How to Stop Tooth Decay: Symptoms, Causes & Prevention
Sugar consumption is the main cause of cavities and tooth decay, combined with mineral deficiencies especially magnesium, zinc, copper and trace elements.
Milos Pokimica
Written By: Milos Pokimica
Medically Reviewed by: Dr. Xiùying Wáng, M.D.
Updated October 4, 2023Key Takeaways:
– Tooth decay and gum diseases affect 60–90% of people worldwide.
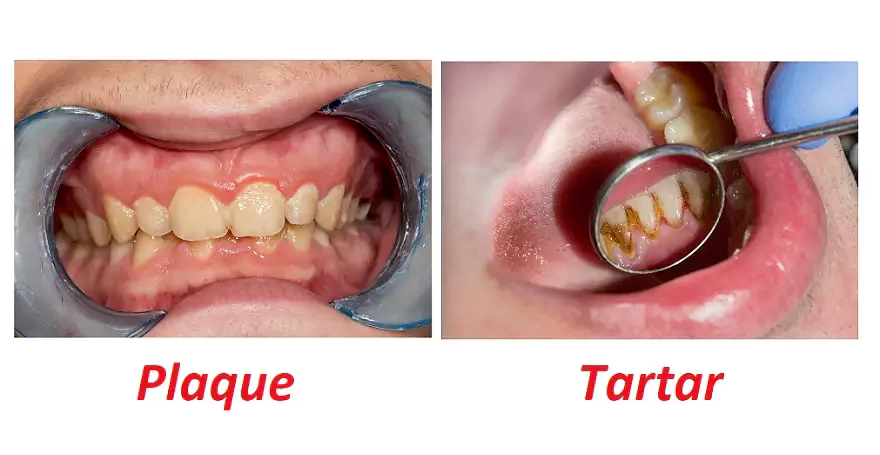
– The bacteria form a sticky layer on the teeth called dental plaque or biofilm, where they feed on the sugars and starches from food and produce acids that erode tooth enamel.
– The human oral microbiome consists of more than 700 different bacterial species, making it one of the most complex microbial flora in the human body (Jørn et al., 2005).
– One of the main factors that contribute to tooth decay is the consumption of dietary carbohydrates, especially sucrose (Sheiham & James, 2015).
– Some bacteria are beneficial for oral health because they help balance the pH and prevent the growth of harmful microbes.
– A bacterium that is particularly notorious for causing caries is Streptococcus mutans.
– Streptococcus mutans have a special ability to adhere to the tooth surface and produce large amounts of acid when it consumes sugars, especially sucrose but also fructose as well (Forssten et al., 2010).
– Streptococcus mutans can also form biofilms, which are complex structures of bacteria and extracellular substances that protect them from external threats (Forssten et al., 2010).
– Candida albicans can also form biofilms on the teeth, and it havs a symbiotic relationship with Streptococcus mutans (Metwalli et al., 2013).
– The yeast and the bacteria stick to each other and to the tooth surface, forming a protective layer that shields them from saliva, brushing, and antimicrobial agents.
– The streptococci produce lactic acid from sugar, which lowers the pH and erodes the enamel. The acid also helps the yeast to grow, and the yeast provides oxygen-free zones for the bacteria to thrive.
– Several studies have shown that Candida albicans enhances the adherence of Streptococcus mutans to different surfaces, such as human teeth and artificial materials (Metwalli et al., 2013).
– Candida albicans can also produce acid and cause caries by itself, as shown by an experiment where rats raised on an ampicillin-supplemented diet and exposed to Candida albicans developed severe cavities (Klinke et al., 2011).
– The truth is that tooth decay has only one cause: dietary sugars (Sheiham & James, 2015).
– There is no safe level of sugar intake for your teeth. The only way to prevent tooth decay is to avoid or minimize sugar intake as much as possible.
– The World Health Organization (WHO) recommends limiting your free sugars intake to less than 5% of your total energy intake per day.
– Sucrose, which is the common table sugar, has a special property that makes it the most cariogenic, or cavity-causing, carbohydrate in our diet. Sucrose can be transformed into extracellular polysaccharides (EPS) by some plaque bacteria, such as Streptococcus mutans (Forssten et al., 2010).
– Among different carbohydrates, sucrose is the most effective in stimulating EPS production.
– Mineral deficiencies can affect the formation and structure of the enamel, and therefore its physical properties (Zamojda et al., 2023).
– Enamel is mainly made of crystals called hydroxyapatites, which are composed of calcium and phosphate. But enamel also contains trace amounts of other minerals, such as magnesium, zinc, and copper (Zamojda et al., 2023).
– Magnesium, zinc, and copper may have complex interactions with each other and with other factors that affect enamel structure and function.
– Trace minerals are present in the enamel and can affect its formation and structure.
– A study by (Ghadimi et al., 2013) with 38 human teeth measured the concentration of 19 trace elements in the enamel samples.
– Deficiency in trace minerals may have implications for enamel’s health and function. For example, some trace elements may influence enamel’s crystallographic properties and ultimately its physical properties.
– The most important factor in stopping tooth decay is the diet. Do not consume more than 3 to 5 percent of calories from free sugar and correct mineral deficiencies.
– There are very potent natural nontoxic phytochemicals, antioxidants, and other substances that are good in fighting both candida and bacteria and can be used in homemade natural mouthwash. At the same time, they also provide a high amount of antioxidant and anti-inflammatory support for inflamed gums.
Tooth Decay.
Tooth decay is a serious problem that affects people of all ages and backgrounds, but especially children and those who have limited access to dental care. In the United States, almost half of the children between 2 to 11 years old have had tooth decay in their baby teeth, and in the adult population, tooth decay and gum diseases affect 60–90% of people worldwide. People with disabilities and lower socioeconomic status are more likely to suffer from tooth decay and its complications.
But what causes tooth decay and how can we prevent it?
Tooth decay is the result of a complex interaction between the bacteria that live in the mouth, the food we eat, the saliva we produce, and our genetic factors.
The bacteria form a sticky layer on the teeth called dental plaque or biofilm, where they feed on the sugars and starches from food and produce acids that erode tooth enamel.
The acids also create sticky substances called glucans that help the bacteria stick to the teeth and form more plaque.
Some areas of your teeth are more prone to decay than others, such as the pits and fissures on the chewing surfaces of your back teeth. These areas are harder to clean and more likely to trap food and plaque, which can lead to more acid production and enamel breakdown. That’s why most of the cavities occur in these areas.
Tooth decay is a preventable disease. It can be avoided with proper oral hygiene, regular dental check-ups, and a balanced diet.
Microorganisms Present in the Mouth.
Have you ever wondered what kind of microscopic creatures live in the mouth? You might be surprised to learn that the human mouth is home to a diverse and complex community of bacteria, fungi, viruses, and other microorganisms. These tiny organisms form natural biofilms on the surfaces of your teeth, gums, tongue, and cheeks, taking advantage of the abundant nutrients and moisture in your oral cavity.
The human oral microbiome consists of more than 700 different bacterial species, making it one of the most complex microbial flora in the human body (Jørn et al., 2005).
However, not all oral bacteria are friendly. Sometimes, a disturbance in the balance of this ecosystem can lead to the overgrowth of harmful bacteria that cause oral diseases such as tooth decay and gum disease.
In the supragingival plaque (the sticky film that forms on the surface of your teeth above the gum line), Streptococcus mutans is the main culprit for causing cavities, along with other streptococci such as S. sanguinis, S. mitis, and S. salivarius (Forssten et al., 2010). These bacteria produce acids that erode the enamel of your teeth and create holes or cavities. Other bacteria that contribute to tooth decay include lactobacilli and Veillonella.
In the subgingival plaque (the plaque that accumulates below the gum line), you will find mostly Gram-negative anaerobic bacteria such as Fusobacterium nucleatum, Porphyromonas gingivalis, and Prevotella intermedia (Jørn et al., 2005). These bacteria are known to cause periodontal disease (gum disease), which is a chronic inflammation and infection of the gums and surrounding tissues. These bacteria release toxins that damage the gum tissue and bone that support your teeth, leading to bleeding, swelling, pain, and eventually tooth loss.
Dental Plaque.
Teeth are covered by a thin layer of sticky substance called pellicle, which acts as a landing pad for various microorganisms. These microorganisms attach themselves to the pellicle and to each other, forming a complex network of cells and fibers. This network is called a biofilm, and it is also known as dental plaque.
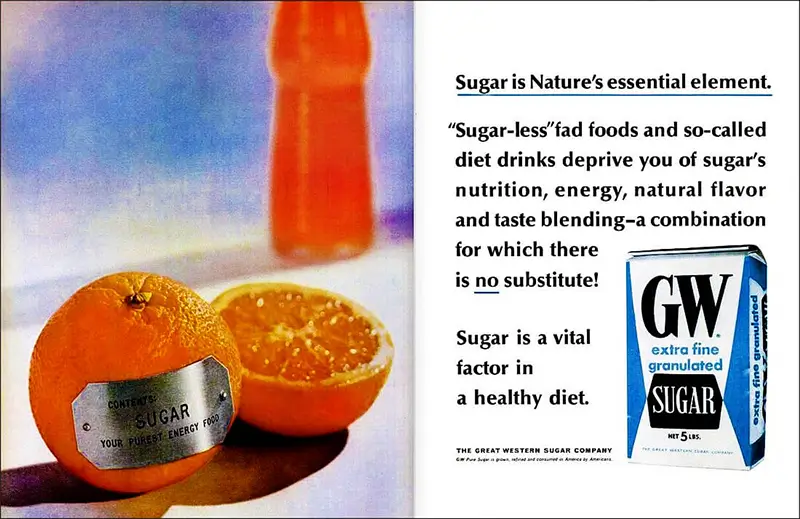
Dental plaque is not just a cosmetic problem. It can also cause serious damage to your teeth and gums by producing harmful substances that affect the health of your dental tissues: enamel, dentin, and cementum. These are the hard layers that protect the inner part of your tooth, the pulp, where the nerves and blood vessels are located.
The bacteria in the plaque use the sugars and starches from food and drinks as their fuel, and in the process, they produce acids that lower the pH of the mouth (Metwalli et al., 2013).
These acids dissolve the minerals from dental tissues, creating tiny holes or cavities in the teeth. This condition is called dental caries, and it can lead to toothache, infection, and tooth loss.
But that’s not all. The bacteria in the plaque can also interact with each other in different ways. Some bacteria can create favorable conditions for other bacteria to grow and thrive, such as providing nutrients or enzymes. This is called synergy, and it can increase the diversity and virulence of the plaque. Some bacteria can also stick to each other on the surface of your teeth, forming clusters or aggregates. This is called coaggregation, and it can help the bacteria resist being washed away by saliva or brushing. These interactions can make the plaque more resistant to your body’s defenses and more likely to cause gum disease.
As you can see, teeth are not just inert structures. They are living ecosystems where different types of microorganisms coexist and compete for resources. Keeping these ecosystems in balance is essential for your oral health and overall well-being.
The Three Steps of Dental Plaque Formation.
Dental plaque formation involves three main steps:
- Step 1: The acquired pellicle. As soon as you clean your teeth, your saliva coats them with a thin layer of molecules. This layer is called the acquired pellicle, and it contains various components such as glycoproteins, mucins, sialic acid, and bacterial debris. The acquired pellicle protects your enamel from erosion and abrasion, but it also provides a surface for bacteria to attach to.
- Step 2: The primary colonizers. The next step is when some bacteria start to interact with the acquired pellicle and stick to it. These bacteria are called the primary colonizers, and they include species such as Streptococcus sanguis and Actinomyces viscosus. The primary colonizers form the initial layer of the biofilm, and their growth is influenced by factors such as osmolarity, carbon source, and pH.
- Step 3: The secondary colonizers. The final step is when other bacteria join the biofilm by adhering to the primary colonizers. These bacteria are called the secondary colonizers, and they include species such as S. mutans and S. sobrinus . The secondary colonizers add more diversity and complexity to the biofilm, and they also produce more acidic metabolites that can damage your teeth.
How Dental Plaque Causes Cavities.
One of the main factors that contributes to tooth decay is the consumption of dietary carbohydrates, especially sucrose (Sheiham & James, 2015).
Sucrose is a type of sugar that consists of 50% glucose and 50% fructose molecules. When you eat sucrose, some of it gets broken down by enzymes in your saliva, but some of it also reaches your dental plaque. There, some bacteria can use sucrose to make extracellular polysaccharides (EPS), which are long chains of sugar molecules. EPS can make the biofilm more sticky and more resistant to removal by brushing or rinsing. EPS can also trap more bacteria and food particles in the biofilm, creating a favorable environment for acid production.
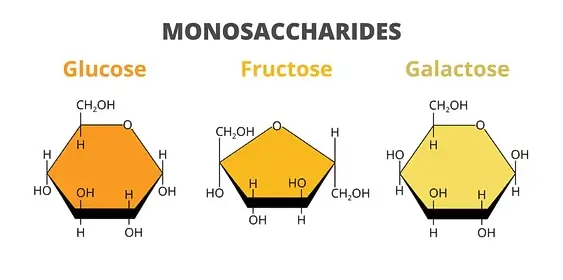
Acid production is another key factor that leads to tooth decay. Some bacteria in the dental plaque can ferment carbohydrates (such as glucose and fructose) into acids (such as lactic acid and acetic acid) (Jørn et al., 2005).
These acids lower the pH of the biofilm, making it more acidic. When the pH drops below a certain level (usually around 5.5), the enamel starts to dissolve. This process is called demineralization, and it creates tiny holes or cavities in your teeth.
How Does a Cavity Develop?
The tooth decay process is a gradual deterioration of the tooth’s hard outer layer, called enamel, by the action of bacteria and acids. It can lead to cavities, pain, infection, and tooth loss if not treated. Here is a summary of the stages of tooth decay:
- Stage 1: Initial demineralization. This is tooth decay early sign when the enamel begins to lose minerals due to the acids produced by plaque bacteria. A white spot may appear on the tooth, indicating early decay. This early stage can be reversed by using fluoride and minerals from saliva to repair the enamel.
- Stage 2: Enamel decay. This is when the enamel breaks down further and forms small holes or cavities. The tooth may become darker in color or have black spots. This stage requires a filling by a dentist to restore the tooth’s structure.
- Stage 3: Dentin decay. This is when the decay reaches the dentin, which is the softer layer under the enamel. The dentin contains tubes that connect to the nerves of the tooth, so this stage may cause sensitivity or pain. The decay also progresses faster in the dentin than in the enamel.
- Stage 4: Pulp damage. This is when the decay affects the pulp, which is the innermost layer of the tooth that contains blood vessels and nerves. The pulp may become inflamed and swollen, putting pressure on the nerves and causing more pain. The pulp may also become infected by bacteria.
- Stage 5: Abscess. This is when the infection spreads from the pulp to the surrounding tissues and forms a pus-filled pocket called an abscess. An abscess can cause severe pain, swelling, fever, and other symptoms. It can also damage the bone and other teeth if not treated promptly.
The Role of Streptococcus Mutans in Tooth Decay.
Not all bacteria in plaque are equally harmful. Some bacteria are actually beneficial for oral health because they help balance the pH and prevent the growth of harmful microbes. However, there is one bacterium that is particularly notorious for causing caries: Streptococcus mutans.
It belongs to a group of seven closely related species called the mutans streptococci. Streptococcus mutans can be found in your mouth, throat, and gut, but it prefers to live on your teeth.
This tiny microbe has a special ability to adhere to the tooth surface and produce large amounts of acid when it consumes sugars, especially sucrose but also fructose as well (Forssten et al., 2010).
These sugars are commonly found in candies, soft drinks, fruits, and other foods that we often enjoy. When Streptococcus mutans break down these sugars, it lowers the pH of the plaque and creates an acidic environment that dissolves the enamel.

This process is called demineralization, and it makes the tooth more vulnerable to decay.
Streptococcus mutans is not only good at making acid but also at surviving it. It can tolerate low pH levels better than most other bacteria in plaque. This gives it an advantage over its competitors and allows it to dominate the plaque community.
Streptococcus mutans can also form biofilms, which are complex structures of bacteria and extracellular substances that protect them from external threats (Forssten et al., 2010).
Biofilms make it harder for saliva, fluoride, and antimicrobial agents to reach and kill Streptococcus mutans. They also make it easier for Streptococcus mutans to transfer from one tooth to another, or from one person to another through saliva or utensils.
Streptococcus mutans has several features that make it cariogenic (cavity-causing), such as:
- Adherence to enamel surfaces. Streptococcus mutans can stick to the acquired pellicle and to other plaque bacteria using special proteins called adhesins. This allows Streptococcus mutans to form part of the biofilm and resist being washed away by saliva or water.
- Production of acidic metabolites. Streptococcus mutans can ferment various carbohydrates into acids, such as lactic acid. Streptococcus mutans can also tolerate low pH levels better than most other oral bacteria. This means that Streptococcus mutans can survive and thrive in an acidic environment, while other bacteria die or become less active.
- Capacity to build up glycogen reserves. Streptococcus mutans can store excess glucose as glycogen inside its cells. Glycogen is a type of polysaccharide that can be used as an energy source when carbohydrates are scarce. This gives Streptococcus mutans an advantage over other bacteria that depend on external carbohydrates for energy.
- Ability to synthesize extracellular polysaccharides. Streptococcus mutans can produce EPS from sucrose, but also from glucose and fructose. EPS can be either glucans (made of glucose units) or fructans (made of fructose units). Streptococcus mutans uses enzymes called glucosyltransferases (GTF) and fructosyltransferases (FTF) to make EPS. EPS can help Streptococcus mutans to adhere to the biofilm, protect itself from antimicrobial agents, and create a reservoir of carbohydrates for future use.
Usually, Streptococcus mutans appears in the tooth cavities about 6-24 months before the onset of caries. Streptococcus mutans can also cooperate with other bacteria, such as Streptococcus sobrinus and lactobacilli, to enhance the cariogenic potential of the biofilm.
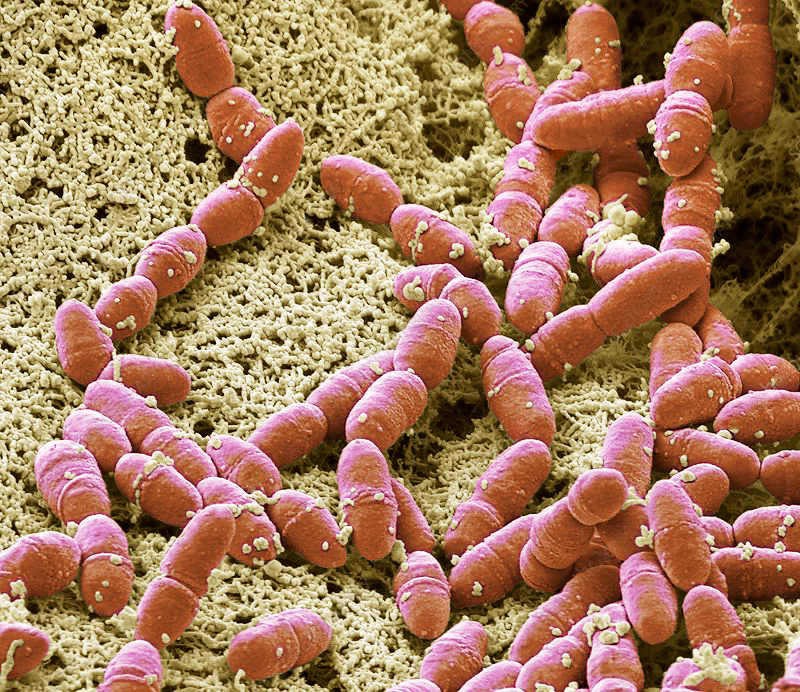
But Streptococcus mutans are not alone in their attack. They often team up with another microbe that you might have heard of, Candida albicans. This is a type of fungus that can cause infections in different parts of your body, including your mouth.
Candida albicans can also form biofilms on your teeth, and it seems that they have a symbiotic relationship with Streptococcus mutans (Metwalli et al., 2013).
Candida albicans can help Streptococcus mutans by providing them with more sugar to make glucans and acid. Streptococcus mutans can help Candida albicans by creating an acidic environment that favors their growth. Together, they can create a vicious cycle of tooth decay that can damage your teeth beyond repair.
Candida Albicans: Partner in Crime?
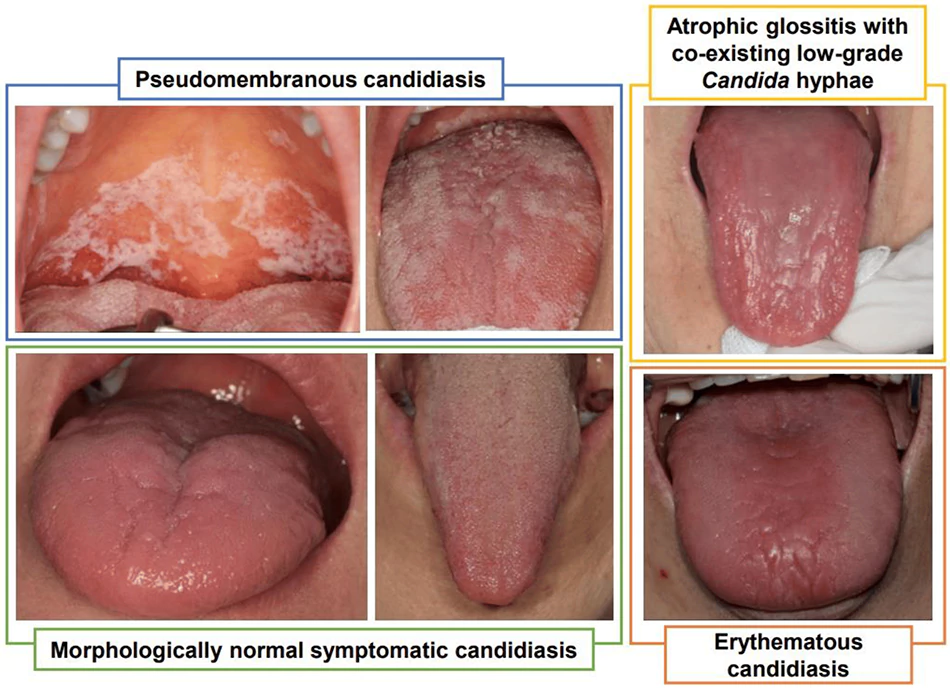
Candida albicans is a type of yeast that normally lives in our mouth, skin, and gut without causing any trouble. But when our immune system is weakened by diseases, or chronic inflammation this friendly fungus can become a dangerous enemy. It can change its shape from round cells to hyphae (long filaments) that it uses to invade our tissues and organs by stabbing and piercing the tissue. This is called candidiasis, and it can be fatal if not treated.
Hyphae do not fully kill the tissue that candida invades all at once and also candida tricks our immune system into not recognizing it. That is a reason why it is almost impossible to get rid of it completely.
But how does Candida albicans get a foothold in our mouths? It turns out that it has some help from other microbes that live there. These are the oral bacteria, such as streptococci, that form a sticky layer on our teeth and gums. Candida albicans can stick to this layer and grow along with the bacteria. This is called coadhesion, and it is essential for Candida albicans to colonize and persist in our oral cavity.
The oral bacteria also provide some other benefits for Candida albicans. They produce lactic acid, which Candida albicans can use as food. They also lower the oxygen level in the mouth, which Candida albicans prefer. And they secrete some substances that stimulate the growth of Candida. In return, Candida protects the bacteria from being washed away by saliva or swallowed by us.
One of the bacteria that Candida albicans likes to cooperate with is Streptococcus mutans, the main culprit of dental caries. It’s a win-win situation for them.
The streptococci produce lactic acid from sugar, which lowers the pH and erodes the enamel. The acid also helps the yeast grow, and the yeast provides oxygen-free zones for the bacteria to thrive. Moreover, the yeast and the bacteria stick to each other and to the tooth surface, forming a protective layer that shields them from saliva, brushing, and antimicrobial agents.
This sounds like a perfect match made in hell, right? But is there any evidence that Candida albicans and Streptococcus mutans actually cause more damage together than alone?
The answer is yes.
Several studies have shown that Candida albicans enhances the adherence of Streptococcus mutans to different surfaces, such as human teeth and artificial materials (Metwalli et al., 2013).
You can see this for yourself in the image below (Figure 1), where the bacteria are attached to the yeast filaments like beads on a string.
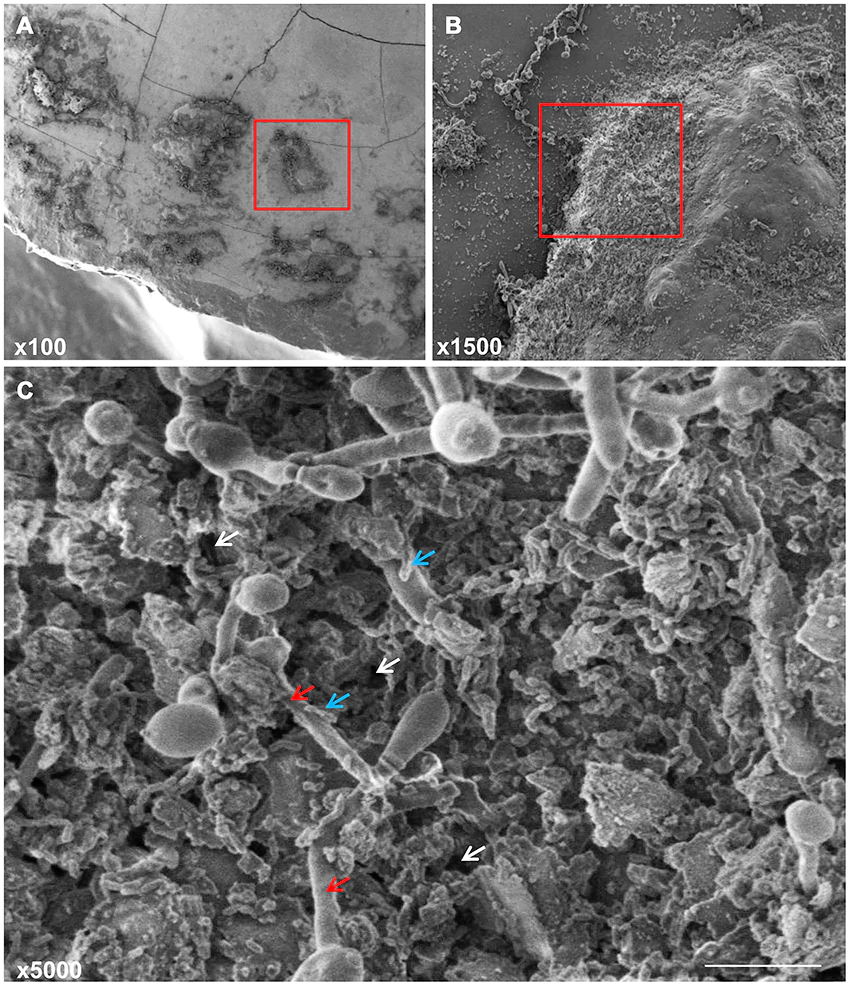
What’s more, Candida albicans can also produce acid and cause caries by itself, as shown by an experiment where rats raised on an ampicillin-supplemented diet and exposed to Candida albicans developed severe cavities as a consequence of Candida’s pronounced ability to produce and tolerate acids (Klinke et al., 2011). And if you believe that this only happens in animals, think again.
A clinical study found that children who had more Candida albicans in their mouths also had more caries (Raja et al., 2010).
So what does this mean for you and your oral health? It means that you should not ignore the presence of Candida albicans in your mouth, especially if you have other risk factors for caries, such as high sugar intake, poor oral hygiene, or dry mouth. It also means that you should be aware of the potential interactions between Candida albicans and Streptococcus mutans, and how they can make each other more harmful. The next time you brush your teeth, remember that you are not only fighting bacteria but also fungi.
Diet and Dental Caries.
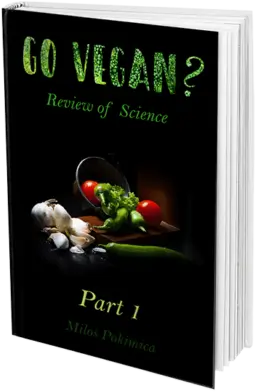
You may think that tooth decay is a multifactorial disease, meaning that it has many causes. You may also think that you can prevent it by using fluoride and brushing your teeth regularly. However, these are misconceptions that have been influenced by the sugar industry, which wants to downplay the role of sugar in causing tooth decay.
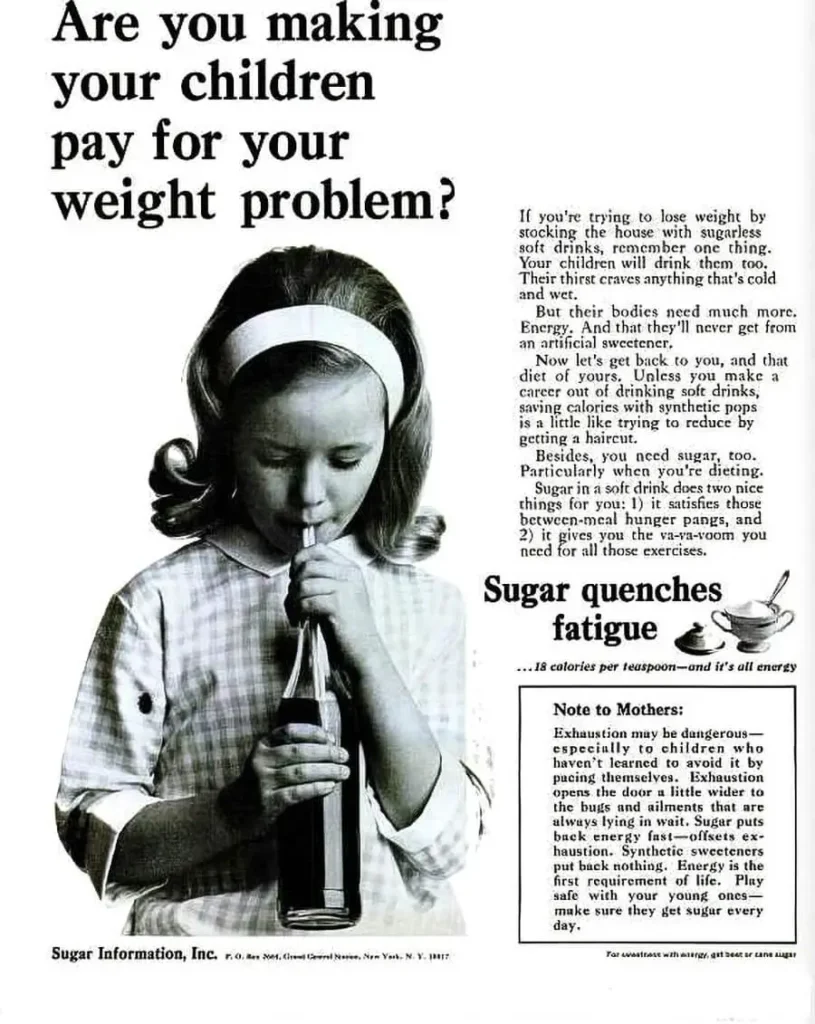
The truth is that tooth decay has only one cause: dietary sugars (Sheiham & James, 2015).
These are the sugars that you eat or drink, such as sucrose (table sugar), glucose, fructose, and lactose. These sugars provide food for the bacteria in your mouth, allowing them to multiply and produce more acids. Without sugars, there would be no tooth decay.
This means that there is no safe level of sugar intake for your teeth. The only way to prevent tooth decay is to avoid or minimize sugar intake as much as possible.
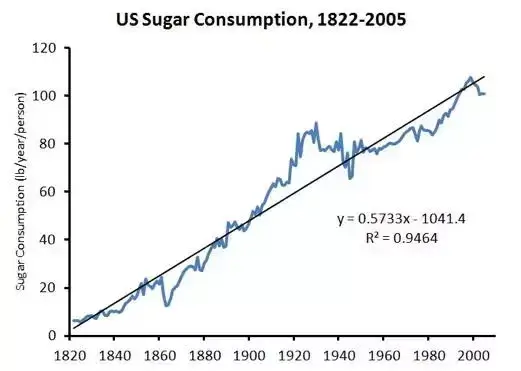
The World Health Organization (WHO) recommends limiting your free sugars intake to less than 10% of your total energy intake per day (World Health Organization: WHO, 2017). Free sugars are the sugars that are added to foods and drinks by the manufacturer, cook, or consumer, as well as the sugars naturally present in honey, syrups, fruit juices, and fruit juice concentrates.
The WHO also suggests that further reducing your free sugars intake to less than 5% of your total energy intake per day would provide additional dental health benefits.
However, most people consume far more sugar than these recommendations. According to the WHO, the global average free sugars intake was 9.9% of total energy intake in 2016. In some regions, such as Africa and the Americas, it was even higher than 15%. This explains why tooth decay is a worldwide epidemic that affects people of all ages and backgrounds.
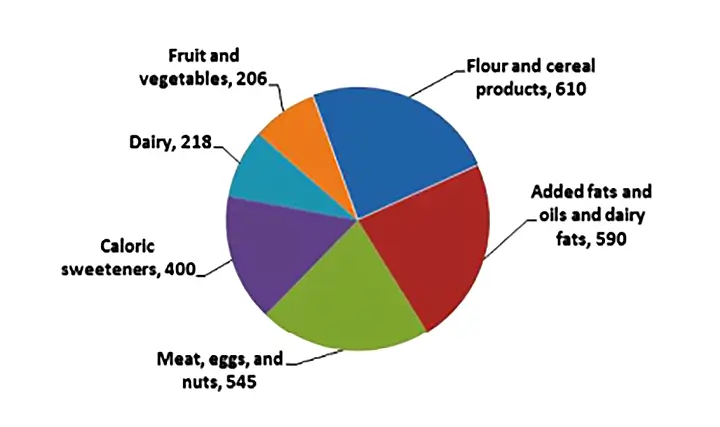
By cutting down on sugars, we can not only protect our teeth from decay but also improve our overall health and well-being. We need to be aware of the hidden sugars in processed foods and drinks, such as soft drinks, candies, cakes, cookies, cereals, sauces, and yogurts. We need to read nutrition labels carefully and choose products with low or no added sugars. We need to limit our consumption of sugary snacks and beverages between meals. We need to eat more fresh fruits and vegetables instead of juices or dried fruits. And we need to drink more water or unsweetened tea or coffee instead of sugary drinks.
Not All Sugars Are Equally Harmful.
Sucrose is a sweet enemy for your teeth. It not only feeds the bacteria that cause tooth decay but also helps them build a sticky and acidic fortress on your enamel.
Sucrose, which is the common table sugar, has a special property that makes it the most cariogenic, or cavity-causing, carbohydrate in our diet. Sucrose can be transformed into extracellular polysaccharides (EPS) by some plaque bacteria, such as Streptococcus mutans (Forssten et al., 2010).
Among different carbohydrates, sucrose is the most effective in stimulating EPS production.
EPSs are extracellular polysaccharides, which are sugars that bacteria produce and release outside their cells. EPSs are often found in dental plaque. You might think that EPSs act like a shield, blocking the acids and sugars from reaching tooth enamel. But that’s not the case. EPSs are not good at stopping diffusion, which means that substances can easily pass through them. So, EPSs don’t protect your teeth from decay by preventing diffusion. In fact, they do the opposite. They make your teeth more vulnerable to decay by providing food for the bacteria.
Some EPSs are water-insoluble, which means they don’t dissolve in water.
These EPSs are a rich source of fermentable sugars, which bacteria can use to produce acids that damage a tooth enamel.
Water-insoluble EPSs also help the bacteria stick to the teeth, making it harder for you to remove them with brushing or flossing.
Mineral Deficiencies.
Mineral deficiencies can affect the formation and structure of the enamel, and therefore its physical properties (Zamojda et al., 2023).
Enamel is the outermost layer of the crown of the tooth and it is highly mineralized, meaning it contains a lot of minerals that make it strong and resistant.
Enamel is not a living tissue like skin or bones. It is developed during the process of odontogenesis, which is the formation of teeth in the embryo. Once your teeth erupt, enamel cannot grow or regenerate. That means that you have to take good care of your enamel because once it is gone, it is gone for good.
But what makes enamel so hard and durable in the first place? The answer lies in its mineral composition. Minerals play a vital role in enamel formation and function, and they may also influence how enamel reacts to different agents that appear in the oral cavity, such as acids, bacteria, or abrasives.
Enamel is mainly made of crystals called hydroxyapatites, which are composed of calcium and phosphate. But enamel also contains trace amounts of other minerals, such as magnesium, zinc, and copper (Zamojda et al., 2023).
These minerals play a vital role in enamel formation and function, and they may also influence how enamel reacts to different agents that appear in the human mouth, such as acids, bacteria, or abrasives.
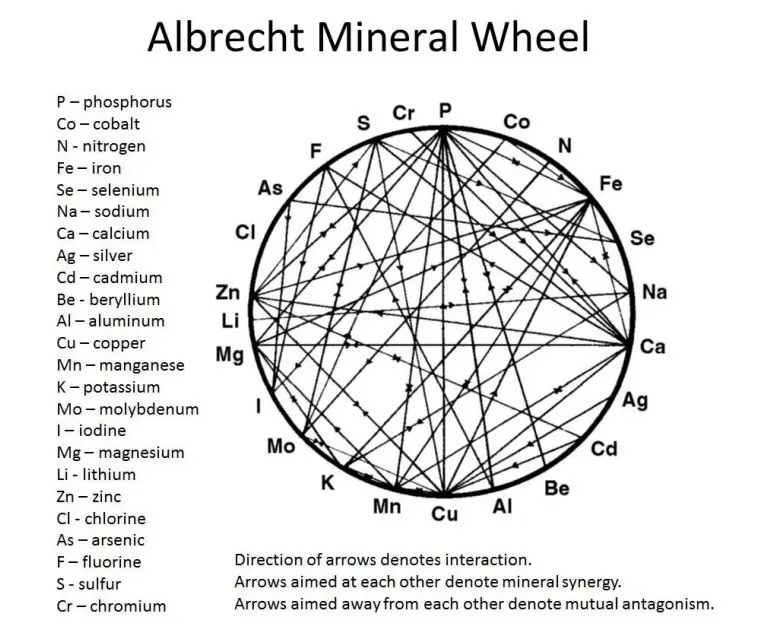
For example, magnesium can influence the activity of an enzyme called alkaline phosphatase, which is involved in the development of properly shaped hydroxyapatite crystals. Magnesium can also inhibit the transition of calcium phosphate from a non-crystallized form to a crystallized form, which affects the structure and hardness of enamel. Magnesium is also a component of the organic matrix of enamel (Klimuszko et al, 2018)
Zinc participates in the metabolism of many factors and proteins that are involved in enamel formation, such as kallikrein 4, alkaline phosphatase, Krox 25 and Krox 26 transcription factors, and enamelysin. Zinc can also protect enamel from acid attack by forming a protective layer on the enamel surface. Zinc is essential for normal enamel formation, and its deficiency can make your enamel weaker. However, too much zinc can also be harmful, as it can inhibit or modify the growth of hydroxyapatite crystals.
Studies on rats have shown that the diet of pregnant mothers can affect the mineral content of dental hard tissues in their offspring. If the mothers have a low intake of magnesium and zinc, their offspring will also have lower levels of these minerals in their teeth. This can make their teeth more vulnerable to dental caries and other pathological agents.
Copper ions can inhibit the formation of dental plaque, the acid solubility of enamel, and the remineralization of enamel. Copper can also prevent bacterial growth and activity by oxidizing their key thiol groups.
Copper can help prevent the demineralization of the enamel by forming an insoluble layer of copper phosphate on the tooth surface. This layer acts as a barrier that reduces the loss of calcium from the enamel and stabilizes its crystal structure. This means that the more copper there is in the solution surrounding the tooth, the more calcium there will be in the enamel, and the less soluble it will be.
Copper also has other benefits for your oral health. For instance, can also inhibit some enzymes that degrade the proteins in the enamel matrix, such as procollagen N-proteinase, glucosyl-transferase, and gelatinase A and B. These enzymes are involved in the formation and maturation of the enamel, and their inhibition can enhance its durability.
In this study (Zamojda et al., 2023), they wanted to compare the content of calcium (Ca), magnesium (Mg), zinc (Zn), and copper (Cu) in different layers of healthy and worn tooth enamel.
Here are some of the main findings:
- They found a statistically significant difference between the mean amount of zinc in severely worn dentition and all the layers of healthy teeth, both in vivo and in vitro. This means that zinc may be lost from enamel due to wear, or that zinc may have a protective effect on enamel against wear.
- They also found strong positive relationships between magnesium and zinc contents at some depths of enamel. This means that these two minerals may have a similar role in enamel formation or function, or that they may influence each other’s uptake or retention in enamel.
- They detected a significant difference between the amount of copper in the severely worn dentitions compared to the superficial layer of the healthy teeth, both in vivo and in vitro. This means that copper may be either depleted or enriched in enamel due to wear or that copper may have an effect on enamel resistance or susceptibility to wear.
In conclusion, the study suggests that zinc metabolism may play an important role in enamel formation and may influence enamel’s resistance to wear after tooth eruption.
It also indicates that magnesium, zinc, and copper may have complex interactions with each other and with other factors that affect enamel structure and function.
Trace Minerals.
Trace minerals are very small amounts of minerals that are present in the body and in the environment. Some examples of trace minerals are zinc, copper, iron, and selenium.
Trace minerals are present in the enamel and can affect its formation and structure.
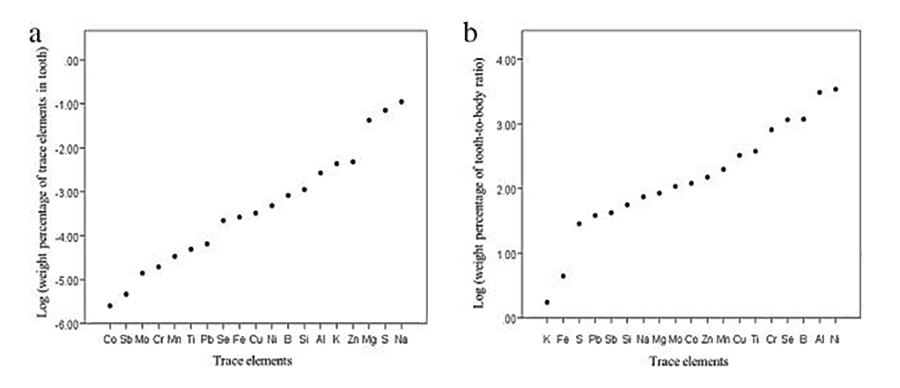
But how many trace elements are in your tooth enamel compared to the rest of your body? To answer this question, scientists conducted a study (Ghadimi et al., 2013) with 38 human teeth that were extracted for various reasons. They measured the concentration of 19 trace elements in the enamel samples.
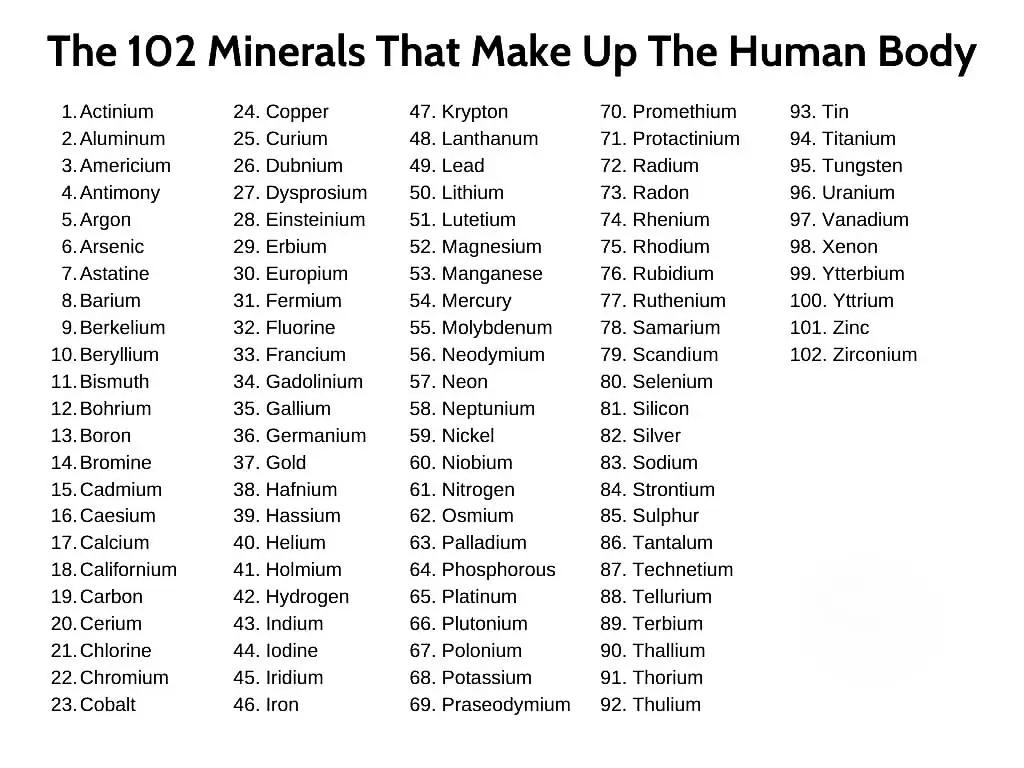
They found that some trace elements had very low concentrations, such as chromium, molybdenum, cobalt, and antimony. These trace elements were barely detectable in the enamel samples. Other trace elements had very high concentrations, such as zinc, sodium, and sulfur. These trace elements were abundant in the enamel samples.
But how do these concentrations compare to the average elemental composition of the human body?
The study found that some trace elements had a similar concentration in the enamel and in the body, such as potassium and iron. These trace elements were evenly distributed throughout the body.
The most abundant trace elements in saliva (Na, Mg, K, and Zn) are also the most abundant trace elements in tooth enamel (Borella et al. 1994; Sighinolfi et al. 1989).
Other trace elements had a higher concentration in the enamel than in the body, such as sulfur, antimony, lead, silicon, sodium, magnesium, molybdenum, cobalt, zinc, manganese, copper, titanium, chromium, selenium, boron, aluminum, and nickel. These trace elements were concentrated in the enamel by 1 (sulfur, antimony, lead, silicon, sodium, and magnesium), 2 (molybdenum, cobalt, zinc, manganese, copper, titanium, and chromium), or 3 orders of magnitude (selenium, boron, aluminum, and nickel).
The most striking difference was for nickel. Nickel was almost 3500 times more abundant in the enamel than in the body. This means that nickel was highly concentrated in the enamel.
Deficiency in trace minerals may have implications for enamel’s health and function. For example, some trace elements may influence enamel’s crystallographic properties and ultimately its physical properties.
Therapy and Challenges.
Do you know how much it costs to replace a missing tooth? Dental caries or tooth decay is one of the most expensive diseases in the world. It affects millions of people, especially children, and can lead to pain, infection, and tooth loss.
You may think that brushing your teeth with fluoride toothpaste and flossing regularly is enough to protect your teeth from caries. But that’s not the whole story.
Caries are caused by bacteria that form a sticky layer on your teeth called biofilm. Biofilm is like a fortress that shields the bacteria from your saliva, toothbrush, and fluoride. It also allows the bacteria to produce acid that erodes your enamel and causes cavities.
So how can we break through this biofilm and stop the bacteria from damaging our teeth?
Scientists have been looking for new ways to fight caries by targeting the biofilm itself. One of the strategies they have explored is using antimicrobial peptides, which are natural substances that can kill bacteria without harming our cells. One example of these peptides is histatin, which is found in our saliva and has a broad-spectrum antimicrobial activity.
Another strategy that scientists have investigated is using inhibitors of exopolysaccharide, which is a type of sugar that the bacteria use to build the biofilm matrix. By blocking this sugar, we can prevent the biofilm from forming and growing. Some studies have shown that combining these inhibitors with fluoride can reduce the amount of exopolysaccharide and acids in the biofilm.
As you can see, there are many promising approaches to prevent and treat caries by targeting the biofilm. But we still have a long way to go before we can use them in clinical practice.
Until then, we should continue to follow the basic rules of oral hygiene: brush twice a day with fluoride toothpaste, floss daily, use mouthwash, limit sugary foods and drinks, and visit your dentist regularly. The most important factor is the diet. Do not consume more than 3 to 5 percent of calories from free sugar and correct mineral deficiencies.
There is no free sugar in nature except honey and all of the produce used to be organic with full spectra of trace minerals in them.
Also, one of the important factors is to use mouthwash to kill bacteria and dissolve biofilm and plaque. Just brushing is not enough.
There are very potent natural nontoxic phytochemicals, antioxidants, and other substances that are good in fighting both candida and bacteria and can be used in homemade natural mouthwash. At the same time, they also provide a high amount of antioxidant and anti-inflammatory support for inflamed gums.
You can read more about it in this article Homemade Natural Mouthwash: Proven, Stronger & Less Toxic.
To summarize, what can you do to protect your oral health and avoid the consequences of sugar? Here are some tips:
- Limit your intake of free sugars to less than 10% of your total energy intake per day, which is about 50 grams or 12 teaspoons for an average adult. If possible, aim for less than 5%, which is about 25 grams or 6 teaspoons per day. Ideally, aim for 3%.
- Use other types of sugars, ideally natural whole food substitutes like date sugar instead of sucralose.
- Brush your teeth twice a day with fluoride toothpaste and floss daily to remove plaque and bacteria from your teeth and gums.
- Visit your dentist regularly for check-ups and professional cleaning to prevent and treat any oral problems.
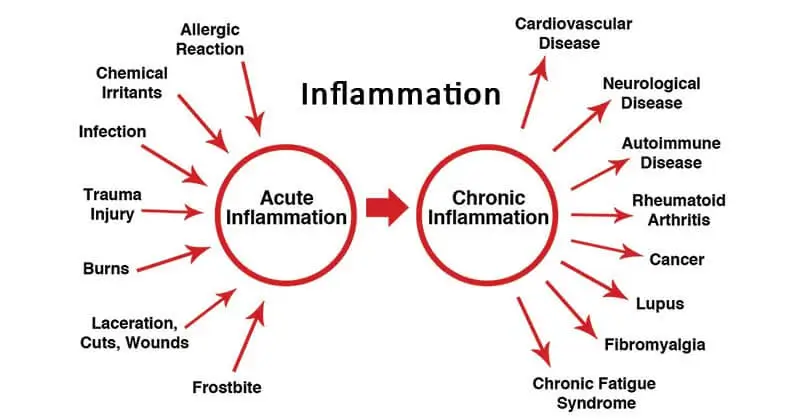
- Avoid smoking, drinking alcohol excessively, eating a diet with a low ORAC score deprived of nutrients, and avoiding pro-inflammatory foods as they can cause chronic inflammation and increase the risk of oral cancer and cancer in general and would inflame the gums and entire body and would lead to oral thrush and candidiasis.
- Support the immune system to keep candida from invading and if you have oral thrush or inflamed gums seek medical treatment.
- Use a mouthwash to kill bacteria and candida and dissolve biofilm and plaque.
- Correct mineral deficiencies.
By following these simple steps, you can enjoy a healthy smile and a healthy life. Remember: sugar may be sweet, but it can also be sour for your oral health. So be smart and choose wisely!
FAQ
References:
- Jørn, A., Paster, B. J., Stokes, L. N., Olsen, I., & Dewhirst, F. E. (2005). Defining the normal bacterial flora of the oral cavity. Journal of Clinical Microbiology, 43(11), 5721–5732. https://doi.org/10.1128/jcm.43.11.5721-5732.2005
- Forssten, S. D., Björklund, M., & Ouwehand, A. C. (2010). Streptococcus mutans, Caries and Simulation Models. Nutrients, 2(3), 290–298. https://doi.org/10.3390/nu2030290
- Metwalli, K. H., Khan, S., Krom, B. P., & Jabra-Rizk, M. A. (2013). Streptococcus mutans, Candida albicans, and the Human Mouth: A Sticky Situation. PLOS Pathogens, 9(10), e1003616. https://doi.org/10.1371/journal.ppat.1003616
- Sheiham, A., & James, W. P. (2015). Diet and Dental Caries: The Pivotal Role of Free Sugars Reemphasized. Journal of dental research, 94(10), 1341–1347. https://doi.org/10.1177/0022034515590377
- Klinke, T., Guggenheim, B., Klimm, W., & Thurnheer, T. (2011). Dental Caries in Rats Associated with Candida albicans. Caries Research, 45(2), 100–106. https://doi.org/10.1159/000324809
- Raja, M., Hannan, A., & Ali, K. (2010). Association of Oral Candidal Carriage with Dental Caries in Children. Caries Research, 44(3), 272–276. https://doi.org/10.1159/000314675
- World Health Organization: WHO. (2017). Sugars and dental caries. www.who.int. https://www.who.int/news-room/fact-sheets/detail/sugars-and-dental-caries
- Zamojda, E., Orywal, K., Mroczko, B., & Sierpińska, T. (2023). Trace elements in dental enamel can be a potential factor of advanced tooth wear. Minerals, 13(1), 125. https://doi.org/10.3390/min13010125
- Ghadimi, E., Eimar, H., Marelli, B., Nazhat, S. N., Asgharian, M., Vali, H., & Tamimi, F. (2013). Trace elements can influence the physical properties of tooth enamel. SpringerPlus, 2, 499. https://doi.org/10.1186/2193-1801-2-499
- Cho, E., Park, Y., Kim, K. Y., Han, D., Kim, H. S., Kwon, J., & Ahn, H. (2021). Clinical characteristics and relevance of oral candida biofilm in Tongue smears. Journal of Fungi, 7(2), 77. https://doi.org/10.3390/jof7020077
- Klimuszko, E., Orywal, K., Sierpinska, T., Sidun, J., & Golebiewska, M. (2018). Evaluation of calcium and magnesium contents in tooth enamel without any pathological changes: in vitro preliminary study. Odontology, 106(4), 369–376. https://doi.org/10.1007/s10266-018-0353-6
Related Posts
Do you have any questions about nutrition and health?
I would love to hear from you and answer them in my next post. I appreciate your input and opinion and I look forward to hearing from you soon. I also invite you to follow us on Facebook, Instagram, and Pinterest for more diet, nutrition, and health content. You can leave a comment there and connect with other health enthusiasts, share your tips and experiences, and get support and encouragement from our team and community.
I hope that this post was informative and enjoyable for you and that you are prepared to apply the insights you learned. If you found this post helpful, please share it with your friends and family who might also benefit from it. You never know who might need some guidance and support on their health journey.
– You Might Also Like –

Learn About Nutrition
Milos Pokimica is a doctor of natural medicine, clinical nutritionist, medical health and nutrition writer, and nutritional science advisor. Author of the book series Go Vegan? Review of Science, he also operates the natural health website GoVeganWay.com
Medical Disclaimer
GoVeganWay.com brings you reviews of the latest nutrition and health-related research. The information provided represents the personal opinion of the author and is not intended nor implied to be a substitute for professional medical advice, diagnosis, or treatment. The information provided is for informational purposes only and is not intended to serve as a substitute for the consultation, diagnosis, and/or medical treatment of a qualified physician or healthcare provider.NEVER DISREGARD PROFESSIONAL MEDICAL ADVICE OR DELAY SEEKING MEDICAL TREATMENT BECAUSE OF SOMETHING YOU HAVE READ ON OR ACCESSED THROUGH GoVeganWay.com
NEVER APPLY ANY LIFESTYLE CHANGES OR ANY CHANGES AT ALL AS A CONSEQUENCE OF SOMETHING YOU HAVE READ IN GoVeganWay.com BEFORE CONSULTING LICENCED MEDICAL PRACTITIONER.
In the event of a medical emergency, call a doctor or 911 immediately. GoVeganWay.com does not recommend or endorse any specific groups, organizations, tests, physicians, products, procedures, opinions, or other information that may be mentioned inside.
Editor Picks –
Milos Pokimica is a health and nutrition writer and nutritional science advisor. Author of the book series Go Vegan? Review of Science, he also operates the natural health website GoVeganWay.com
Latest Articles –
Top Health News — ScienceDaily
- The overlooked nutrition risk of Ozempic and Wegovyon February 4, 2026
Popular weight-loss drugs like Ozempic and Wegovy can dramatically curb appetite, but experts warn many users are flying blind when it comes to nutrition. New research suggests people taking these medications may not be getting enough guidance on protein, vitamins, and overall diet quality, increasing the risk of muscle loss and nutrient deficiencies.
- A 25-year study found an unexpected link between cheese and dementiaon February 4, 2026
A massive Swedish study tracking nearly 28,000 people for 25 years found an unexpected link between full-fat dairy and brain health. Among adults without a genetic risk for Alzheimer’s, eating more full-fat cheese was associated with a noticeably lower risk of developing the disease, while higher cream intake was tied to reduced dementia risk overall. The findings challenge decades of low-fat dietary advice but come with important caveats.
- MIT’s new brain tool could finally explain consciousnesson February 4, 2026
Scientists still don’t know how the brain turns physical activity into thoughts, feelings, and awareness—but a powerful new tool may help crack the mystery. Researchers at MIT are exploring transcranial focused ultrasound, a noninvasive technology that can precisely stimulate deep regions of the brain that were previously off-limits. In a new “roadmap” paper, they explain how this method could finally let scientists test cause-and-effect in consciousness research, not just observe […]
- Why heart disease risk in type 2 diabetes looks different for men and womenon February 4, 2026
Scientists are digging into why heart disease risk in type 2 diabetes differs between men and women—and sex hormones may be part of the story. In a large Johns Hopkins study, men with higher testosterone had lower heart disease risk, while rising estradiol levels were linked to higher risk. These hormone effects were not seen in women. The results point toward more personalized approaches to heart disease prevention in diabetes.
- Sound machines might be making your sleep worseon February 4, 2026
Sound machines may not be the sleep saviors many believe. Researchers found that pink noise significantly reduced REM sleep, while simple earplugs did a better job protecting deep, restorative sleep from traffic noise. When pink noise was combined with outside noise, sleep quality dropped even further. The results suggest that popular “sleep sounds” could be doing more harm than good—particularly for kids.
- This unexpected plant discovery could change how drugs are madeon February 3, 2026
Plants make chemical weapons to protect themselves, and many of these compounds have become vital to human medicine. Researchers found that one powerful plant chemical is produced using a gene that looks surprisingly bacterial. This suggests plants reuse microbial tools to invent new chemistry. The insight could help scientists discover new drugs and produce them more sustainably.
- A hidden cellular process may drive aging and diseaseon February 3, 2026
As we age, our cells don’t just wear down—they reorganize. Researchers found that cells actively remodel a key structure called the endoplasmic reticulum, reducing protein-producing regions while preserving fat-related ones. This process, driven by ER-phagy, is tied to lifespan and healthy aging. Because these changes happen early, they could help trigger later disease—or offer a chance to stop it.
PubMed, #vegan-diet –
- Diet type and the oral microbiomeon February 2, 2026
CONCLUSION: The diet-oral microbiome-systemic inflammation axis is bidirectional and clinically relevant. Understanding both direct ecological regulation and indirect metabolic effects is essential to support precision nutrition strategies aimed at maintaining oral microbial balance and systemic inflammatory risk mitigation.
- Consensus document on healthy lifestyleson January 22, 2026
Proteins are a group of macronutrients that are vital to our lives, as they perform various functions, including structural, defensive and catalytic. An intake of 1.0-1.2 g/kg/body weight per day would be sufficient to meet our needs. Carbohydrate requirements constitute 50 % of the total caloric value and should be obtained mainly in the form of complex carbohydrates. In addition, a daily intake of both soluble and insoluble fiber is necessary. Regular consumption of extra virgin olive oil […]
- Vitamin B12 and D status in long-term vegetarians: Impact of diet duration and subtypes in Beijing, Chinaon January 21, 2026
CONCLUSIONS: This study reveals a dual challenge among Beijing long-term vegetarians: vitamin B12 deficiency was strongly associated with the degree of exclusion of animal products from the diet (veganism), while vitamin D deficiency was highly prevalent and worsened with longer diet duration. The near-universal vitamin D deficiency observed in this study suggests that, in the Beijing context, the risk may extend beyond dietary choice, potentially reflecting regional environmental factors;…
- Nutritional evaluation of duty meals provided to riot police forces in Germanyon January 13, 2026
Background: The primary role of the German riot police is maintaining internal security. Due to challenging working conditions, riot police forces face an elevated risk of various diseases. During duty, forces are provided with meals. A balanced diet can reduce the risk of some of these diseases and contribute to health-promoting working conditions. Aim: First evaluation of the nutritional quality of duty meals in Germany based on German Nutrition Society recommendations (DGE). Methods: In…
- Iodineon January 1, 2006
Iodine is an essential trace nutrient for all infants that is a normal component of breastmilk. Infant requirements are estimated to be 15 mcg/kg daily in full-term infants and 30 mcg/kg daily in preterm infants.[1] Breastmilk iodine concentration correlates well with maternal urinary iodine concentration and may be a useful index of iodine sufficiency in infants under 2 years of age, but there is no clear agreement on a value that indicates iodine sufficiency, and may not correlate with […]
Random Posts –
Featured Posts –
Latest from PubMed, #plant-based diet –
- From paddy soil to dining table: biological biofortification of rice with zincby Lei Huang on February 4, 2026
One-third of paddy soils are globally deficient in zinc (Zn) and 40% of Zn loss in the procession from brown rice to polished rice, which results in the global issue of hidden hunger, e.g., the micronutrient deficiencies in the rice-based population of developing countries. In the recent decades, biofortification of cereal food crops with Zn has emerged as a promising solution. Herein, we comprehensively reviewed the entire process of Zn in paddy soil to human diet, including the regulatory…
- Molecular Characterization of Tobacco Necrosis Virus A Variants Identified in Sugarbeet Rootsby Alyssa Flobinus on February 3, 2026
Sugarbeet provides an important source of sucrose; a stable, environmentally safe, and low-cost staple in the human diet. Viral diseases arising in sugarbeet ultimately impact sugar content, which translates to financial losses for growers. To manage diseases and prevent such losses from occurring, it is essential to characterize viruses responsible for disease. Recently, our laboratory identified a tobacco necrosis virus A variant named Beta vulgaris alphanecrovirus 1 (BvANV-1) in sugarbeet…
- Nutrition in early life interacts with genetic risk to influence preadult behaviour in the Raine Studyby Lars Meinertz Byg on February 3, 2026
CONCLUSIONS: Nutrition in early life and psychiatric genetic risk may interact to determine lasting child behaviour. Contrary to our hypothesis, we find dietary benefits in individuals with lower ADHD PGS, necessitating replication. We also highlight the possibility of including genetics in early nutrition intervention trials for causal inference.
- Effect of the gut microbiota on insect reproduction: mechanisms and biotechnological prospectsby Dilawar Abbas on February 2, 2026
The insect gut microbiota functions as a multifunctional symbiotic system that plays a central role in host reproduction. Through the production of bioactive metabolites, gut microbes interact with host hormonal pathways, immune signaling, and molecular regulatory networks, thereby shaping reproductive physiology and fitness. This review summarizes recent advances in understanding how gut microbiota regulate insect reproduction. Accumulating evidence demonstrates that microbial metabolites…
- Rationale and design of a parallel randomised trial of a plant-based intensive lifestyle intervention for diabetes remission: The REmission of diabetes using a PlAnt-based weight loss InteRvention…by Brighid McKay on February 2, 2026
CONCLUSIONS: This trial will provide high-quality clinical evidence on the use of plant-based ILIs to address the epidemics of obesity and diabetes to inform public health policies and programs in Canada and beyond.
- Diet type and the oral microbiomeby Daniel Betancur on February 2, 2026
CONCLUSION: The diet-oral microbiome-systemic inflammation axis is bidirectional and clinically relevant. Understanding both direct ecological regulation and indirect metabolic effects is essential to support precision nutrition strategies aimed at maintaining oral microbial balance and systemic inflammatory risk mitigation.