The average American today may regularly consume more than 90 grams of protein each day.
What do you suppose our daily protein intake was before technology made it possible for people to go above 40 parallel?
The short answer is between 15 and 20 grams each day. And all the protein, or at least 97% of it, was derived from plants, with only around 3% coming from animals.
According to anthropological research, the protein was never ingested in the same quantities as it is today during the majority of the evolution of hominins. And there is a simple reason, our ancestors didn’t have spears or traps or fire or any other technology. Only anatomically modern humans have started to use bows and arrows, spears, and traps to hunt. Homo Erectus didn’t.
Also, every species of hominid and every primate was vegan. How then can we survive on low-quantity and low-quality protein sources? Because there is scarcity in nature, our bodies have evolved to preserve all that can be preserved.
Our body saves protein. It is the process of autophagy.
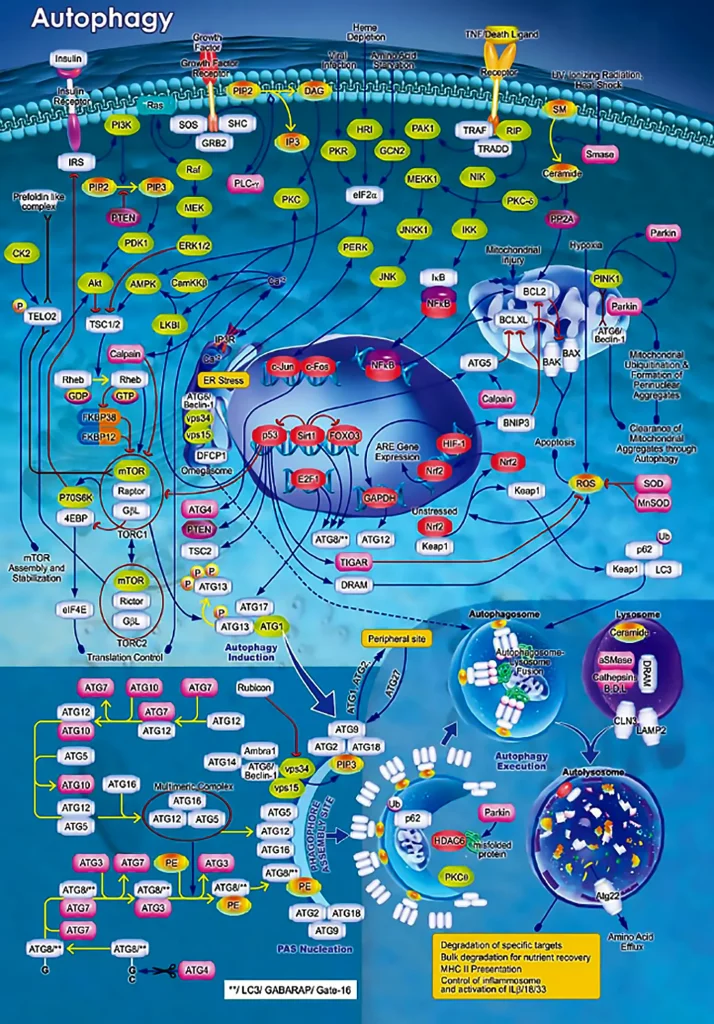
This means that you eat yourself every day. Auto means oneself, whereas phagy means to eat. Every day, we eat ourselves. Each and every one of our body’s cells are composed of proteins, and when a cell dies, it gets recycled. And this is actual recycling that is 100% effective. The only cells that we physically lose are those that cannot be recycled, such as hair, nails, and skin, which literally physically depart from our bodies. Everything else is recycled.
Protein is not necessary for life. Protein is recycled. The protein that has been lost from our bodies as dead skin, hair, and nails has to be replaced. It amounts to a few grams in a single day.
Milos Pokimica
That is the truth.
Constant overfeeding on high-quality protein on the other hand has serious health implications.
One of many is, for example, the epidemic of cancer. When we consume a high-protein diet as a result the levels of amino acids circulating in our bloodstream are constantly elevated. Then our body starts to release the IGF-1 hormone into the bloodstream. That is a hormone that gives a signal to cells to repair and divide if they need to. The normal cell will do nothing but the cancer cell will do a lot. There is a greater correlation between IGF-1 level and cancer progression than there is between smoking and lung cancer.
The second effect of overconsumption of protein is the instant and complete shutdown of autophagy. Our body evolved to preserve energy because, for most life on this planet, food is not a choice, and starvation and death are the normal forms of existence. This means that if there are pre-cancerous mutations or any type of damage in our cells they are not going to be instructed to go to cell death as long as there is no starvation. Our body is going to keep them alive waiting for the next drought to be used as a source of energy. Think of it this way. If there is starvation and some cells must go first on the line are damaged pre-cancerous cells. On the other hand, the complete lacking of any form of starvation in the modern way of life with constant overfeeding on high protein food sources is not congruent with starvation and scarcity of our ancestor’s environment. Maladaptation in time will create a rise in all forms of correlated diseases of affluence. Cancer is one of them.
This also means that even if you eat a whole food plant-based diet you will need to incorporate intermittent fasting to reap all of the benefits.
Also, this means that consuming too many plant proteins as well, for example, overconsumption of legumes especially consumption of soy, will negate some of the benefits that a vegan diet has on cancer prevention and longevity.
High IGF-1 levels will shorten lifespan significantly not just from cancer but from metabolic disorders and accelerated aging also (Kubo et al., 2022). Keep this in mind if you want to reap all of the health benefits of plant-based eating the next time someone or your doctor asks you where did you get your protein?
Even in allopathic medicine consensus is that in general, if certain plant foods are consumed in appropriate combinations, they can provide all the essential amino acids for human nutrition, although some of them may be absent in certain plants, including for example lysine in cereals, rice, and corn, and methionine in legumes. Even in allopathic medicine consensus is that if we just consume any whole food source no matter what it is including potatoes, corn, rice, or carrots, and if we have enough calories from that whole food source for sustenance without consuming empty calories like sugar or oil, we would get enough of essential amino acids in the diet. This is for whole food only not vegetable juices. Having a constantly high level of protein in the diet on the other hand leads to serious health implications that you can read about in more detail in correlated articles.
Calcium
Calcium intake in the majority of vegans was below recommendations (750 mg/d). This is a concern for people that believe that dairy is the main source of calcium in the western style diet and that without dairy there must be a calcium deficiency. And this is not correct.
Most of the human population is lactose intolerant.
Lactose tolerance first emerged in around 2700b.c in parts of central-eastern Europe and then started to spread. There are abundant plant-based sources of calcium. The concern was raised because of calcium bioavailability that is inversely proportional to the amounts of oxalate, and to a lesser extent, to phytate and fiber found in vegetables. High-calcium foods include green leafy vegetables, sesame seeds, poppy seeds, tofu, tahini… Fortified foods such as cereals, soy, rice, almond and coconut beverages, orange and apple juices are not good sources of calcium because only organic calcium is bioavailable and even bioabsorbable from the gut in the first place. Chelated calcium is bioabsorbable because we will trick our body to pull it inside with the chelated agent but once in the bloodstream it will still not be bioavailable for biochemical processes.
Only organic calcium is truly bioavailable to the cells in our body.
Nevertheless, the best absorption and utilization of calcium is provided by low-oxalate vegetables, including broccoli, kale, turnip greens, Chinese cabbage, bok choy, and seeds like sesame and poppy. For 100 grams of raw sesame seeds, we will have 975 milligrams of calcium. For 100 grams of raw poppy seeds, we will have 1438 milligrams of calcium. One liter of milk has 1250mg of calcium.
Most people are afraid of calcium loss because of osteoporosis. Keep in mind that African women do not get osteoporosis on 350 mg of calcium a day. Osteoporosis affects dairy queen countries the most.
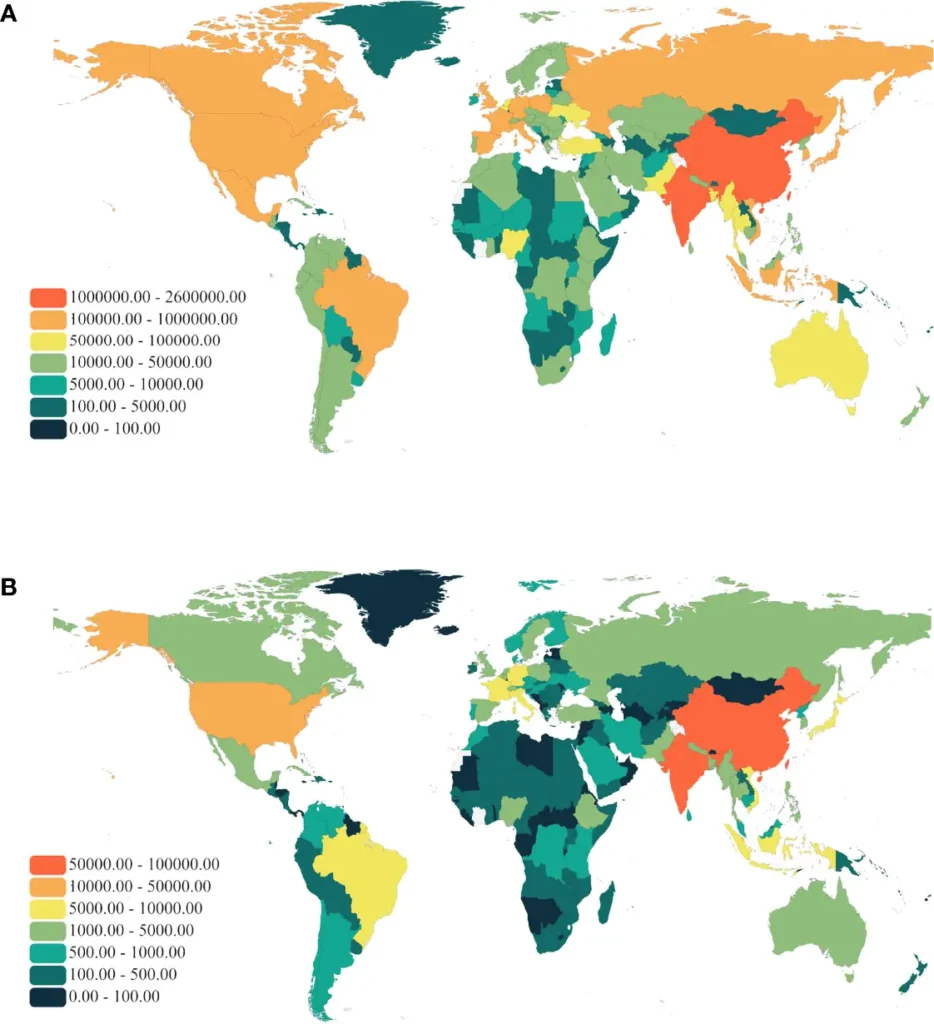
Osteoporosis is not a calcium deficiency disease. As you can see on the map. Africans are 99 percent lactose intolerant. The same is with Native Americans. In India and China, they have a big problem with heavy metal pollution and especially with metals that cause the weakening of bone structures like cadmium and lead.
Osteoporosis is a vitamin D chronic deficiency disease. And even this is not completely true. If you have vitamin D deficiency for your entire life and then when you turn 60 you start to suffer from bone demineralization in most cases it is already too late.
The reason why osteoporosis is most prevailing in the most developed countries and not in poor countries in lactose intolerant people is that those people eat much more vegetables.
In most cases, osteoporosis in Western countries is a consequence of magnesium deficiency, not calcium deficiency.
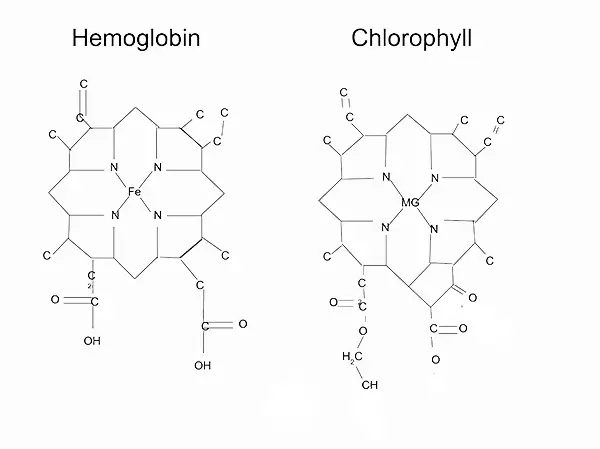
Magnesium is one of the most common and prevailing deficiencies in non-vegan diets because magnesium is mostly found in plant foods. The difference between chlorophyll and hemoglobin is only in oxygen carrier. In hemoglobin, it is iron in chlorophyll it is magnesium. The molecule is the same only the mineral carrier is different.
The problem for the average meat eater is that magnesium is needed for more than 300 enzymes in the human body and one of those enzymes is the enzyme that regulates calcium metabolism. Magnesium deficiency and to an extent vitamin D deficiency are the sources of the emergence of osteoporosis in dairy-dominated diets of the West.
Milos Pokimica
WHO to this day has more sensible recommendation that is designed for the world population’s dietary habits more than for the dietary habits of just America and Europe. WHO recommends around 400 to 500 milligrams of calcium as an optimum per day. In contrast that the US has a recommendation and this is the highest calcium recommendation in the world for no less than 1000mg per day. Ideally 1250mg for adolescents. Most studies have shown that about 500mg is enough for healthy bones. If you consume around 800 to 900 you are already entering the calcium toxicity zone.
Too much calcium leads to too little magnesium because, on the mineral wheel, magnesium and calcium are opposite minerals.
You can pick and choose your calcium authority but my suggestion is to not aim at more than 1000mg of calcium from whole food sources only.
Never consume calcium-fortified food or take calcium as a supplement because calcium spikes in the bloodstream can cause calcifications in the arteries and will coagulate your blood which can lead to calcium thrombosis (Peng et al., 2021).
Peng et al. (2021), examined the risks of individuals with very high coronary artery calcium (CAC) score (≥1000) compared with those with lower or no CAC score. The study used data from MESA (Multi-Ethnic Study of Atherosclerosis), a prospective, observational, community-based cohort of 6814 ethnically diverse individuals who were free of known cardiovascular disease. The main findings of the study were:
- Compared with CAC 0 and CAC 400 to 999, CAC ≥1000 was associated with increased risk for all cardiovascular disease events, all coronary heart disease events, hard coronary heart disease events, and all-cause mortality.
- Compared with CAC 0 and CAC 400 to 999, CAC ≥1000 was also associated with an increased risk for a first non-cardiovascular disease event.
- CAC ≥1000 corresponded to an annualized 3-point major adverse cardiovascular event rate of 3.4 per 100 person-years.
The article concludes that individuals with very high CAC scores have a high burden of subclinical atherosclerosis and are at increased risk for cardiovascular and non-cardiovascular outcomes.
My suggestion is to never drink calcium-fortified vegan milk and if you do drink them never drink more than one cup in a single sitting. Calcium-fortified soy or almond milk is basically a calcium supplement.
| Food (100 grams) | Calcium (mg) | % DV |
|---|---|---|
| Poppy seeds | 1448 | 145 |
| Sesame seeds | 975 | 98 |
| Tahini | 426 | 43 |
| Spinach | 99 | 10 |
| Kale | 150 | 15 |
| Tofu (prepared with calcium) | 350 | 35 |
| Soybeans | 277 | 28 |
| Figs (dried) | 162 | 16 |
| Bok choy | 105 | 11 |
| Almonds | 264 | 26 |
Vitamin K2
In recent years paleo diet people managed to find a new “key” ingredient besides protein to act as a holy caw of “we are the omnivore species” propaganda. And that is vitamin K2 only found in animal products. As such it must be proof that we are not anatomically designed to eat a plant-based diet. Well wrong. Vitamin K2 is actually not a vitamin. Sorry.
Vitamin K1 is a real vitamin but K2 is not.
The vitamin is classified as a vitamin because our body needs to get it from diet and is unable to make it by ourselves. Vitamin C is a vitamin for us but not for any carnivore species on this planet because they make their own vitamin C thus it is not a vitamin. Cholesterol is a vitamin for them but again it is not for us. The human liver unlike the liver of omnivore and carnivore species makes cholesterol. Cholesterol thus is not a nutrient for any plant eater out there. The same is with creatine. We make our own. And the same with K2.
Our bodies make K2 from vitamin K1 which is found in plants.
The main selling pitch here is that higher K2 levels were connected to lowering cardiovascular risk but only if we disregard all of the cholesterol and inflammation that comes along with meat consumption. If you want to increase your K2 levels independently from K1 then you can just eat some natto that is fermented soybeans and very rich in K2 or some other fermented vegetables like sauerkraut. In Serbia and in most Slavic countries sauerkraut is traditionally made and eaten during winter in most households but is not as great of a source of K2 as kimchi or natto. In Western countries Korean kimchi is more popular, and you can start to incorporate kimchi into the diet if this K2 thing really bothers you. Fermented vegetables are also one of the best sources of probiotic bacteria but you will have to make them yourself. If you find fermented vegetables in the store, any store, supermarket, or farmer’s market, all of the fermented vegetables have to be pasteurized by law before they can be sold. There will be no living bacteria in them, so if you want probiotic bacteria and K2 you will have to learn how to ferment them yourself.
| Food (100 grams) | Vitamin K2 (mcg) | % DV |
|---|---|---|
| Natto | 1103 | 919 |
| Kimchi | 65 | 54 |
| Sauerkraut | 4.8 | 4 |
| Tempeh | 3.5 | 3 |
| Kombucha | 0.5 | <1 |
| Miso | 10 | 8 |
| Vegan cheese (made from fermented nuts) | 8.5 | 7 |
| Pickles | 4.5 | 4 |
| Vegan yogurt (made from fermented soy or coconut) | 3.5 | 3 |
| Vegan kefir (made from fermented grains or nuts) | 3.2 | 3 |
| Vegan vitamin K2 drops (made from fermented natto) | 1000 per drop | 833 |
This is the classic, spicy, traditional napa cabbage kimchi called tongbaechu-kimchi, aka baechu-kimchi, or pogi-kimchi. But this dish is so common that most Koreans simply call it “kimchi.” When people talk about kimchi, this is the dish they’re referring to!
Vitamin B12
People may easily see how a change in our way of life has contributed to the persistent and widespread vitamin D insufficiency that affects the majority of the population. We have left the warm climate conditions of Africa, where we have been evolving for 50 million years, and are now in the cold climate of the northern hemisphere, where there is no sunshine. We live indoors and use clothing to stay warm.
However, what about vitamin B12?
I’m frequently asked about it. If we are evolutionarily predisposed to be herbivores, how is it that B12 is exclusively found in animal products and not in plant foods?
There is an easy explanation for this. This vitamin is produced by a particular type of bacteria, not by plants or animals.
We have that type of bacteria in our colon and we produce B12, but there is an issue that prevents B12 from functioning as a vitamin for us. B12 is not available for absorption since it is generated below the ileum, which is where B12 is absorbed. B12 is created, however, it is excreted out rather than absorbed. In evolutionary terms, it is not a vegan diet that is a problem but an increase in sanitation. Under normal circumstances, we wouldn’t be able to wash our hands and would drink contaminated water. For instance, chimpanzees would touch their waste before eating fruit with the same hand.
This enables them to get B12 while eating a plant-based diet. Since we no longer do that and have sanitation, we do not consume enough of that vitamin. We don’t contract cholera either.
An evolutionary incongruent environment with clean water, rather than an incongruent diet, is to blame for the B12 deficiency in vegans.
In a couple of studies done on the issue of B12 deficiency, almost half of the vegans had severe deficiencies and 20% had low levels. They don’t take B12 pills, which explains this result. You must take B12 if you are a vegan. Even vegetarians are only 76 percent sufficient (Gilsing et al., 2010).
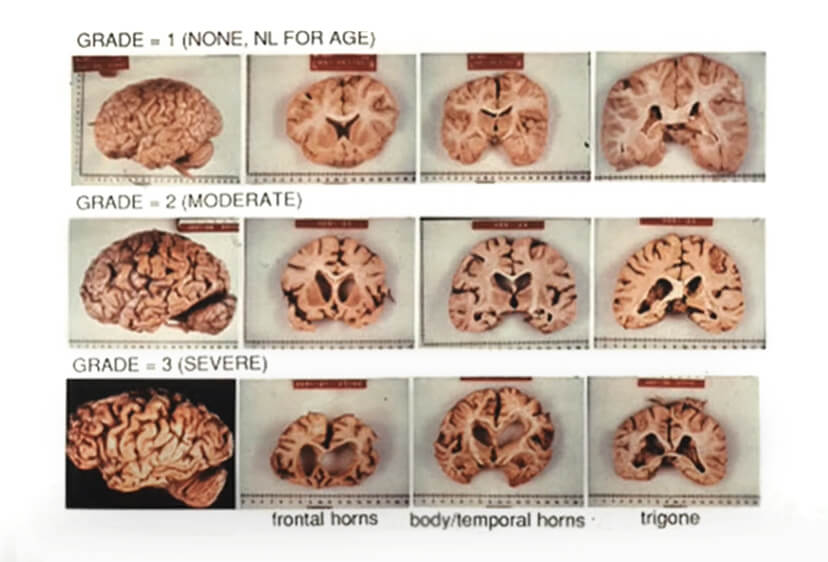
B12 is a crucial vitamin for the body’s numerous processes, particularly for the development of red blood cells and the health of the nervous system and the brain. Anemia is one result of a B12 deficiency, and most of the time it is not iron deficiency as most vegans believe. Also, adequate levels of B12 will slow down cognitive decline in aging. Around 1 in 5 persons over the age of 70 have cognitive deterioration without dementia, and this will develop to 12 percent having full-blown dementia and dying. Age-related brain cell loss is referred to as cognitive decline. To some extent, this is “normal”. It is a type of preventive strategy for Alzheimer’s disease rather than a complete cure.
This is due to the fact that B12 is crucial for regulating homocysteine levels in the brain. B12, folate, and B6 are the three vitamins that regulate homocysteine levels. Most non-vegans consume adequate amounts of B12 and B6, but not nearly enough folate. Contrarily, the majority of vegans consume more folate but, without supplements, have no B12 at all and this will drive homocysteine levels sky high, stroke risk levels high, brain turned into mush high.
Most meat-eaters when measured in studies have homocysteine levels of around 11 because they don’t consume enough folate, which is mostly found in green leafy vegetables and beans and they consume too much methionine. In America, more than 96% of individuals do not consume even the smallest amount of greens and beans, leaving them with a homocysteine level of 11 µmol/L.
Also, the majority of methionine is found in animal protein. It is an essential amino acid in humans and homocysteine is a byproduct of methionine metabolism. Yet, when we look at long-term vegans, their homocysteine levels are horrendous.
In this study (Obersby et al., 2013), homocysteine levels were 16.41 in vegans, 13.91 in vegetarians, and 11.0 in omnivores. Nevertheless, vegans can fully benefit from their diet if they take B12 supplements. Then their homocysteine levels will fall below 5.
Most people don’t actively measure their homocysteine levels or are not familiar with the subject. Yet, it is a fatal condition that, if not treated can develop into a major chronic illness with long-term effects.
High homocysteine levels are one of those conditions that will be subclinical and by the time the first symptoms appear, it will already be too late. Damage has already been done.
My recommendation is to take your B12. Also, the risk-benefits ratio in further downregulating homocysteine levels goes in creatine’s favor as a longevity supplement. Creatine might help you work out as well.
Creatine
You might hear of creatine as a bodybuilding or as a general sports supplement. It is not a vitamin because our own bodies make it. We do not need to supplement with it or take it. It is not essential and yes it is only found in meat. So vegans will have lower levels than meat eaters. Also for this same reason, additional supplementation for meat eaters will have much less of an additional benefit than for plant eaters because people that do consume meat already consumed much more creatine than normal and are to some extent saturated. The body has a level of saturation. When reached any additional creatin is exerted out through the kidneys. In bodybuilding when you start to supplement with creatine you will first do a loading phase to quickly saturate your body and then you will go into a maintenance phase with no more than 5 grams of creatine per day. For some people, creatine supplementation will do nothing. They are so-called non-responders. And this is a people that consume too much creatine from meat already. But for vegans, it is a different situation.
A plant-based diet is completely deprived of creatine and in vegans, creatin is made only internally.
The problem with creatine is that when our bodies make it, homocysteine is also created as a by-product.
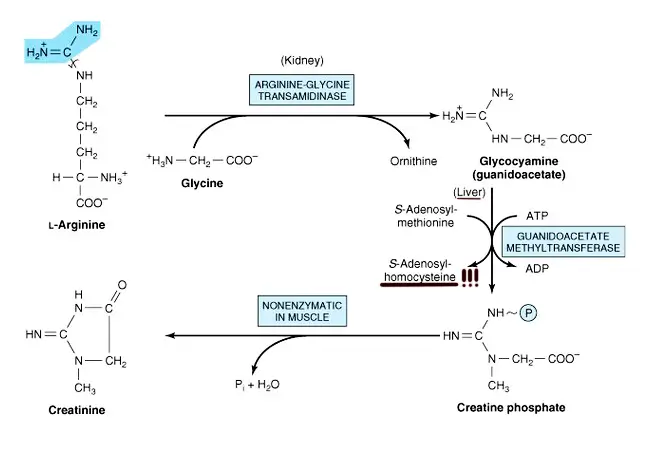
The reasoning goes that if we take creatine as a supplement we will downregulate the need of our body to make it internally and as a consequence will have lower levels of homocysteine.
In this study (Van Bavel et al., 2019), individuals who solely consume a plant-based diet and who do not supplement with vitamin B12 were examined. They had the highest homocysteine levels possible. Even greater than 50 was seen in some subjects.
They didn’t receive B12 supplements only creatine. Their levels gradually decreased and did reach a normal level of approximately 10. This is just supplemental creatine by itself. Additional B12 will bring this level much lower. Currently, I was unable to find any studies on this particular topic, so I’m offering this advice to anyone looking to write their Ph.D. dissertation: look for vegans that don’t take B12 supplements, and then give them both B12 and creatine and measure their homocysteine levels.
Omega-3 fatty acids
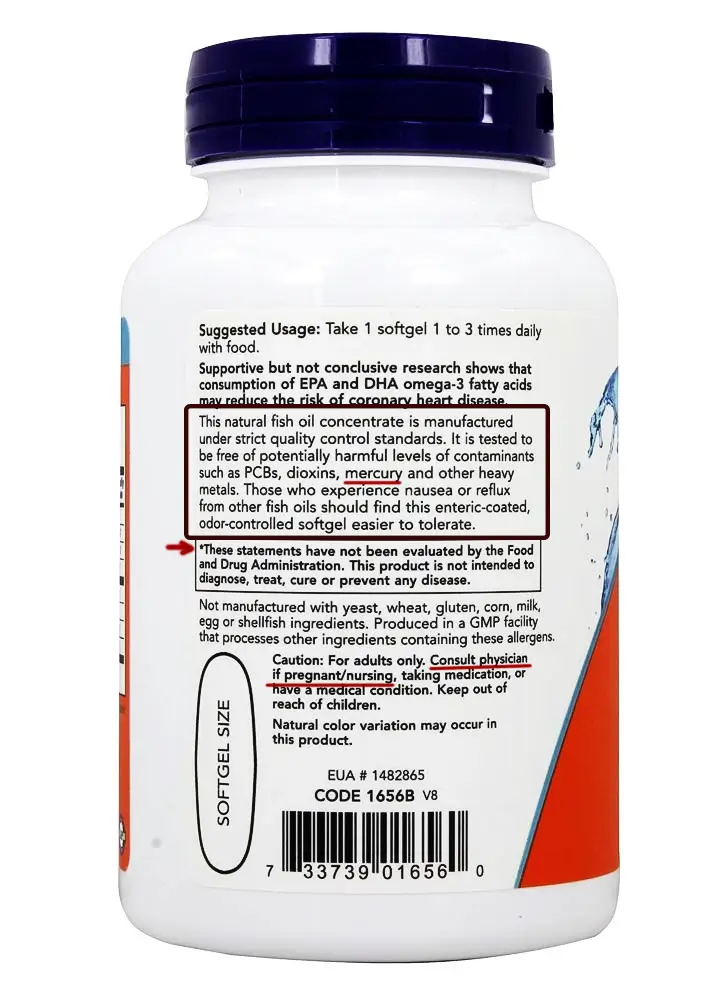
DHA is one more substance that is important for preventing cognitive decline. DHA stands for docosahexaenoic acid and EPA stands for eicosapentaenoic acid. Both are omega-3 fatty acids. And both are only found in animal products. Plant-based omega-3 fatty acid is alpha-linolenic acid (ALA), which the body will convert to EPA and DHA.
DHA plays a key role in the development of eye and nerve tissues (Lafuente et al., 2021). DHA might also reduce the risk of heart and circulatory disease by decreasing the thickness of the blood, reducing swelling (inflammation), and lowering blood levels of triglycerides (Holub, 2009).
In some research blood viscosity of people living in the Artic circle was so low that their wounds wouldn’t heal and the bleeding from a small cut will last for more than 20 minutes because of the all of DHA that they overconsumed. They were at risk from cardiac pathophysiology. The combination of tissue hypoxia and reduced blood viscosity leads to decreased systemic vascular resistance. The body responds to decreased systemic vascular resistance by increasing sodium and water retention resulting in an increased stroke volume and cardiac output.
In the standard American diet on the other hand people do not get an adequate amount. You will have to consume some form of omega-3 fatty acid. If you don’t eat fish which is the number one most toxic meat in existence and the number two pro-inflammatory meat after chicken then you will have to find a source of ALA. You can supplement with fish oil but the fish is extremely polluted with not just mercury but PCP-s, DDT, and all other persistent organic pollutants. The problem was that consumers were starting to become aware of these contaminants. Then the industry tried to clean up this oil by offering a molecularly destined fish oil with the claim that it is free from pollution but when tested independently it was proven to be marginally cleaner and this can be a ground for a lawsuit against the industry.
Then they tried to offer an omega 3 oil from species that are lower on a food chain like krill omega 3 oil which has been tested to be purer than fish oil and even more pure than molecularly destined fish oil. But then again the question arises.
Why won’t you go down all way to the bottom of the food chain and just get an algae-based DHA supplement? Fish and shrimp get their omega-3 from algae in the first place.
Another option will be just to eat a tablespoon of freshly ground flax seeds a day.
And this is if you don’t consume refined polyunsaturated oils like sunflower oil. If you do use vegetable oils then you would need to take more ALAs or go to the supplemental root. The problem is conversion. It is not natural to consume oil in refined form.
The enzyme that converts ALA to EPA and DHA , delta-6-desaturase (D6D), will also bind to polyunsaturated fatty acids. It does have around six times more affinity to ALA (Gerster, 1998) but if there is a lot of polyunsaturated oil in the bloodstream it will oversaturate the enzymatic pathways in the body.
That is the reason you will see a different rate of ALA conversion in different individuals. All the talk of omega 3 to omega 6 ratio is because the enzyme will bind to both of them and this is a problem when we introduce refined omega 6 oil into the diet. On average, 1–10% of ALA is converted into EPA and 0.5–5% into DHA. That is 10 times the difference in individuals and all because of the refined oil.
We need from 300mg to one gram of DHA per day. At a conversion rate of 0.5%, we will need to consume from 6000mg to 20000mg of ALA. To consume 20 grams of omega 3 oil will be to consume around 50 grams of ground flaxseeds in a day for a high-end estimate. This will represent a significant number of calories as well. This is for a 0.5% conversion. For a 5% conversion, it will be 5 grams of flaxseeds per day for 1 gram of DHA. For a minimal RDA of 300mg, we will need 10 grams of flaxseed for the high end or 1 to two grams for the low end. And all of this is very confusing.
Range goes from 2 grams to 50 grams of flax per day. Maybe some chia pudding with some walnuts and maybe some algae-based DHA supplement if you have money. You shod incorporate flaxseeds into the diet for their lignan content regardless of omega 3s. Lignans have a positive effect on the lipid profiles of patients with dyslipidemia-related diseases. Dietary intake of lignans is also associated with reduced cancer and cardiovascular disease risk and lowered inflammation. But there is one big but here.
ALA is the most sensitive oil for oxidation of all oils in existence.
As soon as it gets exposed to oxygen in the air it will oxidase and become rancid. Never under any circumstances consume flaxseed oil or any other omega-3 oil. Never buy or consume pre-grounded flaxseeds or any other omega-3-rich seeds.
If you want to eat flaxseed grind them for yourself. Also not too much, and use them immediately. Do not add them to blenders if they are not vacuum blending types. Grind them as little as it is necessary and eat them immediately. Do not put them in the fridge for later. Eat them immediately or throw them away.

Vitamine E
Even with a whole-food plant-based diet, vitamin E is extremely difficult to obtain in adequate amounts. This is one of the universal deficiencies. The majority of us who do not actively try to address vitamin E deficiency will most likely end up having insufficient consumption. Actually, the vitamin known by the name vitamin E is just one of a group of eight compounds. All of them are fat-soluble antioxidants: four tocopherol isoforms (α-, β-, γ-, and δ-tocopherol) and four tocotrienol isoforms (α-, β-, γ-, and δ-tocotrienol). Only one form, α-tocopherol, is classified as vitamin E. The other tocopherols nonetheless also have biological actions in the human body.
Since oil and water don’t mix our bodies require vitamin C for the water and vitamin E for the fat parts of our cells as a defense against free radicals. Organs comprised of fat, such as the brain, are particularly susceptible to inflammation brought on by a vitamin E shortage.
This is one of the deficiencies that will remain undetected for a long time creating DNA damage before manifesting itself as a chronic disease. At that point, the damage has already been done.
As vitamin E is a fat-soluble antioxidant and it can only be found in fat.
The only food therefore that will have it is one that stores energy in the form of fat. This will be predominantly nuts and seeds. Also because vitamin E is an antioxidant if it gets exposed to the air it will oxidase and the oil will become rancid. The number one source of vitamin E in the Western diet is exactly vegetable oil. This is one big fat lie designed to fool you.
Vitamin E is very hard to get because vitamin E as a fat-soluble antioxidant only exists in fat. And because it is an antioxidant it reacts to oxygen in the air so if we have any vitamin E exposed to air it is gone. Oil is rancid. End of story.
The number one source of vitamin E in the Western diet is exactly vegetable oil. This is one big fat lie designed to fool you. Nutrition labels will list vitamin E from rancid oil as a reliable source in the diet. This also applies to grounded seeds.
Even if you use a home oil extraction to obtain fresh oil, as soon as the oil is extracted, the vitamin E content is drastically reduced. You should use it immediately. This also applies whether you ground your own seeds, use a blender, or engage in any other method of exposing vitamin E and other antioxidants to the air.
And what do the majority of people do with oil?
It is used for frying, cooking, and baking. Heat speeds up oxidation, so say goodbye to any vitamin E content when using oil in the kitchen. You have rancid oil that is pro-inflammatory, carcinogenic, and mutagenic, and whatever you use to fry in it is also carcinogenic. Because it has a greater smoking point than polyunsaturated fat, saturated fat is more stable when deep-fried. Vegetable oils are only listed as a source of vitamin E in paper statistics. If you know anything about nutrition you would know that this is a lie. This is actually done on purpose to avoid fully freaking off the public because there are no easy fixes for this.
They will use vitamin E in fortified foods and count that as a source, which is the second reason you don’t see widespread vitamin E deficiency. And here’s is the truth: Industry cannot produce vitamin E with the exact same molecular structure in laboratories because it would be too costly. They are marketing supplements that aren’t actually vitamin E as vitamin E.
Natural α-tocopherol made by plants found in food has an RRR-configuration at the 2, 4’, and 8’-position of the α-tocopherol molecule (wrongly referred to as d-α-tocopherol). Chemically synthesized all-rac-α-tocopherol (all-racemic-α-tocopherol; incorrectly labeled dl-α-tocopherol) is a mixture of eight stereoisomers of α-tocopherol, which arose from the three chiral carbons at the 2, 4’, and 8’-positions: RRR-, RSR-, RRS-, RSS-, SRR-, SSR-, SRS-, and SSS-α-tocopherol. While all stereoisomers have equal in vitro antioxidant activity, only the forms in the R-conformation at position 2 (noted 2R) meet the vitamin E requirements in humans.
It’s nothing new, really.
Synthetic vitamin E has no antioxidant capability in vivo (Pearson et al., 2006). According to Pearson et al. (2006), it was noticed that plasma oxidation activity actually increases by 27% in people who are given Vitamin E supplementation.
Everyone in the fields of nutrition and medicine is aware that synthesized vitamin E has no antioxidant activity in vivo. It is a phony vitamin supplement that is added to infant formula. In recent years there has been a string of research that showed an increase in mortality with the use of synthetic vitamin E.
In the best-case scenario, synthetic vitamin E pills are just a complete waste of money. In the worst-case scenario, those who use it could actually be paying to live shortened lives.
The only real option is to have nutritional optimization. We require full not pre-ground, raw, fresh nuts or seeds that are high enough in vitamin E as a source. And if you look at the nutrition charts only available option is sunflower seeds and almonds.
All other seeds have considerably lower levels of vitamin E. It would take at least 40 grams of raw sunflowers seeds to correct vitamin E deficiency per day. And this means 40 grams of raw, whole, sunflower seeds, every single day, for the rest of your life.
Conclusion:
- Standard western diet has been acknowledged as a main source of all diseases of affluence like heart disease and stroke, cancer, diabetes…
- A whole food plant-based diet is a diet that is congruent with the last 50 million years of our evolution.
- The number of individuals that truly adhere to a whole food plant-based diet is still almost insignificant compared to the rest of the population.
- The vegan diet does not include products made out of animals and would have a much or completely different nutrition profile from the standard American diet.
- The nutritional composition of macro and micronutrients would be completely different.
- Secondly and more importantly there are some nutrients that are only found or are found in not adequate amounts in one type of diet.
- For carnivores and omnivores, cholesterol is an essential nutrient but not for us.
- Apart from the macronutrients, plants contain numerous phytochemicals (phyto means plant in ancient Greek), and some of them are essential for life like carotenoids, polyphenols, and other antioxidants.
- Animal products are completely deprived of any type of antioxidants and are severely pro-inflammatory.
- Vitamin D is a common deficiency. It will affect everyone on this planet that do not run naked in the middle of the day in African savannas.
- Iodine is one more universal deficiency.
- Our body is able to tightly control our iron blood levels when we eat green leafy vegetables only but when we eat meat all of that heme iron will go into the bloodstream even if it is not needed.
- Having excess iron or iron levels that are above the minimum required levels is not optimal, it is pro-inflammatory and inflammation is correlated to a vast range of diseases including cancer.
- In most cases, anemia is not caused by iron deficiency but this would be a subject for another article. Anemia in vegans is most likely caused by B12 deficiency number one, then zinc deficiency number two, and only then iron deficiency number three.
- Vegans have shown the lowest zinc intake when compared to groups with different dietary habits.
- Minerals never act alone but as a complex of different substances.
- Every mineral has opposing minerals and other synergetic minerals. All minerals also compete for absorption.
- According to anthropological research, daily protein intake before technology made it possible for people to go above 40 was parallel between 15 and 20 grams each day.
- Our body saves protein. It is the process of autophagy.
- The protein that has been lost from our bodies as dead skin, hair, and nails has to be replaced.
- Constant overfeeding on high-quality protein on the other hand has serious health implications.
- If you eat a whole food plant-based diet you will need to incorporate intermittent fasting to reap all of the benefits of cancer prevention and longevity.
- Consuming too many plant proteins will negate some of the benefits that a vegan diet has on cancer prevention and longevity.
- Calcium intake in the majority of vegans was below recommendations (750 mg/d).
- Most of the human population is lactose intolerant.
- Only organic calcium is truly bioavailable to the cells in our body.
- Osteoporosis is not a calcium deficiency disease.
- Magnesium deficiency and to an extent vitamin D deficiency are the sources of the emergence of osteoporosis in dairy-dominated diets of the west.
- Magnesium is needed for more than 300 enzymes in the human body and one of those enzymes is the enzyme that regulates calcium metabolism.
- Magnesium is one of the most common and prevailing deficiencies in non-vegan diets because magnesium is mostly found in plant foods.
- Too much calcium leads to too little magnesium because, on the mineral wheel, magnesium and calcium are opposite minerals.
- Our bodies make K2 from vitamin K1 which is found in plants.
- B12 is not available for absorption since it is generated below the ileum, which is where B12 is absorbed.
- An evolutionary incongruent environment with clean water, rather than an incongruent diet, is to blame for the B12 deficiency in vegans.
- B12 is a crucial vitamin for the body’s numerous processes, particularly for the development of red blood cells and the health of the nervous system and the brain.
- B12, folate, and B6 are the three vitamins that regulate homocysteine levels.
- When our bodies make creatine, homocysteine is also created as a by-product.
- If we take creatine as a supplement we will downregulate the need of our body to make it internally and as a consequence will have lower levels of homocysteine.
- DHA is one more substance that is important for preventing cognitive decline.
- Eat a tablespoon of freshly ground flax seeds a day.
- Take an algae-based DHA supplement if you have money.
- Alpha-linolenic acid (ALA) is the most sensitive oil for the oxidation of all oils in existence.
- Even with a whole-food plant-based diet, vitamin E is extremely difficult to obtain in adequate amounts.
- As vitamin E is a fat-soluble antioxidant and it can only be found in fat.
- The number one source of vitamin E in the Western diet is exactly vegetable oil.
- Even if you use a home oil extraction to obtain fresh oil, as soon as the oil is extracted, the vitamin E content is drastically reduced.
- Heat speeds up oxidation.
- Synthesized vitamin E has no antioxidant activity in vivo.
- There has been a string of research that showed an increase in mortality with the use of synthetic vitamin E.
FAQ
References:
Passages selected from a book: Pokimica, Milos. Go Vegan? Review of Science Part 3. Kindle ed., Amazon, 2020.
- Sinha, R., Cross, A. J., Graubard, B. I., Leitzmann, M. F., & Schatzkin, A. (2009). Meat intake and mortality: a prospective study of over half a million people. Archives of internal medicine, 169(6), 562–571. https://doi.org/10.1001/archinternmed.2009.6
- Dietary Guidelines for Americans | health.gov. (n.d.). https://health.gov/our-work/nutrition-physical-activity/dietary-guidelines
- Thomas D. (2007). The mineral depletion of foods available to us as a nation (1940-2002)–a review of the 6th Edition of McCance and Widdowson. Nutrition and health, 19(1-2), 21–55. https://doi.org/10.1177/026010600701900205
- Bailey, R. L., West, K. P., Jr, & Black, R. E. (2015). The epidemiology of global micronutrient deficiencies. Annals of nutrition & metabolism, 66 Suppl 2, 22–33. https://doi.org/10.1159/000371618
- Berner, L. A., Keast, D. R., Bailey, R. L., & Dwyer, J. T. (2014). Fortified foods are major contributors to nutrient intakes in diets of US children and adolescents. Journal of the Academy of Nutrition and Dietetics, 114(7), 1009–1022.e8. https://doi.org/10.1016/j.jand.2013.10.012
- Rosanoff, A., Dai, Q., & Shapses, S. A. (2016). Essential Nutrient Interactions: Does Low or Suboptimal Magnesium Status Interact with Vitamin D and/or Calcium Status?. Advances in nutrition (Bethesda, Md.), 7(1), 25–43. https://doi.org/10.3945/an.115.008631
- Dietrich, M., Jacques, P., Pencina, M., Lanier, K., Keyes, M., Kaur, G., Wolf, P., & Vasan, R. (2009). Vitamin E Supplement Use and the Incidence of Cardiovascular Disease and All-Cause Mortality in the Framingham Heart Study: Does the Underlying Health Status Play a Role? Atherosclerosis, 205(2), 549. https://doi.org/10.1016/j.atherosclerosis.2008.12.019
- Institute of Medicine (US) Panel on Dietary Antioxidants and Related Compounds. (2000). Dietary Reference Intakes for Vitamin C, Vitamin E, Selenium, and Carotenoids. National Academies Press (US). [PubMed]
- Jiang, Qing. “Natural forms of vitamin E: metabolism, antioxidant, and anti-inflammatory activities and their role in disease prevention and therapy.” Free radical biology & medicine vol. 72 (2014): 76-90. doi:10.1016/j.freeradbiomed.2014.03.035
- World Health Organization. (2007). Protein and amino acid requirements in human nutrition : report of a joint FAO/WHO/UNU expert consultation. https://apps.who.int/iris/handle/10665/43411
- Fulgoni, V. L. (2008). Current protein intake in America: Analysis of the National Health and Nutrition Examination Survey, 2003–2004. The American Journal of Clinical Nutrition, 87(5), 1554S-1557S. https://doi.org/10.1093/ajcn/87.5.1554S
- Delimaris I. (2013). Adverse Effects Associated with Protein Intake above the Recommended Dietary Allowance for Adults. ISRN nutrition, 2013, 126929. https://doi.org/10.5402/2013/126929
- Fallon, N., & Dillon, S. A. (2020). Low Intakes of Iodine and Selenium Amongst Vegan and Vegetarian Women Highlight a Potential Nutritional Vulnerability. Frontiers in Nutrition, 7. https://doi.org/10.3389/fnut.2020.00072
- Yeliosof, O., & Silverman, L. A. (2018). Veganism as a cause of iodine deficient hypothyroidism. Journal of pediatric endocrinology & metabolism : JPEM, 31(1), 91–94. https://doi.org/10.1515/jpem-2017-0082
- Pawlak, R., Berger, J., & Hines, I. (2016). Iron Status of Vegetarian Adults: A Review of Literature. American journal of lifestyle medicine, 12(6), 486–498. https://doi.org/10.1177/1559827616682933
- Appleby, P., Roddam, A., Allen, N., & Key, T. (2007). Comparative fracture risk in vegetarians and nonvegetarians in EPIC-Oxford. European journal of clinical nutrition, 61(12), 1400–1406. https://doi.org/10.1038/sj.ejcn.1602659
- Plourde, M., & Cunnane, S. C. (2007). Extremely limited synthesis of long chain polyunsaturates in adults: implications for their dietary essentiality and use as supplements. Applied physiology, nutrition, and metabolism = Physiologie appliquee, nutrition et metabolisme, 32(4), 619–634. https://doi.org/10.1139/H07-034
- Gerster H. (1998). Can adults adequately convert alpha-linolenic acid (18:3n-3) to eicosapentaenoic acid (20:5n-3) and docosahexaenoic acid (22:6n-3)?. International journal for vitamin and nutrition research. Internationale Zeitschrift fur Vitamin- und Ernahrungsforschung. Journal international de vitaminologie et de nutrition, 68(3), 159–173. [PubMed]
- Brenna J. T. (2002). Efficiency of conversion of alpha-linolenic acid to long chain n-3 fatty acids in man. Current opinion in clinical nutrition and metabolic care, 5(2), 127–132. https://doi.org/10.1097/00075197-200203000-00002
- Yang, C., Xia, H., Wan, M., Lu, Y., Xu, D., Yang, X., Yang, L., & Sun, G. (2021). Comparisons of the effects of different flaxseed products consumption on lipid profiles, inflammatory cytokines and anthropometric indices in patients with dyslipidemia related diseases: systematic review and a dose-response meta-analysis of randomized controlled trials. Nutrition & metabolism, 18(1), 91. https://doi.org/10.1186/s12986-021-00619-3
- Shen, Y., Huang, X., Wu, J., Lin, X., Zhou, X., Zhu, Z., Pan, X., Xu, J., Qiao, J., Zhang, T., Ye, L., Jiang, H., Ren, Y., & Shan, P. (2022). The Global Burden of Osteoporosis, Low Bone Mass, and Its Related Fracture in 204 Countries and Territories, 1990-2019. Frontiers in Endocrinology, 13. https://doi.org/10.3389/fendo.2022.882241
- Mattson, M. P., Longo, V. D., & Harvie, M. (2017). Impact of intermittent fasting on health and disease processes. Ageing research reviews, 39, 46–58. https://doi.org/10.1016/j.arr.2016.10.005
- Bachmeyer, C., Bourguiba, R., Gkalea, V., & Papageorgiou, L. (2019). Vegan Diet as a Neglected Cause of Severe Megaloblastic Anemia and Psychosis. The American journal of medicine, 132(12), e850–e851. https://doi.org/10.1016/j.amjmed.2019.06.025
- Gilsing, A. M., Crowe, F. L., Lloyd-Wright, Z., Sanders, T. A., Appleby, P. N., Allen, N. E., & Key, T. J. (2010). Serum concentrations of vitamin B12 and folate in British male omnivores, vegetarians and vegans: results from a cross-sectional analysis of the EPIC-Oxford cohort study. European journal of clinical nutrition, 64(9), 933–939. https://doi.org/10.1038/ejcn.2010.142
- Smith, A. D., Smith, S. M., de Jager, C. A., Whitbread, P., Johnston, C., Agacinski, G., Oulhaj, A., Bradley, K. M., Jacoby, R., & Refsum, H. (2010). Homocysteine-lowering by B vitamins slows the rate of accelerated brain atrophy in mild cognitive impairment: a randomized controlled trial. PloS one, 5(9), e12244. https://doi.org/10.1371/journal.pone.0012244
- Douaud, G., Refsum, H., de Jager, C. A., Jacoby, R., Nichols, T. E., Smith, S. M., & Smith, A. D. (2013). Preventing Alzheimer’s disease-related gray matter atrophy by B-vitamin treatment. Proceedings of the National Academy of Sciences of the United States of America, 110(23), 9523–9528. https://doi.org/10.1073/pnas.1301816110
- Obersby, D., Chappell, D. C., Dunnett, A., & Tsiami, A. A. (2013). Plasma total homocysteine status of vegetarians compared with omnivores: a systematic review and meta-analysis. The British journal of nutrition, 109(5), 785–794. https://doi.org/10.1017/S000711451200520X
- Van Bavel, D., de Moraes, R., & Tibirica, E. (2019). Effects of dietary supplementation with creatine on homocysteinemia and systemic microvascular endothelial function in individuals adhering to vegan diets. Fundamental & clinical pharmacology, 33(4), 428–440. https://doi.org/10.1111/fcp.12442
- Liscum, L. (2008). Cholesterol biosynthesis. In Elsevier eBooks (pp. 399–421). https://doi.org/10.1016/b978-044453219-0.50016-7
- Emerit, J., Beaumont, C., & Trivin, F. (2001). Iron metabolism, free radicals, and oxidative injury. Biomedicine & pharmacotherapy = Biomedecine & pharmacotherapie, 55(6), 333–339. https://doi.org/10.1016/s0753-3322(01)00068-3
- Yu, Y., Yan, Y., Niu, F., Wang, Y., Chen, X., Su, G., Liu, Y., Zhao, X., Qian, L., Liu, P., & Xiong, Y. (2021). Ferroptosis: a cell death connecting oxidative stress, inflammation and cardiovascular diseases. Cell Death Discovery, 7(1). https://doi.org/10.1038/s41420-021-00579-w
- Teucher, B., Olivares, M., & Cori, H. (2004). Enhancers of iron absorption: ascorbic acid and other organic acids. International journal for vitamin and nutrition research. Internationale Zeitschrift fur Vitamin- und Ernahrungsforschung. Journal international de vitaminologie et de nutrition, 74(6), 403–419. https://doi.org/10.1024/0300-9831.74.6.403
- Bakaloudi, D. R., Halloran, A., Rippin, H. L., Oikonomidou, A. C., Dardavesis, T. I., Williams, J., Wickramasinghe, K., Breda, J., & Chourdakis, M. (2021). Intake and adequacy of the vegan diet. A systematic review of the evidence. Clinical nutrition (Edinburgh, Scotland), 40(5), 3503–3521. https://doi.org/10.1016/j.clnu.2020.11.035
- Kondaiah, P., Yaduvanshi, P. S., Sharp, P. A., & Pullakhandam, R. (2019). Iron and Zinc Homeostasis and Interactions: Does Enteric Zinc Excretion Cross-Talk with Intestinal Iron Absorption?. Nutrients, 11(8), 1885. https://doi.org/10.3390/nu11081885
- Foster, M., Chu, A., Petocz, P., & Samman, S. (2013). Effect of vegetarian diets on zinc status: a systematic review and meta-analysis of studies in humans. Journal of the science of food and agriculture, 93(10), 2362–2371. https://doi.org/10.1002/jsfa.6179
- Saunders, A. V., Craig, W. J., & Baines, S. K. (2013). Zinc and vegetarian diets. The Medical journal of Australia, 199(S4), S17–S21. https://doi.org/10.5694/mja11.11493
- McLaren, D. S. (1974). THE GREAT PROTEIN FIASCO. The Lancet, 304(7872), 93–96. https://doi.org/10.1016/s0140-6736(74)91649-3
- Semba, R. D. (2016). The rise and fall of protein malnutrition in global health. Annals of nutrition & metabolism, 69(2), 79. https://doi.org/10.1159/000449175
- Kubo, H., Sawada, S., Satoh, M., Asai, Y., Kodama, S., Sato, T., Tomiyama, S., Seike, J., Takahashi, K., Kaneko, K., Imai, J., & Katagiri, H. (2022). Insulin-like growth factor-1 levels are associated with high comorbidity of metabolic disorders in obese subjects; a Japanese single-center, retrospective-study. Scientific Reports, 12(1), 1-9. https://doi.org/10.1038/s41598-022-23521-1
- Peng, A. W., Dardari, Z., Blumenthal, R. S., Dzaye, O., Obisesan, O. H., Uddin, S., Nasir, K., Blankstein, R., Budoff, M. J., Mortensen, M. B., Joshi, P. H., Page, J. T., & Blaha, M. J. (2021). Very High Coronary Artery Calcium (≥1000) and Association With Cardiovascular Disease Events, Non–Cardiovascular Disease Outcomes, and Mortality. Circulation, 143(16), 1571–1583. https://doi.org/10.1161/circulationaha.120.050545
- Lafuente, M., Rodríguez González-Herrero, M. E., Romeo Villadóniga, S., & Domingo, J. C. (2021). Antioxidant Activity and Neuroprotective Role of Docosahexaenoic Acid (DHA) Supplementation in Eye Diseases That Can Lead to Blindness: A Narrative Review. Antioxidants (Basel, Switzerland), 10(3), 386. https://doi.org/10.3390/antiox10030386
- Holub B. J. (2009). Docosahexaenoic acid (DHA) and cardiovascular disease risk factors. Prostaglandins, leukotrienes, and essential fatty acids, 81(2-3), 199–204. https://doi.org/10.1016/j.plefa.2009.05.016
- Gerster H. (1998). Can adults adequately convert alpha-linolenic acid (18:3n-3) to eicosapentaenoic acid (20:5n-3) and docosahexaenoic acid (22:6n-3)?. International journal for vitamin and nutrition research. Internationale Zeitschrift fur Vitamin- und Ernahrungsforschung. Journal international de vitaminologie et de nutrition, 68(3), 159–173. [PubMed]
- Pearson, P., Lewis, S. A., Britton, J., Young, I. S., & Fogarty, A. (2006). The pro-oxidant activity of high-dose vitamin E supplements in vivo. BioDrugs : clinical immunotherapeutics, biopharmaceuticals and gene therapy, 20(5), 271–273. https://doi.org/10.2165/00063030-200620050-00002
Related Posts
Do you have any questions about nutrition and health?
I would love to hear from you and answer them in my next post. I appreciate your input and opinion and I look forward to hearing from you soon. I also invite you to follow us on Facebook, Instagram, and Pinterest for more diet, nutrition, and health content. You can leave a comment there and connect with other health enthusiasts, share your tips and experiences, and get support and encouragement from our team and community.
I hope that this post was informative and enjoyable for you and that you are prepared to apply the insights you learned. If you found this post helpful, please share it with your friends and family who might also benefit from it. You never know who might need some guidance and support on their health journey.
– You Might Also Like –

Learn About Nutrition
Milos Pokimica is a doctor of natural medicine, clinical nutritionist, medical health and nutrition writer, and nutritional science advisor. Author of the book series Go Vegan? Review of Science, he also operates the natural health website GoVeganWay.com
Medical Disclaimer
GoVeganWay.com brings you reviews of the latest nutrition and health-related research. The information provided represents the personal opinion of the author and is not intended nor implied to be a substitute for professional medical advice, diagnosis, or treatment. The information provided is for informational purposes only and is not intended to serve as a substitute for the consultation, diagnosis, and/or medical treatment of a qualified physician or healthcare provider.NEVER DISREGARD PROFESSIONAL MEDICAL ADVICE OR DELAY SEEKING MEDICAL TREATMENT BECAUSE OF SOMETHING YOU HAVE READ ON OR ACCESSED THROUGH GoVeganWay.com
NEVER APPLY ANY LIFESTYLE CHANGES OR ANY CHANGES AT ALL AS A CONSEQUENCE OF SOMETHING YOU HAVE READ IN GoVeganWay.com BEFORE CONSULTING LICENCED MEDICAL PRACTITIONER.
In the event of a medical emergency, call a doctor or 911 immediately. GoVeganWay.com does not recommend or endorse any specific groups, organizations, tests, physicians, products, procedures, opinions, or other information that may be mentioned inside.
Editor Picks –
Milos Pokimica is a health and nutrition writer and nutritional science advisor. Author of the book series Go Vegan? Review of Science, he also operates the natural health website GoVeganWay.com
Latest Articles –
Top Health News — ScienceDaily
- The overlooked nutrition risk of Ozempic and Wegovyon February 4, 2026
Popular weight-loss drugs like Ozempic and Wegovy can dramatically curb appetite, but experts warn many users are flying blind when it comes to nutrition. New research suggests people taking these medications may not be getting enough guidance on protein, vitamins, and overall diet quality, increasing the risk of muscle loss and nutrient deficiencies.
- A 25-year study found an unexpected link between cheese and dementiaon February 4, 2026
A massive Swedish study tracking nearly 28,000 people for 25 years found an unexpected link between full-fat dairy and brain health. Among adults without a genetic risk for Alzheimer’s, eating more full-fat cheese was associated with a noticeably lower risk of developing the disease, while higher cream intake was tied to reduced dementia risk overall. The findings challenge decades of low-fat dietary advice but come with important caveats.
- MIT’s new brain tool could finally explain consciousnesson February 4, 2026
Scientists still don’t know how the brain turns physical activity into thoughts, feelings, and awareness—but a powerful new tool may help crack the mystery. Researchers at MIT are exploring transcranial focused ultrasound, a noninvasive technology that can precisely stimulate deep regions of the brain that were previously off-limits. In a new “roadmap” paper, they explain how this method could finally let scientists test cause-and-effect in consciousness research, not just observe […]
- Why heart disease risk in type 2 diabetes looks different for men and womenon February 4, 2026
Scientists are digging into why heart disease risk in type 2 diabetes differs between men and women—and sex hormones may be part of the story. In a large Johns Hopkins study, men with higher testosterone had lower heart disease risk, while rising estradiol levels were linked to higher risk. These hormone effects were not seen in women. The results point toward more personalized approaches to heart disease prevention in diabetes.
- Sound machines might be making your sleep worseon February 4, 2026
Sound machines may not be the sleep saviors many believe. Researchers found that pink noise significantly reduced REM sleep, while simple earplugs did a better job protecting deep, restorative sleep from traffic noise. When pink noise was combined with outside noise, sleep quality dropped even further. The results suggest that popular “sleep sounds” could be doing more harm than good—particularly for kids.
- This unexpected plant discovery could change how drugs are madeon February 3, 2026
Plants make chemical weapons to protect themselves, and many of these compounds have become vital to human medicine. Researchers found that one powerful plant chemical is produced using a gene that looks surprisingly bacterial. This suggests plants reuse microbial tools to invent new chemistry. The insight could help scientists discover new drugs and produce them more sustainably.
- A hidden cellular process may drive aging and diseaseon February 3, 2026
As we age, our cells don’t just wear down—they reorganize. Researchers found that cells actively remodel a key structure called the endoplasmic reticulum, reducing protein-producing regions while preserving fat-related ones. This process, driven by ER-phagy, is tied to lifespan and healthy aging. Because these changes happen early, they could help trigger later disease—or offer a chance to stop it.
PubMed, #vegan-diet –
- Diet type and the oral microbiomeon February 2, 2026
CONCLUSION: The diet-oral microbiome-systemic inflammation axis is bidirectional and clinically relevant. Understanding both direct ecological regulation and indirect metabolic effects is essential to support precision nutrition strategies aimed at maintaining oral microbial balance and systemic inflammatory risk mitigation.
- Consensus document on healthy lifestyleson January 22, 2026
Proteins are a group of macronutrients that are vital to our lives, as they perform various functions, including structural, defensive and catalytic. An intake of 1.0-1.2 g/kg/body weight per day would be sufficient to meet our needs. Carbohydrate requirements constitute 50 % of the total caloric value and should be obtained mainly in the form of complex carbohydrates. In addition, a daily intake of both soluble and insoluble fiber is necessary. Regular consumption of extra virgin olive oil […]
- Vitamin B12 and D status in long-term vegetarians: Impact of diet duration and subtypes in Beijing, Chinaon January 21, 2026
CONCLUSIONS: This study reveals a dual challenge among Beijing long-term vegetarians: vitamin B12 deficiency was strongly associated with the degree of exclusion of animal products from the diet (veganism), while vitamin D deficiency was highly prevalent and worsened with longer diet duration. The near-universal vitamin D deficiency observed in this study suggests that, in the Beijing context, the risk may extend beyond dietary choice, potentially reflecting regional environmental factors;…
- Nutritional evaluation of duty meals provided to riot police forces in Germanyon January 13, 2026
Background: The primary role of the German riot police is maintaining internal security. Due to challenging working conditions, riot police forces face an elevated risk of various diseases. During duty, forces are provided with meals. A balanced diet can reduce the risk of some of these diseases and contribute to health-promoting working conditions. Aim: First evaluation of the nutritional quality of duty meals in Germany based on German Nutrition Society recommendations (DGE). Methods: In…
- Iodineon January 1, 2006
Iodine is an essential trace nutrient for all infants that is a normal component of breastmilk. Infant requirements are estimated to be 15 mcg/kg daily in full-term infants and 30 mcg/kg daily in preterm infants.[1] Breastmilk iodine concentration correlates well with maternal urinary iodine concentration and may be a useful index of iodine sufficiency in infants under 2 years of age, but there is no clear agreement on a value that indicates iodine sufficiency, and may not correlate with […]
Random Posts –
Featured Posts –
Latest from PubMed, #plant-based diet –
- From paddy soil to dining table: biological biofortification of rice with zincby Lei Huang on February 4, 2026
One-third of paddy soils are globally deficient in zinc (Zn) and 40% of Zn loss in the procession from brown rice to polished rice, which results in the global issue of hidden hunger, e.g., the micronutrient deficiencies in the rice-based population of developing countries. In the recent decades, biofortification of cereal food crops with Zn has emerged as a promising solution. Herein, we comprehensively reviewed the entire process of Zn in paddy soil to human diet, including the regulatory…
- Molecular Characterization of Tobacco Necrosis Virus A Variants Identified in Sugarbeet Rootsby Alyssa Flobinus on February 3, 2026
Sugarbeet provides an important source of sucrose; a stable, environmentally safe, and low-cost staple in the human diet. Viral diseases arising in sugarbeet ultimately impact sugar content, which translates to financial losses for growers. To manage diseases and prevent such losses from occurring, it is essential to characterize viruses responsible for disease. Recently, our laboratory identified a tobacco necrosis virus A variant named Beta vulgaris alphanecrovirus 1 (BvANV-1) in sugarbeet…
- Nutrition in early life interacts with genetic risk to influence preadult behaviour in the Raine Studyby Lars Meinertz Byg on February 3, 2026
CONCLUSIONS: Nutrition in early life and psychiatric genetic risk may interact to determine lasting child behaviour. Contrary to our hypothesis, we find dietary benefits in individuals with lower ADHD PGS, necessitating replication. We also highlight the possibility of including genetics in early nutrition intervention trials for causal inference.
- Effect of the gut microbiota on insect reproduction: mechanisms and biotechnological prospectsby Dilawar Abbas on February 2, 2026
The insect gut microbiota functions as a multifunctional symbiotic system that plays a central role in host reproduction. Through the production of bioactive metabolites, gut microbes interact with host hormonal pathways, immune signaling, and molecular regulatory networks, thereby shaping reproductive physiology and fitness. This review summarizes recent advances in understanding how gut microbiota regulate insect reproduction. Accumulating evidence demonstrates that microbial metabolites…
- Rationale and design of a parallel randomised trial of a plant-based intensive lifestyle intervention for diabetes remission: The REmission of diabetes using a PlAnt-based weight loss InteRvention…by Brighid McKay on February 2, 2026
CONCLUSIONS: This trial will provide high-quality clinical evidence on the use of plant-based ILIs to address the epidemics of obesity and diabetes to inform public health policies and programs in Canada and beyond.
- Diet type and the oral microbiomeby Daniel Betancur on February 2, 2026
CONCLUSION: The diet-oral microbiome-systemic inflammation axis is bidirectional and clinically relevant. Understanding both direct ecological regulation and indirect metabolic effects is essential to support precision nutrition strategies aimed at maintaining oral microbial balance and systemic inflammatory risk mitigation.