Binge Eating and Hormonal Regulation: Emotional Hunger
Our entire evolution, we were like any other species on this planet, in constant hunger and in search of food. Overeating is an example of maladaptation.
Milos Pokimica
Written By: Milos Pokimica
Medically Reviewed by: Dr. Xiùying Wáng, M.D.
Updated June 9, 2023For our entire evolution, we were like any other species on this planet in constant search of food. We were not obese but in a state of constant hunger and constant physical activity. This was the case for all of our ancestor species and that means the time period of 50 million years.
Technological progress that happened in the last couple of hundreds of years didn’t change our body physiology. It is an abrupt shift in evolutional terms. The feeling of constant fullness, on the other hand, is not natural, and it is an example of maladaptation. Our hominin ancestors and even homo sapiens dint have technology and food on every corner. Hunger is a normal feeling and it is a normal feeling for every animal. Because of our evolutionary conditioning and the way our brain works, people even if we are on a restrictive diet cannot deal with the feeling of constant hunger. We want to have a feeling of fullness and there is nothing we can do about it. So here comes caffeine, hunger suppressors of different kinds and medicine and surgeries, and so on.
In an evolutionary sense, this is protective behavior, because there is an extreme scarcity of food, bingeing as much as we possibly can is a good survival strategy. But what happens when we have an overabundance of food and we never had that abundance during our entire existence including our direct ancestor species. Our evolution didn’t begin with the modern human species we have just become a little smarter. Most of our genes and the body are the same, especially in basic survival mechanisms that didn’t have to change for millions of years.
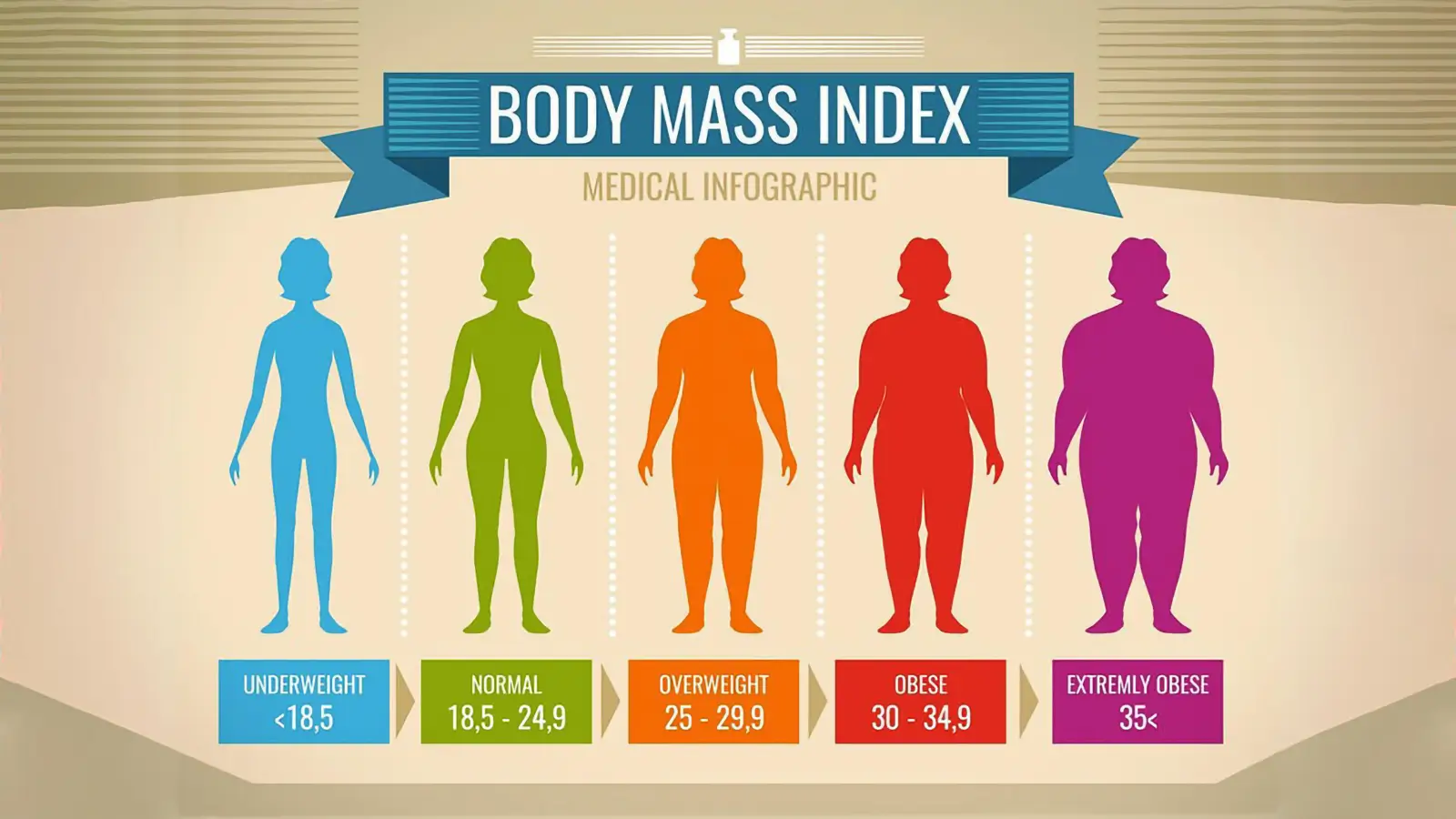
All of this would not have to be an issue but obesity is everything but a cosmetic issue. Most people do understand this but are unable to do anything about it because of fear of starvation. This fear is instinctive and it would override any logical behavior and in reality, we would always overeat. Weight gain comes slowly and in a prolonged period. Even if we gain just a little on a monthly basis, in time this little would be too much.
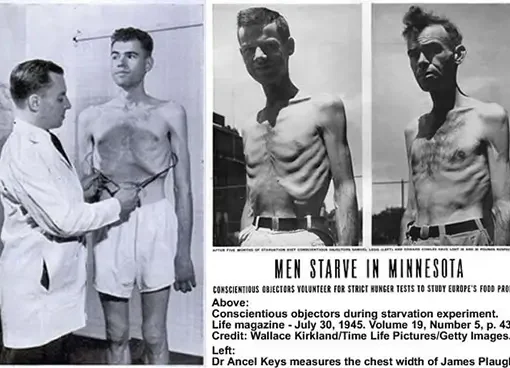
When an individual starts to have a restrictive diet the instinctive fear of starvation will have an impact on behavior and more than just in the psychological way. It will trigger different pathways in the brain that are responsible for appetite control, fear, reward mechanism (how much pleasure we get from pleasurable experiences), and most of our brain functioning. And this will not stop when we go off the diet but will continue as a never-ending story. It is a so-called “yo-yo” effect. Even since a Minnesota starvation experiment (Kelesidis et al., 2010) scientists have been aware of the full scope of effects that a restrictive diet can have on someone’s behavior.
The way that the brain works is by the “carrot and a stick” mechanism. Number one would be the avoidance of pain, and when pain is avoided pleasure-seeking comes into play.
The more pain the stronger behavioral changes. The problem is until the pain is removed the pleasure-seeking does not exist. For example, people in the Minnesota starvation experiment after a period of time couldn’t think of anything else except food. They could not take the pain of constant hunger. After they were given food the fear of starvation never went away and they were overeating and binging as much as they could and have become obese in a very short period. But this behavior exists just to a smaller extent in everyday “normal” behavior. The most normal feeling of hunger had become much more pronounced because today we cannot deal with hunger because we have never experienced the real level of starvation. That is the reason why most of us cannot really cope well with dieting because we do not have tolerance for pain anymore. And even if we do, the normal response of the brain will be to go into survival avoidance of pain mode and cut off all pleasure-seeking behavior until the hunger is removed. It is not possible to be in a state of hunger and enjoy life. Especially because now we are removed from our natural environment and we have supernormal stimuli everywhere. Even a normal feeling of hunger is something that we cannot take as a normal feeling anymore.
Our behavior has been conditioned in such a way that our brain has down-regulated its pleasure response. For example, this happens to heroin addicts. Heroin is one of the strongest drugs in existence. It gives a lot of pleasure. But in time addicts will become more tolerant of the effects of it to some extent because their brain adapts. The same thing has happened in our modern society. Our brain has to some extent adapted to supernormal stimuli from food and hunger has become a much more pronounced feeling than it would be in normal animal species. Because of lack of scarcity food is not as a big reward as it used to be especially because of unnaturally high concentrations and combinations of energy sources that do not exist in nature.
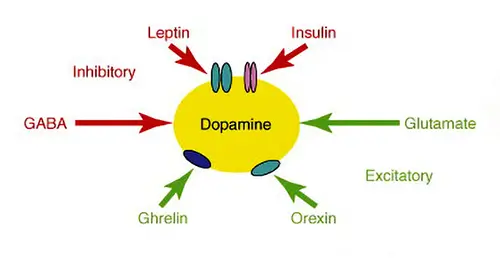
Extracted sugar and extracted fat do not exist in nature and it is digested much quicker than in normal circumstances from whole food sources giving us a dopamine high. Especially the combination of sugar and fat (Zhang et al., 2005). This combination does not exist in nature. Because of this dieting has become a form of addiction much more than it would be in a natural environment.
The result of this is that we have become obese and there is nothing we can do about it. Today nearly 70% of American adults are either overweight or obese.
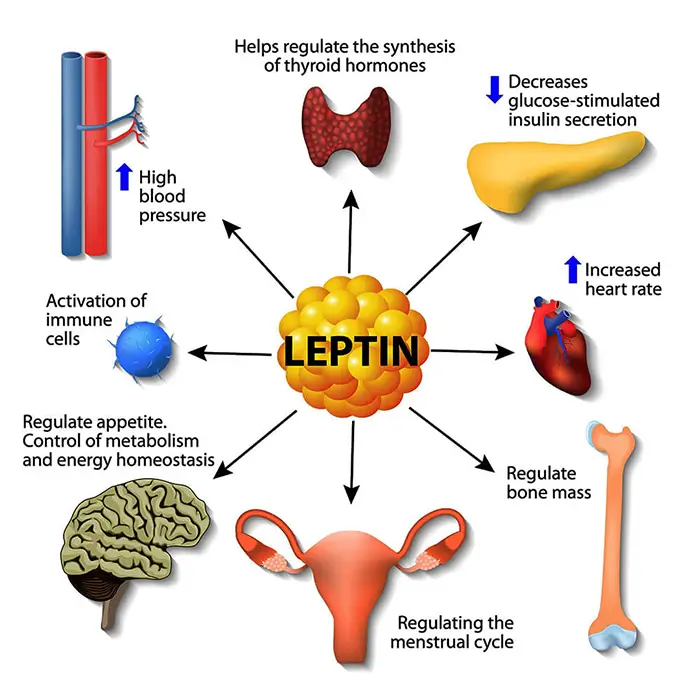
Actually, even anorexia nervosa patients are victims of the same maladaptation. It is not a psychological issue it is conditioned behavior of pleasure and pain reward mechanisms. In anorexia patients, there is also malfunction but in the opposite direction. When they refeed themselves, their plasma leptin concentration will increase rapidly and reach roughly normal levels long before normal weight is achieved (Obradovic et al., 2021). Thus keeping them anorexic. They experience hunger much less than someone that does not have this condition. Excessive leptin production and its effect on the feeling of fullness could play a permissive role in the pathogenesis of this condition.
Leptin is the satiety hormone, and it is opposed by the actions of another hormone named ghrelin, the hunger hormone. Both hormones act on the receptors in the brain to regulate appetite (Zhang et al., 2017). When people think that their conscious mind will have an impact on their behavior I always asked them to do an experiment and try to keep their breath. After a minute or so there will be pain singling and the unconscious part of the brain will override our behavior. The signal is due to the fact that the brain is dying and no matter what, you have to take oxygen in or die. We will gasp for breath no matter how strongly we resist. This is a reason that someone can drown in 20 seconds if panic kicks in. The same behavior changes affect our day-to-day behavior in regard to the water we drink, the air we breathe and the food we eat.
The balance of these two hormones is necessary to achieve an overall energy balance in the body. In obesity, a decreased sensitivity to leptin occurs (Anderberg et al., 2016). This is a big problem that will result in a brain’s inability to detect satiety despite high energy stores in the rest of the body. Why does this happen? The basis for leptin resistance in obese human subjects is unknown. If leptin levels remain persistently raised due to overeating, there may be a downregulation of the leptin receptors and hence decreased sensitivity to the hormone. In humans, and actually in any other animal low leptin levels induced by a low-calorie diet resulted in a decrease in plasma leptin concentration triggering high levels of constant hunger. This may explain the high failure rate of dieting. Low leptin levels are likely to be a powerful stimulus to weight gain.
In the case of obesity, the standard regulatory system will tell the brain that we have fat deposits stored for an extended period and that we can endure little hunger. The problem is that we could never become fat due to scarcity, so we never developed an adaptation to the abundance of food. Our mind still thinks that if we do not eat all that we can we will starve to death in the upcoming drought.
References:
- Kelesidis, T., Kelesidis, I., Chou, S., & Mantzoros, C. S. (2010). Narrative review: the role of leptin in human physiology: emerging clinical applications. Annals of internal medicine, 152(2), 93–100. https://doi.org/10.7326/0003-4819-152-2-201001190-00008
- Zhang, F., Chen, Y., Heiman, M., & Dimarchi, R. (2005). Leptin: structure, function and biology. Vitamins and hormones, 71, 345–372. https://doi.org/10.1016/S0083-6729(05)71012-8
- Obradovic, M., Sudar-Milovanovic, E., Soskic, S., Essack, M., Arya, S., Stewart, A. J., Gojobori, T., & Isenovic, E. R. (2021). Leptin and Obesity: Role and Clinical Implication. Frontiers in endocrinology, 12, 585887. https://doi.org/10.3389/fendo.2021.585887
- Zhang, Y., & Chua, S., Jr (2017). Leptin Function and Regulation. Comprehensive Physiology, 8(1), 351–369. https://doi.org/10.1002/cphy.c160041
- Anderberg, R. H., Hansson, C., Fenander, M., Richard, J. E., Dickson, S. L., Nissbrandt, H., Bergquist, F., & Skibicka, K. P. (2016). The Stomach-Derived Hormone Ghrelin Increases Impulsive Behavior. Neuropsychopharmacology : official publication of the American College of Neuropsychopharmacology, 41(5), 1199–1209. https://doi.org/10.1038/npp.2015.297
- Kalm, L. M., & Semba, R. D. (2005). They starved so that others be better fed: remembering Ancel Keys and the Minnesota experiment. The Journal of nutrition, 135(6), 1347–1352. https://doi.org/10.1093/jn/135.6.1347
- Tobey J. A. (1951). The Biology of Human Starvation. American Journal of Public Health and the Nations Health, 41(2), 236–237.[PubMed]
- Howick, K., Griffin, B. T., Cryan, J. F., & Schellekens, H. (2017). From Belly to Brain: Targeting the Ghrelin Receptor in Appetite and Food Intake Regulation. International journal of molecular sciences, 18(2), 273. https://doi.org/10.3390/ijms18020273
- Müller, M. J., Enderle, J., Pourhassan, M., Braun, W., Eggeling, B., Lagerpusch, M., Glüer, C. C., Kehayias, J. J., Kiosz, D., & Bosy-Westphal, A. (2015). Metabolic adaptation to caloric restriction and subsequent refeeding: the Minnesota Starvation Experiment revisited. The American journal of clinical nutrition, 102(4), 807–819. https://doi.org/10.3945/ajcn.115.109173
- Dulloo A. G. (2021). Physiology of weight regain: Lessons from the classic Minnesota Starvation Experiment on human body composition regulation. Obesity reviews : an official journal of the International Association for the Study of Obesity, 22 Suppl 2, e13189. https://doi.org/10.1111/obr.13189
- LASKER G. W. (1947). The effects of partial starvation on somatotype: an analysis of material from the Minnesota starving experiment. American journal of physical anthropology, 5(3), 323–341. https://doi.org/10.1002/ajpa.1330050305
- Dulloo, A. G., Jacquet, J., & Girardier, L. (1996). Autoregulation of body composition during weight recovery in human: the Minnesota Experiment revisited. International journal of obesity and related metabolic disorders : journal of the International Association for the Study of Obesity, 20(5), 393–405.[PubMed]
- Keys et al. (1950) “The Biology of Human Starvation (2 volumes)”. University of Minnesota Press.
Related Posts
Sources:
Do you have any questions about nutrition and health?
I would love to hear from you and answer them in my next post. I appreciate your input and opinion and I look forward to hearing from you soon. I also invite you to follow us on Facebook, Instagram, and Pinterest for more diet, nutrition, and health content. You can leave a comment there and connect with other health enthusiasts, share your tips and experiences, and get support and encouragement from our team and community.
I hope that this post was informative and enjoyable for you and that you are prepared to apply the insights you learned. If you found this post helpful, please share it with your friends and family who might also benefit from it. You never know who might need some guidance and support on their health journey.
– You Might Also Like –

Learn About Nutrition
Milos Pokimica is a doctor of natural medicine, clinical nutritionist, medical health and nutrition writer, and nutritional science advisor. Author of the book series Go Vegan? Review of Science, he also operates the natural health website GoVeganWay.com
Medical Disclaimer
GoVeganWay.com brings you reviews of the latest nutrition and health-related research. The information provided represents the personal opinion of the author and is not intended nor implied to be a substitute for professional medical advice, diagnosis, or treatment. The information provided is for informational purposes only and is not intended to serve as a substitute for the consultation, diagnosis, and/or medical treatment of a qualified physician or healthcare provider.NEVER DISREGARD PROFESSIONAL MEDICAL ADVICE OR DELAY SEEKING MEDICAL TREATMENT BECAUSE OF SOMETHING YOU HAVE READ ON OR ACCESSED THROUGH GoVeganWay.com
NEVER APPLY ANY LIFESTYLE CHANGES OR ANY CHANGES AT ALL AS A CONSEQUENCE OF SOMETHING YOU HAVE READ IN GoVeganWay.com BEFORE CONSULTING LICENCED MEDICAL PRACTITIONER.
In the event of a medical emergency, call a doctor or 911 immediately. GoVeganWay.com does not recommend or endorse any specific groups, organizations, tests, physicians, products, procedures, opinions, or other information that may be mentioned inside.
Editor Picks –
Milos Pokimica is a health and nutrition writer and nutritional science advisor. Author of the book series Go Vegan? Review of Science, he also operates the natural health website GoVeganWay.com
Latest Articles –
Top Health News — ScienceDaily
- The overlooked nutrition risk of Ozempic and Wegovyon February 4, 2026
Popular weight-loss drugs like Ozempic and Wegovy can dramatically curb appetite, but experts warn many users are flying blind when it comes to nutrition. New research suggests people taking these medications may not be getting enough guidance on protein, vitamins, and overall diet quality, increasing the risk of muscle loss and nutrient deficiencies.
- A 25-year study found an unexpected link between cheese and dementiaon February 4, 2026
A massive Swedish study tracking nearly 28,000 people for 25 years found an unexpected link between full-fat dairy and brain health. Among adults without a genetic risk for Alzheimer’s, eating more full-fat cheese was associated with a noticeably lower risk of developing the disease, while higher cream intake was tied to reduced dementia risk overall. The findings challenge decades of low-fat dietary advice but come with important caveats.
- MIT’s new brain tool could finally explain consciousnesson February 4, 2026
Scientists still don’t know how the brain turns physical activity into thoughts, feelings, and awareness—but a powerful new tool may help crack the mystery. Researchers at MIT are exploring transcranial focused ultrasound, a noninvasive technology that can precisely stimulate deep regions of the brain that were previously off-limits. In a new “roadmap” paper, they explain how this method could finally let scientists test cause-and-effect in consciousness research, not just observe […]
- Why heart disease risk in type 2 diabetes looks different for men and womenon February 4, 2026
Scientists are digging into why heart disease risk in type 2 diabetes differs between men and women—and sex hormones may be part of the story. In a large Johns Hopkins study, men with higher testosterone had lower heart disease risk, while rising estradiol levels were linked to higher risk. These hormone effects were not seen in women. The results point toward more personalized approaches to heart disease prevention in diabetes.
- Sound machines might be making your sleep worseon February 4, 2026
Sound machines may not be the sleep saviors many believe. Researchers found that pink noise significantly reduced REM sleep, while simple earplugs did a better job protecting deep, restorative sleep from traffic noise. When pink noise was combined with outside noise, sleep quality dropped even further. The results suggest that popular “sleep sounds” could be doing more harm than good—particularly for kids.
- This unexpected plant discovery could change how drugs are madeon February 3, 2026
Plants make chemical weapons to protect themselves, and many of these compounds have become vital to human medicine. Researchers found that one powerful plant chemical is produced using a gene that looks surprisingly bacterial. This suggests plants reuse microbial tools to invent new chemistry. The insight could help scientists discover new drugs and produce them more sustainably.
- A hidden cellular process may drive aging and diseaseon February 3, 2026
As we age, our cells don’t just wear down—they reorganize. Researchers found that cells actively remodel a key structure called the endoplasmic reticulum, reducing protein-producing regions while preserving fat-related ones. This process, driven by ER-phagy, is tied to lifespan and healthy aging. Because these changes happen early, they could help trigger later disease—or offer a chance to stop it.
PubMed, #vegan-diet –
- Diet type and the oral microbiomeon February 2, 2026
CONCLUSION: The diet-oral microbiome-systemic inflammation axis is bidirectional and clinically relevant. Understanding both direct ecological regulation and indirect metabolic effects is essential to support precision nutrition strategies aimed at maintaining oral microbial balance and systemic inflammatory risk mitigation.
- Consensus document on healthy lifestyleson January 22, 2026
Proteins are a group of macronutrients that are vital to our lives, as they perform various functions, including structural, defensive and catalytic. An intake of 1.0-1.2 g/kg/body weight per day would be sufficient to meet our needs. Carbohydrate requirements constitute 50 % of the total caloric value and should be obtained mainly in the form of complex carbohydrates. In addition, a daily intake of both soluble and insoluble fiber is necessary. Regular consumption of extra virgin olive oil […]
- Vitamin B12 and D status in long-term vegetarians: Impact of diet duration and subtypes in Beijing, Chinaon January 21, 2026
CONCLUSIONS: This study reveals a dual challenge among Beijing long-term vegetarians: vitamin B12 deficiency was strongly associated with the degree of exclusion of animal products from the diet (veganism), while vitamin D deficiency was highly prevalent and worsened with longer diet duration. The near-universal vitamin D deficiency observed in this study suggests that, in the Beijing context, the risk may extend beyond dietary choice, potentially reflecting regional environmental factors;…
- Nutritional evaluation of duty meals provided to riot police forces in Germanyon January 13, 2026
Background: The primary role of the German riot police is maintaining internal security. Due to challenging working conditions, riot police forces face an elevated risk of various diseases. During duty, forces are provided with meals. A balanced diet can reduce the risk of some of these diseases and contribute to health-promoting working conditions. Aim: First evaluation of the nutritional quality of duty meals in Germany based on German Nutrition Society recommendations (DGE). Methods: In…
- Iodineon January 1, 2006
Iodine is an essential trace nutrient for all infants that is a normal component of breastmilk. Infant requirements are estimated to be 15 mcg/kg daily in full-term infants and 30 mcg/kg daily in preterm infants.[1] Breastmilk iodine concentration correlates well with maternal urinary iodine concentration and may be a useful index of iodine sufficiency in infants under 2 years of age, but there is no clear agreement on a value that indicates iodine sufficiency, and may not correlate with […]
Random Posts –
Featured Posts –
Latest from PubMed, #plant-based diet –
- From paddy soil to dining table: biological biofortification of rice with zincby Lei Huang on February 4, 2026
One-third of paddy soils are globally deficient in zinc (Zn) and 40% of Zn loss in the procession from brown rice to polished rice, which results in the global issue of hidden hunger, e.g., the micronutrient deficiencies in the rice-based population of developing countries. In the recent decades, biofortification of cereal food crops with Zn has emerged as a promising solution. Herein, we comprehensively reviewed the entire process of Zn in paddy soil to human diet, including the regulatory…
- Molecular Characterization of Tobacco Necrosis Virus A Variants Identified in Sugarbeet Rootsby Alyssa Flobinus on February 3, 2026
Sugarbeet provides an important source of sucrose; a stable, environmentally safe, and low-cost staple in the human diet. Viral diseases arising in sugarbeet ultimately impact sugar content, which translates to financial losses for growers. To manage diseases and prevent such losses from occurring, it is essential to characterize viruses responsible for disease. Recently, our laboratory identified a tobacco necrosis virus A variant named Beta vulgaris alphanecrovirus 1 (BvANV-1) in sugarbeet…
- Nutrition in early life interacts with genetic risk to influence preadult behaviour in the Raine Studyby Lars Meinertz Byg on February 3, 2026
CONCLUSIONS: Nutrition in early life and psychiatric genetic risk may interact to determine lasting child behaviour. Contrary to our hypothesis, we find dietary benefits in individuals with lower ADHD PGS, necessitating replication. We also highlight the possibility of including genetics in early nutrition intervention trials for causal inference.
- Effect of the gut microbiota on insect reproduction: mechanisms and biotechnological prospectsby Dilawar Abbas on February 2, 2026
The insect gut microbiota functions as a multifunctional symbiotic system that plays a central role in host reproduction. Through the production of bioactive metabolites, gut microbes interact with host hormonal pathways, immune signaling, and molecular regulatory networks, thereby shaping reproductive physiology and fitness. This review summarizes recent advances in understanding how gut microbiota regulate insect reproduction. Accumulating evidence demonstrates that microbial metabolites…
- Rationale and design of a parallel randomised trial of a plant-based intensive lifestyle intervention for diabetes remission: The REmission of diabetes using a PlAnt-based weight loss InteRvention…by Brighid McKay on February 2, 2026
CONCLUSIONS: This trial will provide high-quality clinical evidence on the use of plant-based ILIs to address the epidemics of obesity and diabetes to inform public health policies and programs in Canada and beyond.
- Diet type and the oral microbiomeby Daniel Betancur on February 2, 2026
CONCLUSION: The diet-oral microbiome-systemic inflammation axis is bidirectional and clinically relevant. Understanding both direct ecological regulation and indirect metabolic effects is essential to support precision nutrition strategies aimed at maintaining oral microbial balance and systemic inflammatory risk mitigation.