Binge Eating and Hormonal Regulation: Emotional Hunger
Our entire evolution, we were like any other species on this planet, in constant hunger and in search of food. Overeating is an example of maladaptation.
Milos Pokimica
Written By: Milos Pokimica
Medically Reviewed by: Dr. Xiùying Wáng, M.D.
Updated June 9, 2023For our entire evolution, we were like any other species on this planet in constant search of food. We were not obese but in a state of constant hunger and constant physical activity. This was the case for all of our ancestor species and that means the time period of 50 million years.
Technological progress that happened in the last couple of hundreds of years didn’t change our body physiology. It is an abrupt shift in evolutional terms. The feeling of constant fullness, on the other hand, is not natural, and it is an example of maladaptation. Our hominin ancestors and even homo sapiens dint have technology and food on every corner. Hunger is a normal feeling and it is a normal feeling for every animal. Because of our evolutionary conditioning and the way our brain works, people even if we are on a restrictive diet cannot deal with the feeling of constant hunger. We want to have a feeling of fullness and there is nothing we can do about it. So here comes caffeine, hunger suppressors of different kinds and medicine and surgeries, and so on.
In an evolutionary sense, this is protective behavior, because there is an extreme scarcity of food, bingeing as much as we possibly can is a good survival strategy. But what happens when we have an overabundance of food and we never had that abundance during our entire existence including our direct ancestor species. Our evolution didn’t begin with the modern human species we have just become a little smarter. Most of our genes and the body are the same, especially in basic survival mechanisms that didn’t have to change for millions of years.
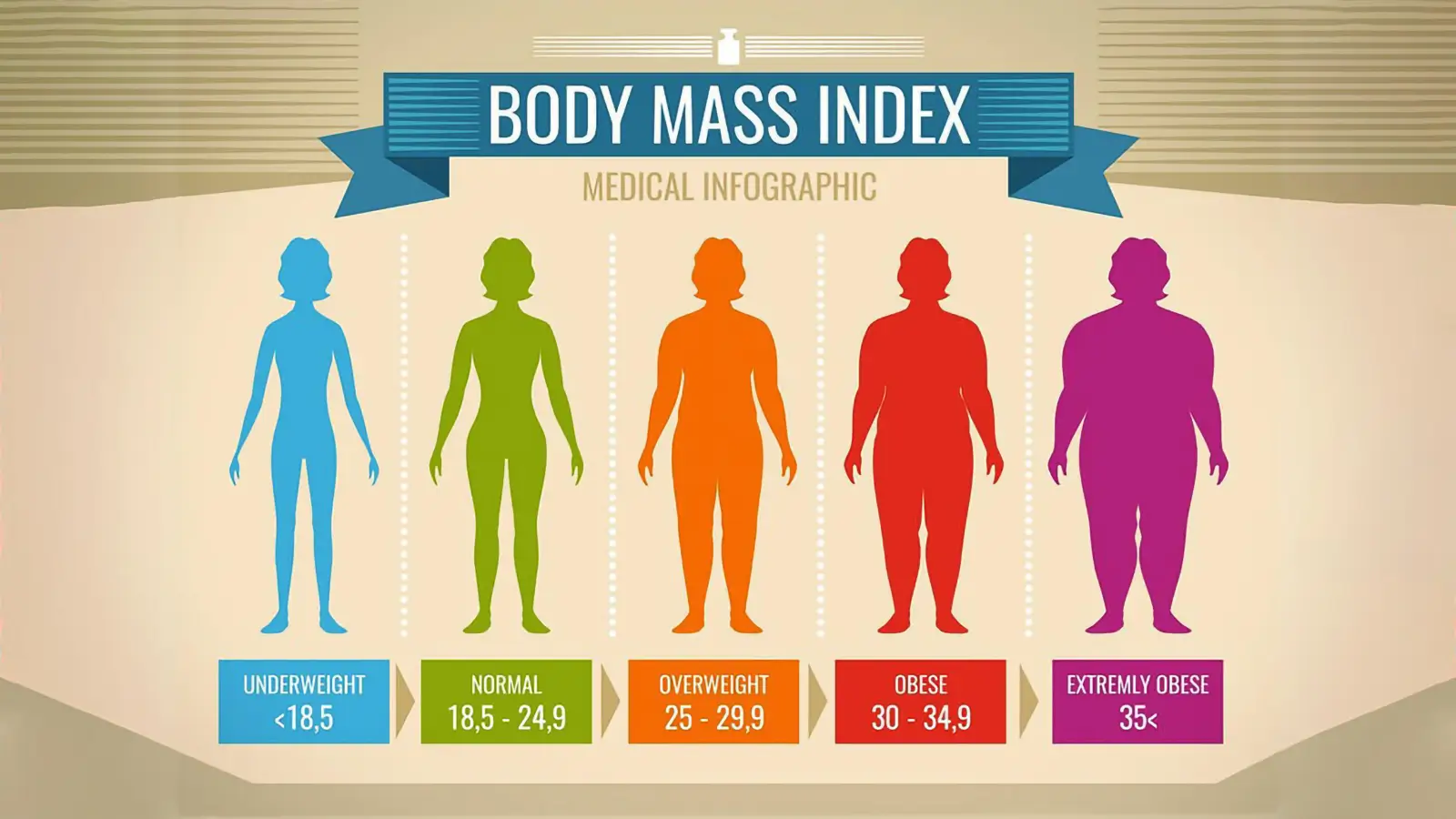
All of this would not have to be an issue but obesity is everything but a cosmetic issue. Most people do understand this but are unable to do anything about it because of fear of starvation. This fear is instinctive and it would override any logical behavior and in reality, we would always overeat. Weight gain comes slowly and in a prolonged period. Even if we gain just a little on a monthly basis, in time this little would be too much.
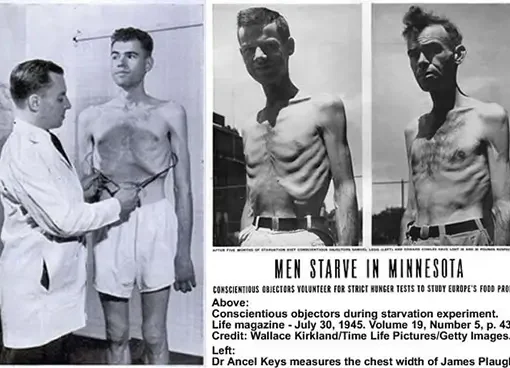
When an individual starts to have a restrictive diet the instinctive fear of starvation will have an impact on behavior and more than just in the psychological way. It will trigger different pathways in the brain that are responsible for appetite control, fear, reward mechanism (how much pleasure we get from pleasurable experiences), and most of our brain functioning. And this will not stop when we go off the diet but will continue as a never-ending story. It is a so-called “yo-yo” effect. Even since a Minnesota starvation experiment (Kelesidis et al., 2010) scientists have been aware of the full scope of effects that a restrictive diet can have on someone’s behavior.
The way that the brain works is by the “carrot and a stick” mechanism. Number one would be the avoidance of pain, and when pain is avoided pleasure-seeking comes into play.
The more pain the stronger behavioral changes. The problem is until the pain is removed the pleasure-seeking does not exist. For example, people in the Minnesota starvation experiment after a period of time couldn’t think of anything else except food. They could not take the pain of constant hunger. After they were given food the fear of starvation never went away and they were overeating and binging as much as they could and have become obese in a very short period. But this behavior exists just to a smaller extent in everyday “normal” behavior. The most normal feeling of hunger had become much more pronounced because today we cannot deal with hunger because we have never experienced the real level of starvation. That is the reason why most of us cannot really cope well with dieting because we do not have tolerance for pain anymore. And even if we do, the normal response of the brain will be to go into survival avoidance of pain mode and cut off all pleasure-seeking behavior until the hunger is removed. It is not possible to be in a state of hunger and enjoy life. Especially because now we are removed from our natural environment and we have supernormal stimuli everywhere. Even a normal feeling of hunger is something that we cannot take as a normal feeling anymore.
Our behavior has been conditioned in such a way that our brain has down-regulated its pleasure response. For example, this happens to heroin addicts. Heroin is one of the strongest drugs in existence. It gives a lot of pleasure. But in time addicts will become more tolerant of the effects of it to some extent because their brain adapts. The same thing has happened in our modern society. Our brain has to some extent adapted to supernormal stimuli from food and hunger has become a much more pronounced feeling than it would be in normal animal species. Because of lack of scarcity food is not as a big reward as it used to be especially because of unnaturally high concentrations and combinations of energy sources that do not exist in nature.
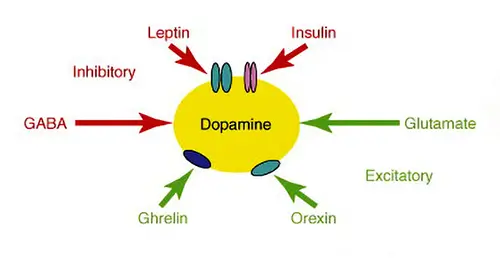
Extracted sugar and extracted fat do not exist in nature and it is digested much quicker than in normal circumstances from whole food sources giving us a dopamine high. Especially the combination of sugar and fat (Zhang et al., 2005). This combination does not exist in nature. Because of this dieting has become a form of addiction much more than it would be in a natural environment.
The result of this is that we have become obese and there is nothing we can do about it. Today nearly 70% of American adults are either overweight or obese.
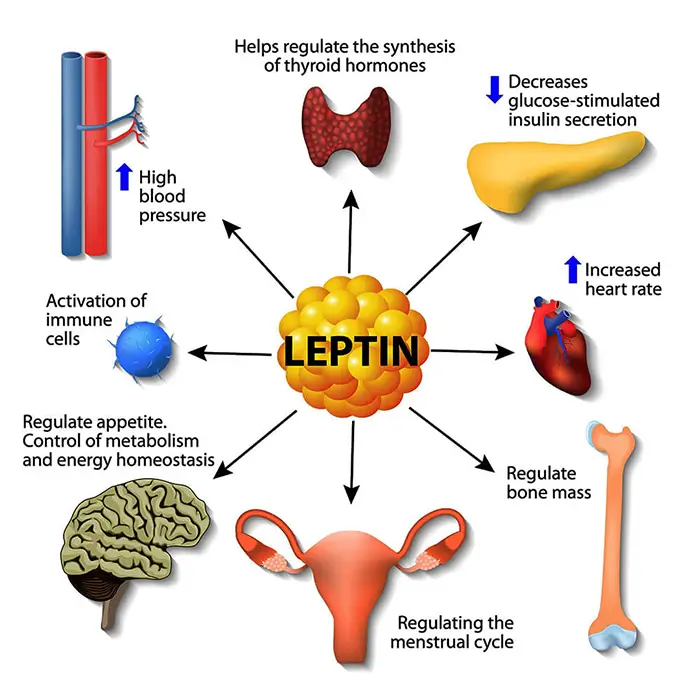
Actually, even anorexia nervosa patients are victims of the same maladaptation. It is not a psychological issue it is conditioned behavior of pleasure and pain reward mechanisms. In anorexia patients, there is also malfunction but in the opposite direction. When they refeed themselves, their plasma leptin concentration will increase rapidly and reach roughly normal levels long before normal weight is achieved (Obradovic et al., 2021). Thus keeping them anorexic. They experience hunger much less than someone that does not have this condition. Excessive leptin production and its effect on the feeling of fullness could play a permissive role in the pathogenesis of this condition.
Leptin is the satiety hormone, and it is opposed by the actions of another hormone named ghrelin, the hunger hormone. Both hormones act on the receptors in the brain to regulate appetite (Zhang et al., 2017). When people think that their conscious mind will have an impact on their behavior I always asked them to do an experiment and try to keep their breath. After a minute or so there will be pain singling and the unconscious part of the brain will override our behavior. The signal is due to the fact that the brain is dying and no matter what, you have to take oxygen in or die. We will gasp for breath no matter how strongly we resist. This is a reason that someone can drown in 20 seconds if panic kicks in. The same behavior changes affect our day-to-day behavior in regard to the water we drink, the air we breathe and the food we eat.
The balance of these two hormones is necessary to achieve an overall energy balance in the body. In obesity, a decreased sensitivity to leptin occurs (Anderberg et al., 2016). This is a big problem that will result in a brain’s inability to detect satiety despite high energy stores in the rest of the body. Why does this happen? The basis for leptin resistance in obese human subjects is unknown. If leptin levels remain persistently raised due to overeating, there may be a downregulation of the leptin receptors and hence decreased sensitivity to the hormone. In humans, and actually in any other animal low leptin levels induced by a low-calorie diet resulted in a decrease in plasma leptin concentration triggering high levels of constant hunger. This may explain the high failure rate of dieting. Low leptin levels are likely to be a powerful stimulus to weight gain.
In the case of obesity, the standard regulatory system will tell the brain that we have fat deposits stored for an extended period and that we can endure little hunger. The problem is that we could never become fat due to scarcity, so we never developed an adaptation to the abundance of food. Our mind still thinks that if we do not eat all that we can we will starve to death in the upcoming drought.
References:
- Kelesidis, T., Kelesidis, I., Chou, S., & Mantzoros, C. S. (2010). Narrative review: the role of leptin in human physiology: emerging clinical applications. Annals of internal medicine, 152(2), 93–100. https://doi.org/10.7326/0003-4819-152-2-201001190-00008
- Zhang, F., Chen, Y., Heiman, M., & Dimarchi, R. (2005). Leptin: structure, function and biology. Vitamins and hormones, 71, 345–372. https://doi.org/10.1016/S0083-6729(05)71012-8
- Obradovic, M., Sudar-Milovanovic, E., Soskic, S., Essack, M., Arya, S., Stewart, A. J., Gojobori, T., & Isenovic, E. R. (2021). Leptin and Obesity: Role and Clinical Implication. Frontiers in endocrinology, 12, 585887. https://doi.org/10.3389/fendo.2021.585887
- Zhang, Y., & Chua, S., Jr (2017). Leptin Function and Regulation. Comprehensive Physiology, 8(1), 351–369. https://doi.org/10.1002/cphy.c160041
- Anderberg, R. H., Hansson, C., Fenander, M., Richard, J. E., Dickson, S. L., Nissbrandt, H., Bergquist, F., & Skibicka, K. P. (2016). The Stomach-Derived Hormone Ghrelin Increases Impulsive Behavior. Neuropsychopharmacology : official publication of the American College of Neuropsychopharmacology, 41(5), 1199–1209. https://doi.org/10.1038/npp.2015.297
- Kalm, L. M., & Semba, R. D. (2005). They starved so that others be better fed: remembering Ancel Keys and the Minnesota experiment. The Journal of nutrition, 135(6), 1347–1352. https://doi.org/10.1093/jn/135.6.1347
- Tobey J. A. (1951). The Biology of Human Starvation. American Journal of Public Health and the Nations Health, 41(2), 236–237.[PubMed]
- Howick, K., Griffin, B. T., Cryan, J. F., & Schellekens, H. (2017). From Belly to Brain: Targeting the Ghrelin Receptor in Appetite and Food Intake Regulation. International journal of molecular sciences, 18(2), 273. https://doi.org/10.3390/ijms18020273
- Müller, M. J., Enderle, J., Pourhassan, M., Braun, W., Eggeling, B., Lagerpusch, M., Glüer, C. C., Kehayias, J. J., Kiosz, D., & Bosy-Westphal, A. (2015). Metabolic adaptation to caloric restriction and subsequent refeeding: the Minnesota Starvation Experiment revisited. The American journal of clinical nutrition, 102(4), 807–819. https://doi.org/10.3945/ajcn.115.109173
- Dulloo A. G. (2021). Physiology of weight regain: Lessons from the classic Minnesota Starvation Experiment on human body composition regulation. Obesity reviews : an official journal of the International Association for the Study of Obesity, 22 Suppl 2, e13189. https://doi.org/10.1111/obr.13189
- LASKER G. W. (1947). The effects of partial starvation on somatotype: an analysis of material from the Minnesota starving experiment. American journal of physical anthropology, 5(3), 323–341. https://doi.org/10.1002/ajpa.1330050305
- Dulloo, A. G., Jacquet, J., & Girardier, L. (1996). Autoregulation of body composition during weight recovery in human: the Minnesota Experiment revisited. International journal of obesity and related metabolic disorders : journal of the International Association for the Study of Obesity, 20(5), 393–405.[PubMed]
- Keys et al. (1950) “The Biology of Human Starvation (2 volumes)”. University of Minnesota Press.
Related Posts
Sources:
Do you have any questions about nutrition and health?
I would love to hear from you and answer them in my next post. I appreciate your input and opinion and I look forward to hearing from you soon. I also invite you to follow us on Facebook, Instagram, and Pinterest for more diet, nutrition, and health content. You can leave a comment there and connect with other health enthusiasts, share your tips and experiences, and get support and encouragement from our team and community.
I hope that this post was informative and enjoyable for you and that you are prepared to apply the insights you learned. If you found this post helpful, please share it with your friends and family who might also benefit from it. You never know who might need some guidance and support on their health journey.
– You Might Also Like –

Learn About Nutrition
Milos Pokimica is a doctor of natural medicine, clinical nutritionist, medical health and nutrition writer, and nutritional science advisor. Author of the book series Go Vegan? Review of Science, he also operates the natural health website GoVeganWay.com
Medical Disclaimer
GoVeganWay.com brings you reviews of the latest nutrition and health-related research. The information provided represents the personal opinion of the author and is not intended nor implied to be a substitute for professional medical advice, diagnosis, or treatment. The information provided is for informational purposes only and is not intended to serve as a substitute for the consultation, diagnosis, and/or medical treatment of a qualified physician or healthcare provider.NEVER DISREGARD PROFESSIONAL MEDICAL ADVICE OR DELAY SEEKING MEDICAL TREATMENT BECAUSE OF SOMETHING YOU HAVE READ ON OR ACCESSED THROUGH GoVeganWay.com
NEVER APPLY ANY LIFESTYLE CHANGES OR ANY CHANGES AT ALL AS A CONSEQUENCE OF SOMETHING YOU HAVE READ IN GoVeganWay.com BEFORE CONSULTING LICENCED MEDICAL PRACTITIONER.
In the event of a medical emergency, call a doctor or 911 immediately. GoVeganWay.com does not recommend or endorse any specific groups, organizations, tests, physicians, products, procedures, opinions, or other information that may be mentioned inside.
Editor Picks –
Milos Pokimica is a doctor of natural medicine, clinical nutritionist, medical health and nutrition writer, and nutritional science advisor. Author of the book series Go Vegan? Review of Science, he also operates the natural health website GoVeganWay.com
Latest Articles –
Plant Based News
-
Jamie Oliver Highlights ‘Important Connection’ Between Tofu And Longevity
on July 6, 2025
-
This Vegan Mung Bean Scramble Looks and Tastes Just Like Eggs
on July 6, 2025
-
Vegan Black Rice And Peas
on July 6, 2025
-
Vegan Cheese Brand Miyoko’s Introduces Taco Blend ‘Shreds’
on July 5, 2025
-
Comforting Curried Veggies
on July 5, 2025
-
10 Vegan Summer Breakfast Ideas
on July 5, 2025
-
New Netflix Documentary Highlights Impact Of Fishing On Sharks
on July 4, 2025
Top Health News — ScienceDaily
- Cough medicine turned brain protector? Ambroxol may slow Parkinson’s dementiaon July 6, 2025
Ambroxol, long used for coughs in Europe, stabilized symptoms and brain-damage markers in Parkinson’s dementia patients over 12 months, whereas placebo patients worsened. Those with high-risk genes even saw cognitive gains, hinting at real disease-modifying power.
- Multisensory VR forest reboots your brain and lifts mood—study confirmson July 6, 2025
Immersing stressed volunteers in a 360° virtual Douglas-fir forest complete with sights, sounds and scents boosted their mood, sharpened short-term memory and deepened their feeling of nature-connectedness—especially when all three senses were engaged. Researchers suggest such multisensory VR “forest baths” could brighten clinics, waiting rooms and dense city spaces, offering a potent mental refresh where real greenery is scarce.
- Pregnancy’s 100-million-year secret: Inside the placenta’s evolutionary power playon July 6, 2025
A group of scientists studying pregnancy across six different mammals—from humans to marsupials—uncovered how certain cells at the mother-baby boundary have been working together for over 100 million years. By mapping gene activity in these cells, they found that pregnancy isn’t just a battle between mother and fetus, but often a carefully coordinated partnership. These ancient cell interactions, including hormone production and nutrient sharing, evolved to support longer, more complex […]
- New tech tracks blood sodium without a single needleon July 6, 2025
Scientists have pioneered a new way to monitor sodium levels in the blood—without drawing a single drop. By combining terahertz radiation and optoacoustic detection, they created a non-invasive system that tracks sodium in real time, even through skin. The approach bypasses traditional barriers like water interference and opens up potential for fast, safe diagnostics in humans.
- Scientists reverse Parkinson’s symptoms in mice — Could humans be next?on July 6, 2025
Scientists at the University of Sydney have uncovered a malfunctioning version of the SOD1 protein that clumps inside brain cells and fuels Parkinson’s disease. In mouse models, restoring the protein’s function with a targeted copper supplement dramatically rescued movement, hinting at a future therapy that could slow or halt the disease in people.
- Tiny twitches, big breakthrough: New clues to catch Parkinson’s sooneron July 6, 2025
These findings highlight the significance of rearing behavior and behavioral lateralization as potential behavioral markers for tracking the progression of Parkinson’s disease.
- The surprising link between hearing loss, loneliness, and lifespanon July 5, 2025
People who treat hearing loss with hearing aids or cochlear implants regain rich conversations, escape isolation, and may even protect their brains and lifespans—proof that better hearing translates into fuller living.
PubMed, #vegan-diet –
- Health and environmental impacts of shifting to plant-based analogues: a risk-benefit assessmenton July 5, 2025
CONCLUSION: PBAs can be considered feasible alternatives to animal-based foods, and the results emphasise meat substitution as a crucial factor for health and environmental benefits.
- Exploring the role of gut microbiota in rheumatoid arthritis: the effects of diet and drug supplementationon July 2, 2025
Rheumatoid Arthritis (RA) is a chronic autoimmune disease that mostly breaks out at the joints. It further causes bone erosion and decreased life quality due to severe pain. Current drugs are mainly focused on reducing pain, but unable to terminate the disease progression. This study aims to determine the effect of diet types (Western, Vegan and Mediterranean) on RA progression. Some dietary supplements and drug administration (Huayu-Qiangshen-Tongbi formula or Leflunomide plus Methotrexate) […]
- Blood biomarkers of Alzheimer’s disease in Australians habitually consuming various plant-based dietson June 30, 2025
BackgroundEvidence suggests that plant-based diets (PBDs) may be protective against neurodegenerative diseases such as Alzheimer’s disease (AD).ObjectiveThis study examined associations between blood-based AD biomarkers in individuals 30-75 years without current or diagnosed cardiovascular disease following different PBDs versus regular meat-eating diets (RMEs).MethodsThis secondary analysis of the Plant-based Diets study measured Aβ(1-42)/Aβ(1-40), p-tau181, NFL, and GFAP in 237 plasma […]
- Zinc supplementation among zinc-deficient vegetarians and vegans restores antiviral interferon-α response by upregulating interferon regulatory factor 3on June 28, 2025
CONCLUSION: We identified zinc-dependent IRF3 expression as an essential cellular mechanism behind impaired IFNα response in zinc-deficient subjects. This may contribute to disturbed antiviral immunity and cause increased susceptibility to virus infections in vivo. Oral zinc supplementation effectively restored IRF3 and IFNα levels. Hence, nutritional interventions may become increasingly important in order to prevent health implications from micronutrient deficiencies among vegetarians and…
- Integrating comparative genomics and risk classification by assessing virulence, antimicrobial resistance, and plasmid spread in microbial communities with gSpreadCompon June 26, 2025
CONCLUSIONS: The gSpreadComp workflow aims to facilitate hypothesis generation for targeted experimental validations by the identification of concerning resistant hotspots in complex microbial datasets. Our study raises attention to a more thorough study of the critical role of diet in microbial community dynamics and the spread of AMR. This research underscores the importance of integrating genomic data into public health strategies to combat AMR. The gSpreadComp workflow is available at…
Random Posts –
Featured Posts –

Latest from PubMed, #plant-based diet –
- Diet in Pregnancy: A Review of Current Challenges and Recommendations. A British Nutrition Foundation Briefing Paperby Kathryn H Hart on July 6, 2025
Pregnancy is a crucial period during which maternal nutrition, weight and lifestyle behaviours have a direct impact on both maternal and fetal health. This briefing paper describes dietary and lifestyle recommendations for women during the preconceptional period and throughout pregnancy, identifying specific factors that can be modified to improve health outcomes for both mother and child. It considers key areas such as nutrient intakes, supplementation, food safety and weight management, and…
- Health and environmental impacts of shifting to plant-based analogues: a risk-benefit assessmentby Catarina Carvalho on July 5, 2025
CONCLUSION: PBAs can be considered feasible alternatives to animal-based foods, and the results emphasise meat substitution as a crucial factor for health and environmental benefits.
- Low-Carbohydrate Diet Patterns That Favor High-Quality Carbohydrates Are Associated with Beneficial Long-Term Changes in Biomarkers of Inflammation and Oxidative Stress in the Framingham Offspring…by Ghaida F Aloraini on July 4, 2025
CONCLUSIONS: LCD patterns that preserved high-quality carbohydrates while replacing low-quality carbohydrates sources, such as refined grains and added sugars, with fat and protein were inversely associated with inflammation and oxidative stress score, potentially lowering chronic disease risk.
- Linking the Planetary Health Diet Index to sarcopenia: the mediating effect of the non-high-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio (NHHR)by Huan Chen on July 4, 2025
CONCLUSION: This study highlights the observed negative correlation between PHDI and sarcopenia, with NHHR acting as a partial mediator. These findings emphasize the potential importance of dietary patterns in strategies aimed at preventing sarcopenia.
- Design and conduct of a full diet-controlled, parallel, 2-week residential trial for diabetes prevention without weight loss in Asian Chinese and European Caucasian adults with prediabetes: the New…by Ivana R Sequeira-Bisson on July 4, 2025
BACKGROUND: The causal underpinning of increased metabolic risk and previously observed dichotomous plasma metabolome in Asian Chinese vs. European Caucasian remains undetermined and may be hypothesised as attributed to ethnicity (genetic background), pathology (dysglycaemia) and/or lifestyle (habitual diet). We aimed to investigate the underlying cause(s) and the effect of dietary intervention on biomarkers of type 2 diabetes (T2D) in cohorts with prediabetes. The diets are a generic current…
- Comparison of digestive capacity in broilers raised on diets with or without soybean mealby Xiaomeng Ye on July 4, 2025
The objective of this study was to investigate the digestive capacity of broilers raised on diets with or without soybean meal, and evaluate the impact on the determination of metabolizable energy (ME) in feed. Two hundred and eighty-eight 7-day-old Arbor Acres male broilers were divided into 6 blocks based on initial body weight (BW). Within each block, 48 broilers were randomly assigned to one of the two types of diet: a corn-soybean meal diet (CSMD) and a corn-based soybean meal-free diet…