Obesity Risk Factors
What are the associated obesity risk factors? For all life on the planet Earth, except for us, food is not a choice.
Milos Pokimica
Written By: Milos Pokimica
Medically Reviewed by: Dr. Xiùying Wáng, M.D.
Updated June 9, 2023The obesity epidemic.
What are the associated obesity risk factors? Animals eat impulsively because they are conditioned to do it for survival. For all life on the planet Earth, food is not a choice. It is a daytime job of survival. The hardest thing for an animal in the wilderness is to gain weight. There is no overabundance in nature because as soon as there is, the number of animals will increase and the new balance will be achieved. This will again create a situation of constant hunger.
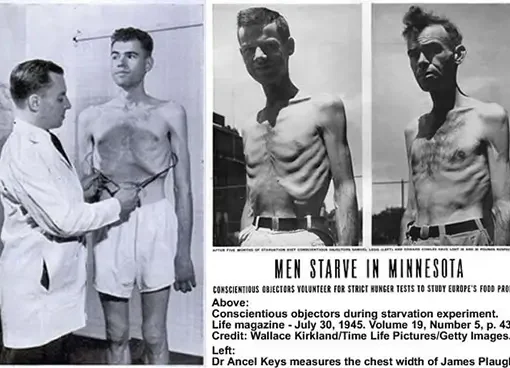
However, in a modern technologically driven society, there is no scarcity. This is the reason why the hardest thing for us is to diet. For most of our evolution, we were slim in a state of constant hunger as any other animal. This was the case for all of our ancestor species and that means the time period of 50 million years. The obesity epidemic today is a maladaptation that is caused by the overabundance of food. This is the new normal and the old normal of dying from starvation is a thing of the ancient past. The problem is that ”ancient” is not really ancient in evolutionary terms. Evolution works for millions of years. The obesity epidemic is therefore more than just a cosmetic issue. It is a health issue that we have to cope with and as a consequence, we will have risk factors that will be associated with it. Being overweight is not a cultural acceptance issue it is a health issue that will never be going to go away.
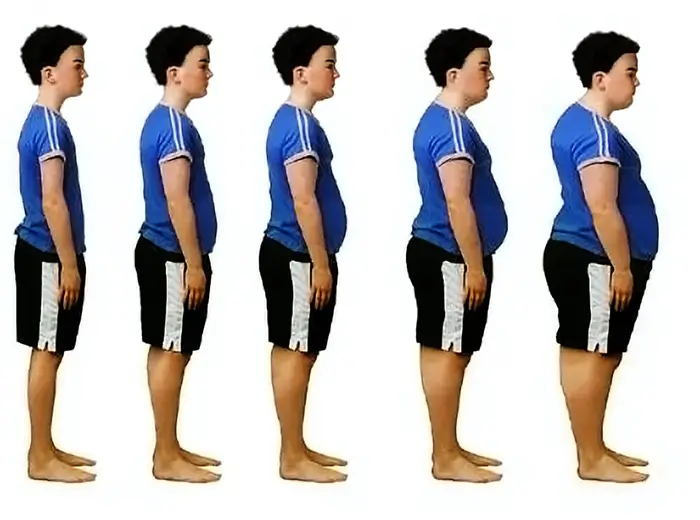
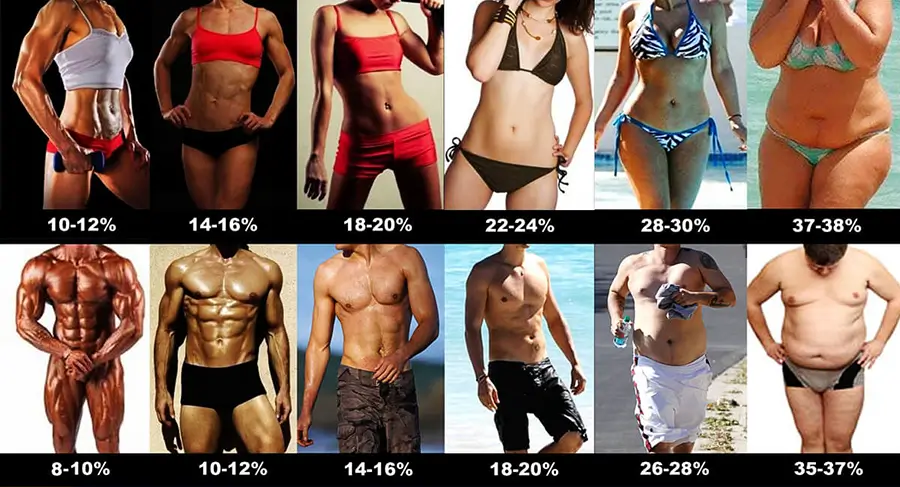
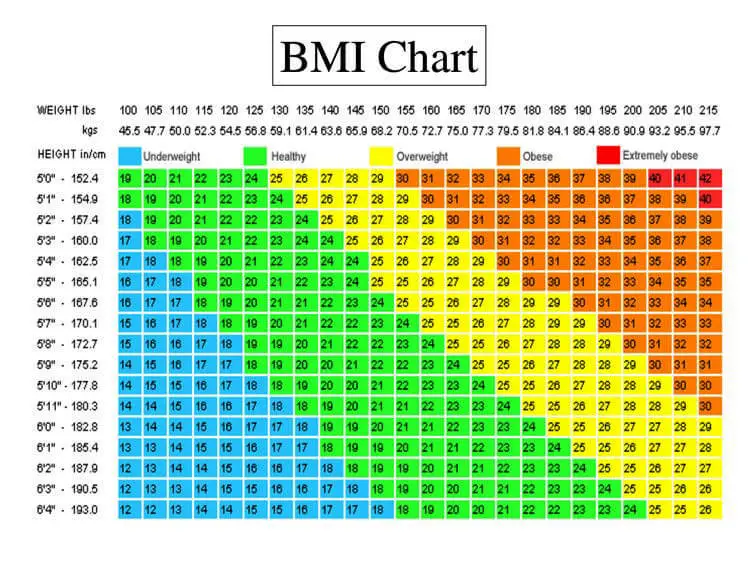
What are the associated obesity risk factors? The body fat percentage (BFP) measures the total fat that you have. Body mass index measures total mass depending on tallness and are different from Body fat percentage. If we have greater muscle mass or larger bones, we will have a higher BMI, so it tells us nothing about fat percentage.
For example, there is the so-called “skinny fat” body type, where you have a high BMI and high BFP or in other words, you are obese and at the same time, you have low muscle mass. Or you can have a high BMI and low BFP like bodybuilders do. Body fat percentage in the leanest athletes is typically at levels of about 6–13% for men or 14–20% for women, this means full six-pack abs and a general shredded look.
Also, there is something called visceral fat, and that is fat that we cannot see. The fat we may be capable of touching on our arms and legs is subcutaneous fat. This internal visceral fat encloses essential organs like the liver, heart, and kidneys and is called organ fat, intra-abdominal fat, or visceral fat. When you are overweight you have more fat inside than you might think. In essence, if we are obese we will have more fat inside than outside. A growing belly can be the result of both types of fat.
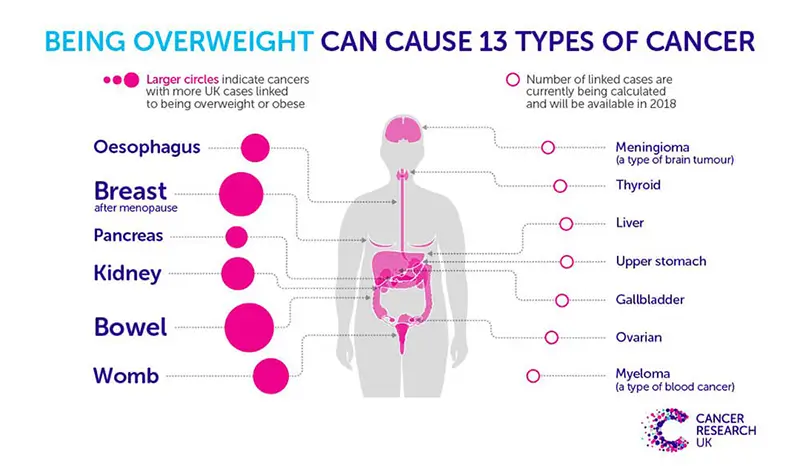
Carrying a large quantity of visceral fat is associated with stroke, heart disease, insulin resistance, osteoarthritis, gout, sleep apnea, asthma, breast cancer, and colorectal cancer. Individuals with a body mass index (BMI) of 30 or higher are considered obese. The term obesity is used to describe individuals who have a weight that can start to cause them health problems and is significantly above their ideal healthy weight. The term morbid obesity is used for individuals that have problems in their regular daily activities due to excessive weight gain. It is a form of disability. Nearly 70% of American adults are either overweight or obese.
Excess weight may increase the risk for many health problems, including:
- Type 2 diabetes
- High blood pressure
- Heart disease and strokes
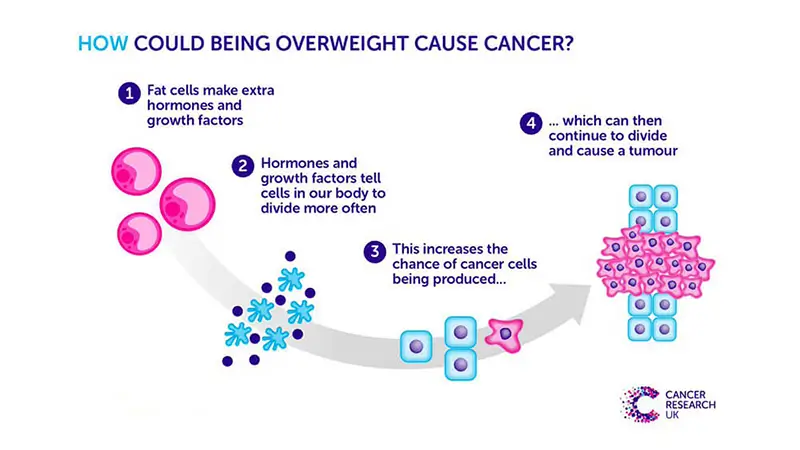
- Certain types of cancer
- Sleep apnea
- Osteoarthritis
- Fatty liver disease
- Kidney disease
- Pregnancy problems (high blood sugar, high blood pressure)
When we talk about risk factors associated with obesity we mean only the diseases that exercise weight is going to create just by itself. In reality, the situation is very different because people that are obese usually at the same time have a very unhealthy diet. It is possible to gain a lot of weight on a nutritionally optimized whole food diet but in reality, extracted sugar and fat and other refined products make a big chunk of calories that creates the excessive caloric intake in the first place.
Having excessive weight in a more realistic condition also means having high cholesterol, high saturated fat, low mineral, low vitamin, low phytochemical and antioxidant, and high pro-inflammatory nutrient-deprived diet. Most of the people that read this will have a hard time understanding that we have in reality a situation where most obese people are also malnourished at the same time. In nutrition, there is a term “junk food” or “empty calorie”. It is similar to the “skinny fat” phenomenon.
Nutrition deficiency affects most of the population at the same time when the population is overweight. Nutritional deficiencies are a wide topic, especially because the land that is used to produce food is depleted and which means that crops will be depleted and that means that animal feed will be deleted. On top of that food is refined and the end result is hypercaloric addictive food filled with calories and nothing much else. In situations where obese people want to go on a calorie-restricted diet and are already malnourished and deficient in most of the essential and non-essential nutrients, we could have a situation that will create a wide range of diseases and all of that diseases will not be directly correlated to obesity but in a sense they are. Eating organic food has much less to do with pesticide residues or with genetically modified organisms but much more to do with low quality eroded land where these food are grown. In organic farming using synthetic fertilizers is forbidden.
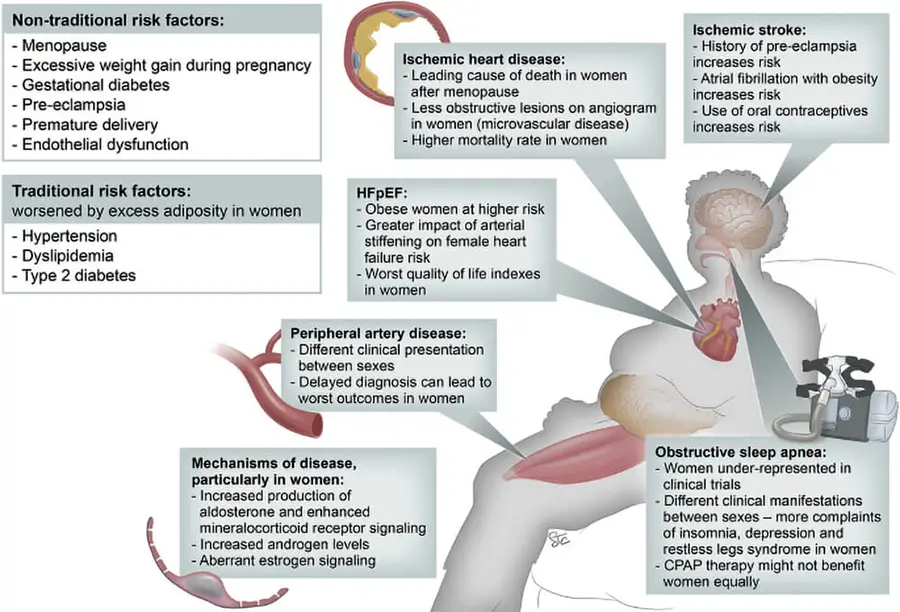
Heart disease and stroke.
Besides carrying large amounts of visceral fat hypercaloric diet also in practice means a higher load of nutrients that our body is also not adapted well to metabolizing. A good example of this is cholesterol. In herbivore species, because they do not eat meat the cholesterol is produced by the liver and they do not need to eat it for their entire life. But when we start to overeat then our body will not be able to metabolize it and that will create additional deposits on blood vessels that will create an increase in risk factors from cardiovascular disease. Obesity on top of that independently just by weight creates increasing pressure on the heart muscle. The increased pressure and all of the cholesterol deposits then create pressure in small or for that measure even larger blood vessels that can be clogged. This will then lower the blood flow and as a response body will increase pressure to increase flow or some of the organs can be left without blood supply. An increase in pressure and deposited fat on the lining and inflammation then can lead to cascading bad effects. Stroke for example is the same disease as a heart attack with a different outcome. Obesity will create a higher risk of stroke. There are actually two main types of stroke, ischemic stroke, and hemorrhagic stroke. In the first one, there will be clogging of the artery and in another type, the artery will burst open. Both of them are associated with obesity.
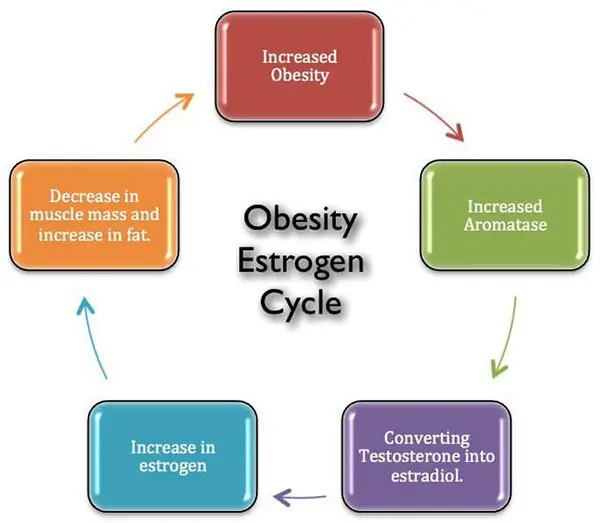
Excess estrogen, low testosterone, and low growth hormone.
Adipose tissue is not a dead organ that sits there and does nothing. It is actually an active organ that has enzymes and is metabolically active. For example, fat cells have enzymes that will metabolize testosterone into estrogen. The enzyme is called aromatase. In breast cancer or in bodybuilding for example one of the goals is to reduce estrogen by blocking its conversion from testosterone by taking aromatase inhibitors. Testosterone is produced at the first instance and only then this enzyme changes it to estrogen. Both are very important hormones and the body needs them both. Unnaturally high levels of fat deposits will create an unnatural level of estrogen and will lower testosterone and that will have cascading effects on the rest of the body (Ylli, 2022).
It is a condition known as hypogonadism (low testosterone) and it usually comes with old age. One of the longevity treatments for the elderly is something known as testosterone replacement therapy which puts the testosterone levels in the elderly in a range of young adults. This can help with muscle wasting, libido, energy and motivation, bone density, and so on. Having low testosterone for both genders is something everyone will want to avoid.
One of the effects will be an increased risk of cancers that are estrogen-responsive such as breast cancer (Picon-Ruiz et al., 2017).
Also, higher estrogen has a wide range of cascading bad effects for itself. One would be polycystic ovarian syndrome. Having disrupted and out of balance levels of androgenic hormones is not just a question of having acne or bodybuilding. It is a serious health issue that affects the quality of life and can create serious diseases.
Disruption in androgenic hormones will also increase infertility (Pasquali et al., 2007). Obesity is associated with subfertility and more than 40% of women seeking obesity surgery do that primarily because they want to have a baby. Infertility in obese patients is correlated to androgen hormone excess on top of insulin resistance (King et al., 2013).
Fat tissue will also suppress the production of growth hormone (Scacchi et al., 1999). Growth hormone deficiency influences a person’s height and helps build bone and muscle. The growth hormone also affects metabolism (the rate at which we burn kilojoules for energy) and will burn fat at a higher rate. One of the strategies of professional athletes is to take a growth hormone to burn fat and build muscle. As for longevity treatment in the elderly, it can also help with a wide range of issues just by itself. A low level of growth hormone can cause a decrease in muscle mass and strength, very low energy levels, reduced bone density, elevated triglyceride levels, and cholesterol, it will affect collagen production and will create dry and thin skin and balding, anxiety and depression, decrease in sexual function.
Fatty liver disease.
Obesity is associated with a spectrum of liver abnormalities, known as nonalcoholic fatty liver disease (NAFLD). Most NAFLD patients are asymptomatic on clinical presentation, even though some may present fatigue, dyspepsia, and dull pain, a general feeling of being unwell and vague discomfort. Treatment for NAFLD involves weight reduction through lifestyle modifications, anti-obesity medication, and bariatric surgery. It is estimated that 75% of obese individuals are at risk of developing a simple fatty liver. A simple fatty liver is far from a “simple” condition. Up to 23% of obese individuals are at risk of developing fatty liver with inflammation. Almost 10% of children may have NAFLD, due in large part to an alarming increase in childhood obesity. In morbidly obese individuals number is 95%. In the picture, you can see how fat goes internally into the cells of the organs. The liver is swollen due to exercise fat intake. In this case, it is done deliberately by force-feeding with a tube. The practice is known as gavage.
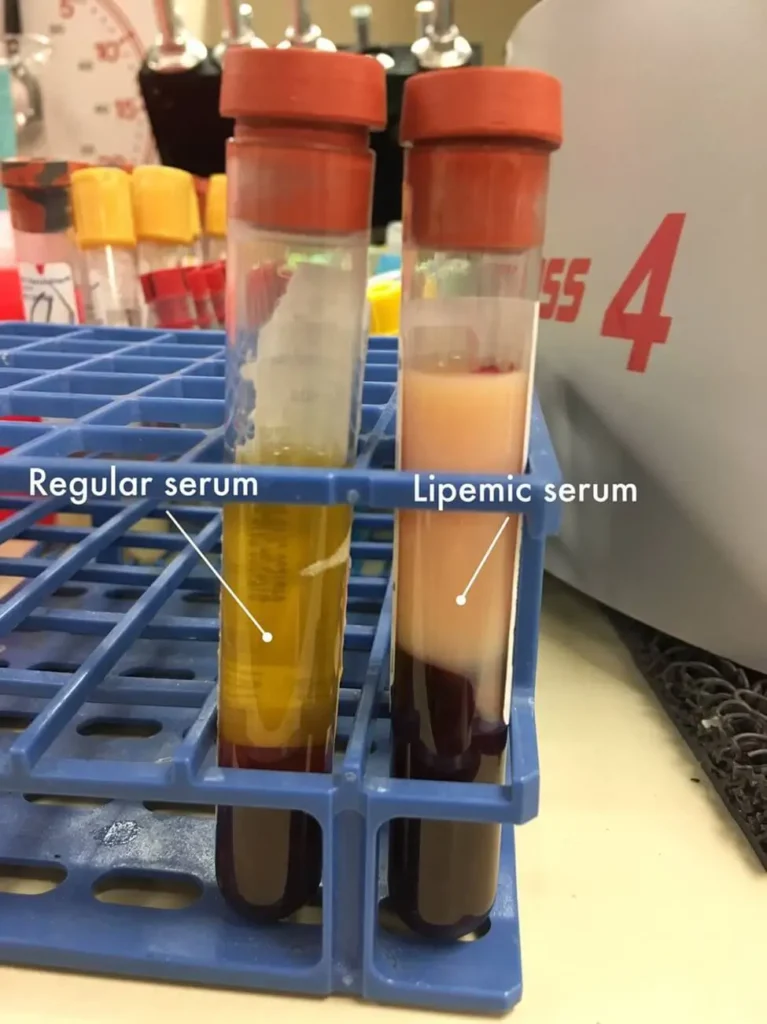
There is also a “spillover” effect where fat cells after a point could not keep all the fat inside them and the fat leeches out to the bloodstream (Almandoz et al., 2013). Fat will then interfere with insulin signaling inside the cells and will increase the resistance of the cells to insulin creating diabetes type 2. Higher blood sugar levels will also suppress growth hormones (Møller et al., 1991). Lipotoxicity also at the same time has the ability to directly kill insulin-producing cells in the pancreas and increase the risk of diabetes type 1 (Engin, 2017).
Joint problems (osteoarthritis).
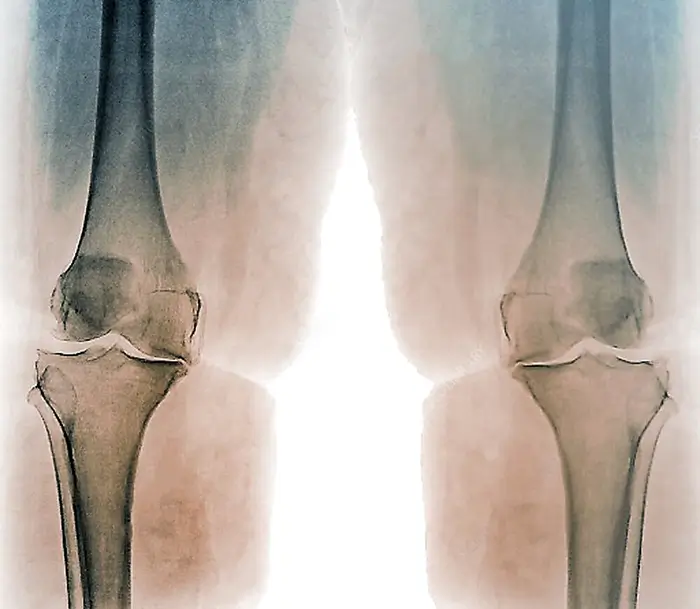
Unlike muscle tissue, the cartage is unable to adapt to the ever-increasing load of weight to the same extent. Cartilage cannot grow to become more resilient because in that case the movement would be obstructed. The consequence is that when we have an ever-larger increase in weight gain that is not congruent with our evolution there is a line where the joints are going to take severe damage in time (King et al., 2013). Obese people will have higher pressure on cartilage and it will wear down over time. There is no difference between being forced to carry bags of cement or being forced to carry excessive fat tissue. There will be physical damage. Then when cartage wears down the inflammation will start or in other words osteoarthritis. Symptoms will include pain, tenderness, swelling, stiffness, grating sensation, and loss of flexibility. This is on top of the loss of flexibility that just excessive weight will cause. In cases of morbid obesity, some people are unable to leave the bad and are unable to stand on their own and this is because of weight on top of any issues that might exist due to arthritis. Osteoarthritis is not an autoimmune disease like rheumatoid arthritis and it is caused just by physical damage to the joints. It is the most common form of arthritis. And it is a “one-way street”.
Sleep apnea.
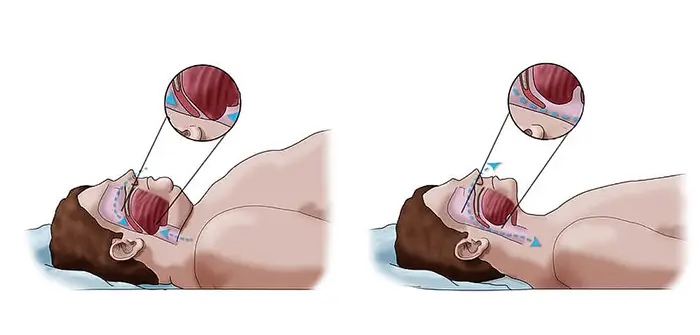
Excessive pressure will also put a lot of strain on muscle tissue that is responsible for breathing and at the same time will obstruct breathing pathways. The narrowest part of that pathway is in the back of our throat and while we are awake that pathway is relatively open. But when we go to sleep the muscles relax and excessive weight will put pressure on them. That will cause closing by narrowing of the opening. This will interrupt breathing and will lower our oxygen intake basically this is a form of suffocation. This can cause not just snoring but interrupted sleep patterns, cardiovascular disease, and premature death. Especially if there is a combination with some other disease that causes swelling like allergies for example or smoking or taking sedatives. Most of the people that are obese have this to some extent and the real problem is that a big chunk of people will have this for a long time before they realize that they have it. When you’re awake, muscles keep. But when you sleep, those muscles relax, allowing the opening to narrow. In Western countries prevalence is estimated at around 2% of women and 4% of men (Schwartz et al., 2008).
Kidney disease.
Why weight gain affects kidneys is largely unknown. There are theories but so far there is no clear answer. It might be a consequence of increased inflammation and oxidative stress, insulin resistance, and hypertension (Kovesdy et al., 2017). As fat goes everywhere it will go to the kidney as well and will create damage by raising inflammation. It is known as a fatty kidney (Foster et al., 1979). The problem with kidneys is that unlike the liver they cannot regenerate themselves. Once the damage is done it will remain for the rest of the life. Having excessive weight will increase the damage and losing weight afterward will not reverse the damage that has already been done. It will also increase the risk of kidney cancer.
Obesity also creates inflammation in the body as a general rule. This means that if we are obese we will have to take a much higher level of antioxidant-rich anti-inflammatory food than someone who is not because we will have a higher level of chronic inflammation that will have a cascading effect and none of them are good. From cancer risk to cardiovascular risk. When inflammation rises the response of the body will be to increase cortisol production by the adrenal glands as it is the main anti-inflammatory hormone of the body. But then that can create high cortisol levels or in other words Cushing’s syndrome. Cortisol is also a stress hormone that puts the body in flight or fight mode and is correlated to different conditions from insomnia, anxiety, and also it is a catabolic hormone that will catabolize muscle mass.
By now you understand that this is just the list of diseases that are directly associated with just excessive weight gain. In real life, this list should be widened because most people that are obese are not on the whole food plant-based nutrient-rich anti-inflammatory, antioxidant-rich, nutrient-dense diet.
References:
- Ylli, D. (2022, September 6). Endocrine Changes in Obesity. Endotext – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK279053/
- Picon-Ruiz, M., Morata-Tarifa, C., Valle-Goffin, J. J., Friedman, E. R., & Slingerland, J. M. (2017). Obesity and adverse breast cancer risk and outcome: Mechanistic insights and strategies for intervention. CA: a cancer journal for clinicians, 67(5), 378–397. https://doi.org/10.3322/caac.21405
- King, L. K., March, L., & Anandacoomarasamy, A. (2013). Obesity & osteoarthritis. The Indian journal of medical research, 138(2), 185–193.[PuMed]
- Scacchi, M., Pincelli, A. I., & Cavagnini, F. (1999). Growth hormone in obesity. International journal of obesity and related metabolic disorders : journal of the International Association for the Study of Obesity, 23(3), 260–271. https://doi.org/10.1038/sj.ijo.0800807
- Almandoz, J. P., Singh, E., Howell, L. A., Grothe, K., Vlazny, D. T., Smailovic, A., Irving, B. A., Nelson, R. H., & Miles, J. M. (2013). Spillover of Fatty acids during dietary fat storage in type 2 diabetes: relationship to body fat depots and effects of weight loss. Diabetes, 62(6), 1897–1903. https://doi.org/10.2337/db12-1407
- Møller, N., Jørgensen, J. O., Abildgård, N., Orskov, L., Schmitz, O., & Christiansen, J. S. (1991). Effects of growth hormone on glucose metabolism. Hormone research, 36 Suppl 1, 32–35.[PubMed]
- Engin A. B. (2017). What Is Lipotoxicity?. Advances in experimental medicine and biology, 960, 197–220. https://doi.org/10.1007/978-3-319-48382-5_8
- King, L. K., March, L., & Anandacoomarasamy, A. (2013). Obesity & osteoarthritis. The Indian journal of medical research, 138(2), 185–193.[PubMed]
- Schwartz, A. R., Patil, S. P., Laffan, A. M., Polotsky, V., Schneider, H., & Smith, P. L. (2008). Obesity and obstructive sleep apnea: pathogenic mechanisms and therapeutic approaches. Proceedings of the American Thoracic Society, 5(2), 185–192. https://doi.org/10.1513/pats.200708-137MG
- Kovesdy, C. P., Furth, S. L., Zoccali, C., & World Kidney Day Steering Committee (2017). Obesity and Kidney Disease: Hidden Consequences of the Epidemic. Canadian journal of kidney health and disease, 4, 2054358117698669. https://doi.org/10.1177/2054358117698669
- Foster, M. C., Hwang, S. J., Porter, S. A., Massaro, J. M., Hoffmann, U., & Fox, C. S. (2011). Fatty kidney, hypertension, and chronic kidney disease: the Framingham Heart Study. Hypertension (Dallas, Tex. : 1979), 58(5), 784–790. https://doi.org/10.1161/HYPERTENSIONAHA.111.175315
- Abraham, S. B., Rubino, D., Sinaii, N., Ramsey, S., & Nieman, L. K. (2013). Cortisol, obesity, and the metabolic syndrome: a cross-sectional study of obese subjects and review of the literature. Obesity (Silver Spring, Md.), 21(1), E105–E117. https://doi.org/10.1002/oby.20083
- Pasquali, R., Patton, L., & Gambineri, A. (2007). Obesity and infertility. Current opinion in endocrinology, diabetes, and obesity, 14(6), 482–487. https://doi.org/10.1097/MED.0b013e3282f1d6cb
- Manrique-Acevedo, C., Chinnakotla, B., Padilla, J., Martinez-Lemus, L. A., & Gozal, D. (2020). Obesity and cardiovascular disease in women. International journal of obesity (2005), 44(6), 1210–1226. https://doi.org/10.1038/s41366-020-0548-0
Related Posts
Do you have any questions about nutrition and health?
I would love to hear from you and answer them in my next post. I appreciate your input and opinion and I look forward to hearing from you soon. I also invite you to follow us on Facebook, Instagram, and Pinterest for more diet, nutrition, and health content. You can leave a comment there and connect with other health enthusiasts, share your tips and experiences, and get support and encouragement from our team and community.
I hope that this post was informative and enjoyable for you and that you are prepared to apply the insights you learned. If you found this post helpful, please share it with your friends and family who might also benefit from it. You never know who might need some guidance and support on their health journey.
– You Might Also Like –

Learn About Nutrition
Milos Pokimica is a doctor of natural medicine, clinical nutritionist, medical health and nutrition writer, and nutritional science advisor. Author of the book series Go Vegan? Review of Science, he also operates the natural health website GoVeganWay.com
Medical Disclaimer
GoVeganWay.com brings you reviews of the latest nutrition and health-related research. The information provided represents the personal opinion of the author and is not intended nor implied to be a substitute for professional medical advice, diagnosis, or treatment. The information provided is for informational purposes only and is not intended to serve as a substitute for the consultation, diagnosis, and/or medical treatment of a qualified physician or healthcare provider.NEVER DISREGARD PROFESSIONAL MEDICAL ADVICE OR DELAY SEEKING MEDICAL TREATMENT BECAUSE OF SOMETHING YOU HAVE READ ON OR ACCESSED THROUGH GoVeganWay.com
NEVER APPLY ANY LIFESTYLE CHANGES OR ANY CHANGES AT ALL AS A CONSEQUENCE OF SOMETHING YOU HAVE READ IN GoVeganWay.com BEFORE CONSULTING LICENCED MEDICAL PRACTITIONER.
In the event of a medical emergency, call a doctor or 911 immediately. GoVeganWay.com does not recommend or endorse any specific groups, organizations, tests, physicians, products, procedures, opinions, or other information that may be mentioned inside.
Editor Picks –
Milos Pokimica is a doctor of natural medicine, clinical nutritionist, medical health and nutrition writer, and nutritional science advisor. Author of the book series Go Vegan? Review of Science, he also operates the natural health website GoVeganWay.com
Latest Articles –
Plant Based News
-
10 High-Protein Dessert Recipes
on July 12, 2025
-
How To Make Creamy Chocolate Oat Milk Without Sugar Or Oil
on July 11, 2025
-
Vegan Quinoa And Feta Salad
on July 11, 2025
-
‘If I Could Only Make One Plant-Based Recipe, This Would Be It’
on July 10, 2025
-
5-Ingredient Vegan Bread And Butter Pudding
on July 10, 2025
-
10 Quick Vegan Weekday Breakfasts
on July 9, 2025
-
This Tempeh Parmesan Recipe Has Gone Viral For A Reason
on July 8, 2025
Top Health News — ScienceDaily
- Florida cat sniffs out another new virus—and scientists are listeningon July 12, 2025
A cat named Pepper has once again helped scientists discover a new virus—this time a mysterious orthoreovirus found in a shrew. Researchers from the University of Florida, including virologist John Lednicky, identified this strain during unrelated testing and published its genome. Although once thought to be harmless, these viruses are increasingly linked to serious diseases in humans and animals. With previous discoveries also pointing to a pattern of viral emergence in wildlife, scientists […]
- Scientists just found 200+ hidden proteins that may drive Alzheimer’son July 12, 2025
A surprising new study has uncovered over 200 misfolded proteins in the brains of aging rats with cognitive decline, beyond the infamous amyloid and tau plaques long blamed for Alzheimer’s. These shape-shifting proteins don’t clump into visible plaques, making them harder to detect but potentially just as harmful. Scientists believe these “stealth” molecules could evade the brain’s cleanup systems and quietly impair memory and brain function. The discovery opens a new frontier in […]
- It’s never too late: Just moving more could add years to your lifeon July 12, 2025
Adopting a physically active lifestyle at any stage of adulthood significantly lowers your risk of dying from any cause, especially from cardiovascular disease. A sweeping analysis of 85 studies confirms that those who stay active consistently reduce their mortality risk by 30–40%, while even those who become active later in life enjoy a 20–25% reduction.
- Researchers grow 400+ brain cell types—a leap for Alzheimer’s and Parkinson’s researchon July 12, 2025
Scientists at ETH Zurich have broken new ground by generating over 400 types of nerve cells from stem cells in the lab, far surpassing previous efforts that produced only a few dozen. By systematically experimenting with combinations of morphogens and gene regulators, the researchers replicated the vast diversity of neurons found in the human brain. This breakthrough holds major promise for studying neurological diseases like Alzheimer’s and Parkinson’s, creating more accurate models for […]
- This tiny brain molecule could hold the key to learning, memory—and Alzheimer’s treatmenton July 12, 2025
A team of researchers has discovered that a protein called cypin plays a powerful role in helping brain cells connect and communicate, which is crucial for learning and memory. By uncovering how cypin tags certain proteins at synapses and interacts with the brain’s protein recycling system, scientists are opening doors to possible treatments for Alzheimer’s, Parkinson’s, and traumatic brain injuries. This breakthrough could be the first step toward boosting brain resilience and cognition.
- Breakthrough microchip reveals how your body fights viruses—in just 90 minuteson July 12, 2025
A team at Scripps Research has created a microchip that can rapidly reveal how a person’s antibodies respond to viruses using only a drop of blood. This game-changing technology, called mEM, condenses a week’s worth of lab work into 90 minutes, offering a powerful tool for tracking immune responses and fast-tracking vaccine development. Unlike earlier methods, it needs far less blood and delivers more detailed insights, even revealing previously undetected antibody targets on viruses like […]
- The first pandemic? Scientists find 214 ancient pathogens in prehistoric DNAon July 11, 2025
Scientists have uncovered DNA from 214 ancient pathogens in prehistoric humans, including the oldest known evidence of plague. The findings show zoonotic diseases began spreading around 6,500 years ago, likely triggered by farming and animal domestication. These ancient infections may still influence us today, and help guide the vaccines of tomorrow.
PubMed, #vegan-diet –
- Effects of different dietary patterns on glucose management in type 1 diabetes: a systematic review and meta-analysis of randomized controlled trialson July 11, 2025
BACKGROUND: Effective glucose management is essential to prevent complications in type 1 diabetes. While nutrition therapy is crucial, the optimal diet remains uncertain. Our systematic review and meta-analysis synthesized evidence from randomized controlled trials (RCTs) on the impact of various diets on glucose management in type 1 diabetes.
- Dietary acid load on the Mediterranean and a vegan diet: a secondary analysis of a randomized, cross-over trialon July 10, 2025
CONCLUSION: These findings suggest that, compared with the Mediterranean diet, dietary acid load decreased significantly on the low-fat vegan diet and was associated with weight loss. The alkalizing effect of a vegan diet may be an independent mechanism by which a vegan diet promotes weight loss.
- Effects of vegan diets and lifestyle on adult body composition: a narrative reviewon July 10, 2025
The health benefits of vegan diets are well documented, though achieving nutritional adequacy requires careful planning, as is the case with any well-designed diet. Vegan diets effectively address obesity, with emerging evidence suggesting that body composition analysis offers a more accurate assessment of body weight management than traditional body mass index (BMI) calculations. This narrative review evaluates the impact of vegan diets on adult body composition based on 16 human […]
- Framing the meat consumption transition: A statistical learning approach to explore the factors shaping young adults’ food choices in Germany and Italyon July 6, 2025
This study examines the factors driving changes in meat consumption among young adults in Germany and Italy-two high-income countries that, despite their distinct culinary traditions, have seen a convergence in meat consumption levels in recent years. The research addresses two aims: to examine the role of environmental attitudes in shaping dietary choices and to explore the impact of socio-demographic factors on meat-consumption patterns. The analysis employs the General Ecological Behavior…
- Health and environmental impacts of shifting to plant-based analogues: a risk-benefit assessmenton July 5, 2025
CONCLUSION: PBAs can be considered feasible alternatives to animal-based foods, and the results emphasise meat substitution as a crucial factor for health and environmental benefits.
Random Posts –
Featured Posts –

Latest from PubMed, #plant-based diet –
- Association between protein diet score and colorectal adenomas risk: a prospective studyby Yangpiaoyi Shi on July 11, 2025
CONCLUSION: Our findings indicate that higher Protein Diet Score is associated with reduced colorectal adenoma incidence among middle-aged and elderly Americans, with similar findings observed for the PAR. These results provide important evidence for optimizing protein intake and source composition to promote intestinal health.
- Dietary acid load on the Mediterranean and a vegan diet: a secondary analysis of a randomized, cross-over trialby Hana Kahleova on July 10, 2025
CONCLUSION: These findings suggest that, compared with the Mediterranean diet, dietary acid load decreased significantly on the low-fat vegan diet and was associated with weight loss. The alkalizing effect of a vegan diet may be an independent mechanism by which a vegan diet promotes weight loss.
- Impact of Elateriospermum tapos Supplementation on Leptin and Hypothalamic Signaling in Female Offspring of High-Fat Diet-Induced Obeseby Santhra Segaran Balan on July 10, 2025
CONCLUSION: In conclusion, the E. tapos shell significantly reduced maternal obesity in female offspring at PND21 compared to its seed.
- Effects of diet on sperm functionality and cryopreservation tolerance in Atlantic salmon (Salmo salar)by Elías Figueroa Villalobos on July 10, 2025
This study evaluates the impact of dietary composition on the functionality and cryopreservation tolerance of intratesticular spermatozoa in Atlantic salmon (Salmo salar). A total of 40 males were divided into four dietary treatment groups: Diet I, based on marine-derived lipids and proteins; Diet II, replacing 65 % of marine proteins and 51 % of lipids with plant and terrestrial animal sources; and two commercial reference diets (III and IV) to contrast with the experimental diets. Over a…
- Healthy Plant-Based Diet Is Associated With a Reduced Risk of Inflammatory Bowel Disease: A Large-Scale Prospective Analysisby Zhenhe Jin on July 9, 2025
Current studies indicated a potential inverse association between plant-based diets (PBD) and inflammatory bowel disease (IBD). Large-scale research is needed to confirm the protective role of PBD in IBD risk. This study evaluated the associations between PBD and IBD risk and explored potential mediators. This prospective cohort study included 143 434 UK Biobank participants, using 24-h dietary recalls to calculate PBD indexes. Cox regression assessed associations between PBD and IBD risk….
- Associations of nutritional knowledge with dietary patterns and breast cancer occurrenceby Beata Stasiewicz on July 9, 2025
It is well-established that women’s nutrition knowledge (NK) is strongly associated with children’s nutritional outcomes. However, the association of women’s NK with their own diet and health status, including cancer occurrence, remains unknown. This case-control study aimed to assess the associations of NK with dietary patterns (DPs) and breast cancer (BC) occurrence in peri- and postmenopausal women. Data were collected for 417 women aged 40.0-79.9 years from north-eastern Poland, including…