Sweets Teeth Sensitivity & Pain: Quick Fix & Lasting Solution
A quick and easy fix for pain relief is clove essential oil, a powerful antioxidant and pain reliever that can help with gum disease and toothache.
Milos Pokimica
Written By: Milos Pokimica
Medically Reviewed by: Dr. Xiùying Wáng, M.D.
Updated October 7, 2023Key Takeaways:
– Teeth sensitivity (DHS) is a condition where the dentin, the layer of tissue under the enamel that covers the tooth, becomes exposed and sensitive to external stimuli.
– Sometimes the enamel can wear away or get damaged by factors such as tooth decay, erosion, abrasion, or trauma. This can expose the dentin and the dentinal tubules to the oral environment.
– There are two main types of dentistry treatments for DHS: desensitizing agents and physical barriers (Liu et al., 2020).
– These treatments are not natural and do not remove the root cause of the problem which is in most cases demineralization of the teeth, gum disease, or plaque buildup with dental caries.
– Tooth mineralization is the process of restoring the minerals that are lost from the enamel, the outermost layer of the tooth, due to various factors such as bacteria, acid, and saliva.
– Tooth remineralization can be influenced by minerals such as magnesium, zinc, and copper, which have various roles in enamel formation and function (Zamojda et al., 2023).
– Trace minerals are present in the enamel and can affect its formation and structure.
– Bacteria form a sticky layer on teeth called dental plaque or biofilm, where they feed on the sugars and starches from food and drinks. As they do so, they produce acids that erode the enamel.
– These acids dissolve the minerals from dental tissues, creating tiny holes or cavities in the teeth (Metwalli et al., 2013). This condition is called dental caries, and it can lead to DHS, toothache, infection, and tooth loss.
– The main culprit for causing cavities in the supragingival plaque (the sticky film that forms on the surface of your teeth above the gum line) is a bacterium called Streptococcus mutans, along with other streptococci such as S. sanguinis, S. mitis, and S. salivarius (Forssten et al., 2010).
– Candida albicans can also form biofilms on your teeth, and it seems that they have a symbiotic relationship with Streptococcus mutans (Metwalli et al., 2013).
– One of the steps for treating tooth sensitivity is the removal of the plaque, healing of the oral thrush or candida overgrowth in the mouth, and keeping the Streptococcus mutans in low numbers.
– Gram-negative anaerobic bacteria such as Fusobacterium nucleatum, Porphyromonas gingivalis, and Prevotella intermedia, are mostly found in the subgingival plaque, the plaque that builds up below the gum line (Jørn et al., 2005).
– These bacteria produce toxins that harm the gum tissue and bone that hold your teeth in place, resulting in symptoms such as bleeding, swelling, pain, and eventually tooth loss.
– Eating a severely pro-inflammatory diet filled with environmental toxicity, that has low levels of antioxidant-rich foods and with a nonexistent ORAC score would lead to chronic inflammation especially if you have other bad habits like drinking, smoking, abusing substances, and overeating on meat and junk food.
– Before a Lidocaine or Novocaine injection, dentists swab your gums with clove oil for 5 minutes for some preliminary anesthetic action before administrating anesthetic injections.
– The eugenol from clove oil works like other local anesthetics, by temporarily blocking the nerves that carry the pain signal to your brain (Taleuzzaman et al., 2021).
– The homemade natural mouthwash presented in this article is very potent and can help you with gum disease and toothache. It can also boost your antioxidant levels and improve your overall health.
Teeth Sensitivity to Sugar or Cold.
If you have ever experienced a sharp pain in your teeth when you drink something cold, hot, sweet, or sour, you may have dentin hypersensitivity (DHS). Sweets teeth pain or in general dentin hypersensitivity is a common dental problem that affects many people, but it can also be very frustrating and confusing.
How do you know if you have DHS or something else? How do you treat it and prevent it from getting worse? What causes it in the first place?
Teeth sensitivity (DHS) is a condition where the dentin, the layer of tissue under the enamel that covers the tooth, becomes exposed and sensitive to external stimuli.
Your teeth are made up of three layers: the enamel, the dentin, and the pulp. The enamel is the hard outer layer that protects your teeth from wear and tear. The dentin is the softer layer underneath the enamel that contains tiny tubes called dentinal tubules. These tubules connect the enamel to the pulp, which is the innermost layer that contains nerves and blood vessels.
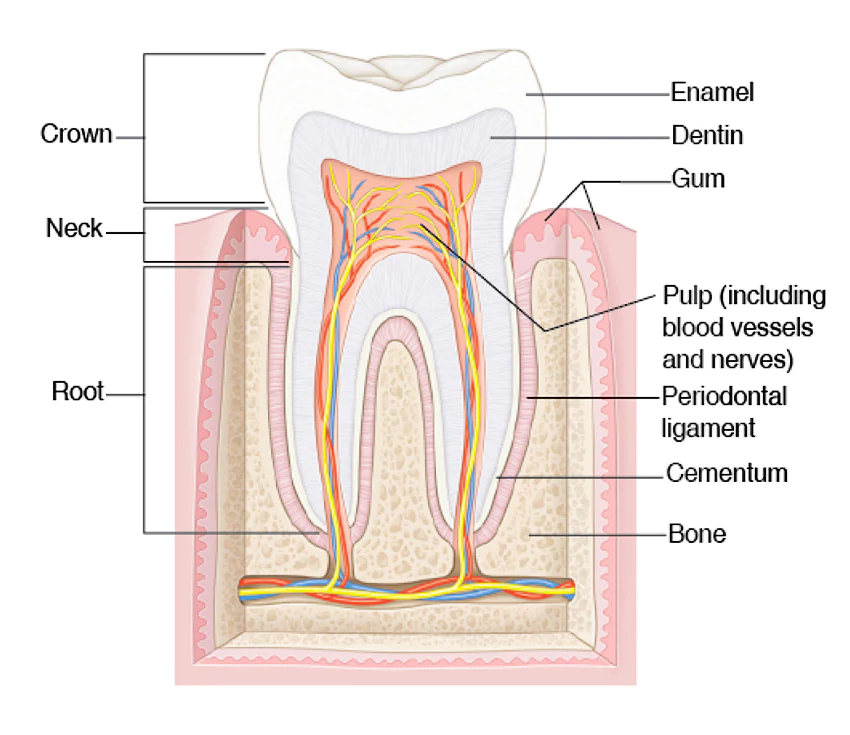
Normally, the enamel covers and seals the dentin, preventing any stimuli from reaching the pulp.
However, sometimes the enamel can wear away or get damaged by factors such as tooth decay, erosion, abrasion, or trauma. This can expose the dentin and the dentinal tubules to the oral environment.
When this happens, any changes in temperature, pressure, or chemical composition in your mouth can cause fluid movements within the dentinal tubules. These fluid movements can stimulate the nerves in the pulp and cause pain. This is called the hydrodynamic theory, and it is the most widely accepted explanation for DHS pain (Liu et al., 2020).
However, DHS pain is not just a matter of exposed dentin and fluid movements. Other factors can influence how your teeth react to stimuli.
For example, some people may have more sensitive nerves than others due to genetic variations or inflammation. Some people may also have more open or wider dentinal tubules than others due to aging or disease. These factors can make some people more prone to DHS than others.
Pain is Not Always a Sensitivity.
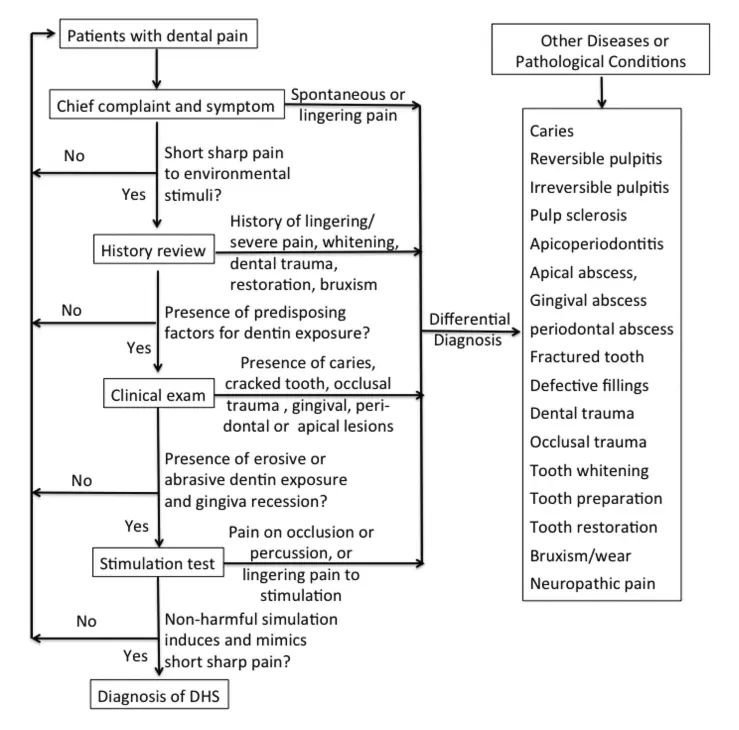
DHS can also be confused with other dental conditions that have similar symptoms.
For example, dental caries (cavities), cracked teeth, pulpitis (inflammation of the pulp), or root canal infections can also cause tooth sensitivity and pain (Liu et al., 2020).
These conditions may require different treatments than DHS, such as fillings, crowns, or root canal therapy. Therefore, it is important to distinguish DHS from other possible causes of tooth pain.
Initiating factors are the ones that trigger the exposure of your dentin and the onset of pain. They include (Liu et al., 2020):
- Tooth decay: Cavities can eat away your enamel and dentin and create holes or gaps in your teeth.
- Tooth wear: Abrasion (from brushing too hard), erosion (from acid attack), attrition (from grinding or clenching), or abfraction (from bending or flexing) can wear away your enamel and dentin and create grooves or notches in your teeth.
- Tooth fracture: Cracks or chips can break your enamel and dentin and create sharp edges or corners in your teeth.
- Gum recession: Your gums can shrink back from your teeth due to aging, inflammation, infection, or brushing too hard. This can expose the roots of your teeth, which are covered by a thin layer of cementum that can easily wear away.
- Dentinal tubule exposure: Your dentin contains millions of tiny tubes called dentinal tubules that connect the enamel to the pulp (the innermost layer that contains nerves and blood vessels). When your dentin is exposed, these tubules become open to the oral environment.
How Can You Recognize DHS?
So how do you diagnose and treat DHS? Unfortunately, there are no universally accepted guidelines for this process. Different dentists may use different methods and criteria to identify and manage DHS. However, there are some general principles and strategies that can help you deal with this condition.
First of all, you need to visit your dentist for a thorough examination of your teeth and mouth. Your dentist will ask you about your medical and dental history, your symptoms, and your habits. They will also perform various tests to check your teeth for signs of decay, damage, or infection. They may also use special tools or devices to apply different stimuli to your teeth and see how they respond.
Based on these findings, your dentist will determine if you have DHS or another dental problem that needs treatment. If you have DHS, your dentist will recommend the best treatment option for you based on the severity of your condition and your personal preferences.
Treatment Options.
There are two main types of dentistry treatments for DHS: desensitizing agents and physical barriers (Liu et al., 2020).
Desensitizing agents are substances that reduce the sensitivity of your nerves or block the transmission of pain signals from your teeth to your brain. They can be applied directly to your teeth by your dentist or by yourself at home using toothpaste, gels, rinses, or strips. Some examples of desensitizing agents that you can get in the dental office are potassium nitrate, fluoride, strontium chloride, oxalates, glutaraldehyde, or calcium phosphate.
Physical barriers are materials that cover and seal the exposed dentin and dentinal tubules, preventing any stimuli from reaching the pulp. They can be applied by your dentist using bonding agents, composite resins, glass ionomers, or varnishes. They can also be applied by yourself at home using sealants or desensitizing chewing gums.
Both types of treatments aim to reduce or eliminate DHS pain by interfering with the hydrodynamic mechanism. However, they may not work for everyone or last forever, these treatments are not natural and do not remove the root cause of the problem which is in most cases demineralization of the teeth, gum disease, or plaque buildup with dental caries.
Some people may not respond well due to allergies or side effects. Some agents or materials may wear off over time due to saliva or brushing. Therefore, you may need to implement holistic and complete removal of the underlying cause of this issue and this would be a topic for this article.
In addition to these treatments that we would be analyzing, you also need to take good care of your oral health and prevent further damage to your enamel and dentin. You can do this by following these tips (Ramli et al., 2022):
- Brush your teeth twice a day with a soft-bristled toothbrush and fluoride toothpaste. Use gentle strokes and avoid scrubbing or brushing too hard.
- Floss your teeth once a day to remove plaque and food particles from between your teeth and gums.
- Rinse your mouth with natural mouthwash after eating or drinking acidic or sugary foods or beverages. This can help neutralize the acids and sugars that can erode your enamel and dentin.
- Avoid or limit foods and drinks that can cause tooth sensitivity, such as ice, cold or hot liquids, citrus fruits, carbonated drinks, wine, or candy. If you do consume them, use a straw or drink water afterward to minimize contact with your teeth.
- Avoid or quit smoking, as it can stain your teeth, damage your gums, and increase your risk of oral cancer.
- Visit your dentist regularly for check-ups and cleanings. Your dentist can monitor your oral health, detect any problems early, and provide professional treatments if needed.
- Reduce or avoid acidic foods and beverages.
- Avoid destructive parafunctional habits, such as tooth grinding. Tooth grinding may result in erosive tooth structure loss.
Mineral Deficiencies and Demineralization.
Minerals are the main building blocks of the enamel, the hard outer layer of the tooth that protects it from decay and sensitivity.
Enamel is not like other tissues in your body. It is not alive and it cannot grow or repair itself. It is formed during the early stages of your life when your teeth are developing inside the gums. Once teeth come out, enamel is set for life. That means that you have to take good care of it because once it is damaged, it cannot be restored.
But what makes enamel so strong and durable in the first place? The answer lies in its mineral composition. Enamel is mainly made of tiny crystals called hydroxyapatites, which are composed of calcium and phosphate. These crystals form a dense and organized structure that gives enamel its hardness and resistance.
Tooth mineralization is the process of restoring the minerals that are lost from the enamel, the outermost layer of the tooth, due to various factors such as bacteria, acid, and saliva.
When the enamel loses minerals, it becomes weaker and more prone to decay and cavities. Tooth remineralization is the natural way of repairing the enamel by depositing calcium and phosphate from the saliva back into the enamel.
Tooth remineralization can be influenced by minerals such as magnesium, zinc, and copper, which have various roles in enamel formation and function (Zamojda et al., 2023). These minerals play a vital role in enamel formation and function, and they may also influence how enamel reacts to different agents that appear in the oral cavity, such as acids, bacteria, or abrasives.
The problem is that if we have a diet consistent with empty calories like sugar, oil, and fat and produce grown on mineral-depleted soil with the use of synthetic fertilizers and on top of that do not get enough magnesium that is mostly found in green leafy vegetables our teeth might go through mineral loss and erosion of enamel.
For example, magnesium can affect the shape and size of the hydroxyapatite crystals, which affects the structure and hardness of enamel. Magnesium can also prevent the conversion of calcium phosphate from a non-crystallized form to a crystallized form, which affects the stability of enamel. Magnesium is also a part of the organic matrix of enamel, which is the scaffold that supports the mineral crystals (Klimuszko et al., 2018).
Magnesium is also one of the most common deficiencies in the standard American diet. About 57% of the US population does not meet the US RDA for dietary intake of magnesium.
Zinc is involved in the metabolism of many factors and proteins that are involved in enamel formation, such as enzymes, transcription factors, and proteases. Zinc can also protect enamel from acid attack by forming a protective layer on the enamel surface. Zinc is essential for normal enamel formation, and its deficiency can make your enamel weaker.
Copper can inhibit the formation of dental plaque, which is a sticky film of bacteria that can cause tooth decay. Copper can also reduce the acid solubility of enamel and enhance its remineralization.
Trace minerals are present in the enamel and can affect its formation and structure.
The most abundant trace elements in saliva (Na, Mg, K, and Zn) are also the most abundant trace elements in tooth enamel.
As you can see, minerals are very important for your enamel health. They help form and maintain your enamel structure and function, and they also help protect your enamel from harmful agents. That’s why you should make sure you get enough minerals from your diet or supplements or your teeth might become demineralized and sensitive leading to DHS.
To read in more detail about demineralization you can visit this article How to Stop Tooth Decay: Symptoms, Causes & Prevention.

Plague Buildup and Tooth Decay (Cavities).
Tooth decay is the result of a complex interaction between the bacteria that live in the mouth, the food we eat, the saliva, and genetic factors.
In the initial stage of tooth decay, there is initial demineralization. This is the first sign of tooth decay when the enamel begins to lose minerals due to the acids produced by plaque bacteria. A white spot may appear on the tooth, indicating early decay.
This early stage can be reversed by minerals from saliva to repair the enamel. At this stage, teeth might become sensitive to sugar and sweet or cold.
In this stage, there would be enamel decay. This is when the enamel breaks down further and forms small holes or cavities. The tooth may become darker in color or have black spots. This stage requires a filling by a dentist to restore the tooth’s structure. In this stage, bacteria have done permanent damage.
The bacteria in the mouth are not always bad. Some of them help us digest food, fight infections, and maintain a healthy balance of microorganisms. However, some of them can also cause problems for teeth and gums.
These bacteria form a sticky layer on teeth called dental plaque or biofilm, where they feed on the sugars and starches from food and drinks. As they do so, they produce acids that erode the enamel. The acids also create sticky substances called glucans that help the bacteria stick to your teeth and form more plaque.
Some areas of teeth are more prone to decay than others, such as the pits and fissures on the chewing surfaces of your back teeth. These areas are harder to clean and more likely to trap food and plaque, which can lead to more acid production and enamel breakdown. That’s why most of the cavities occur in these areas.
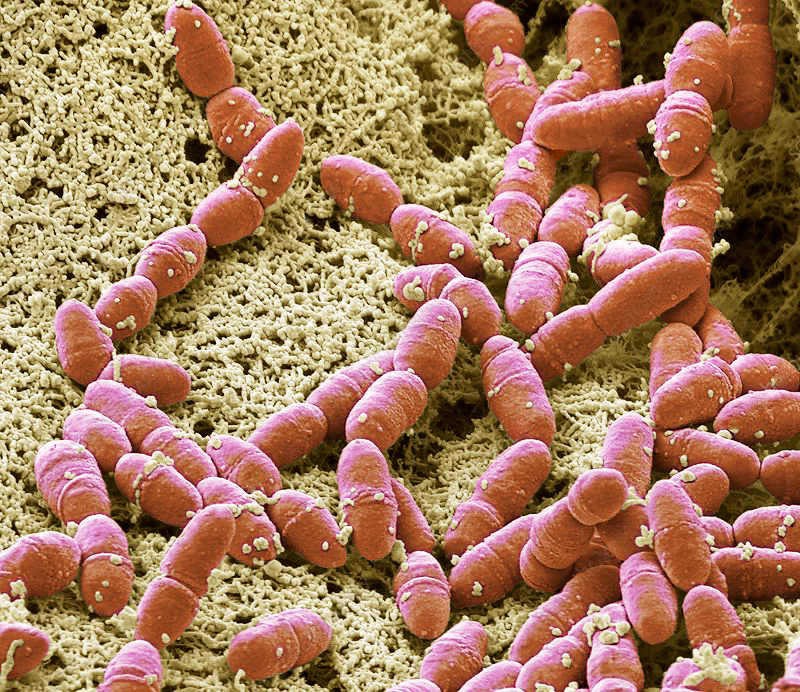
The main culprit for causing cavities in the supragingival plaque (the sticky film that forms on the surface of your teeth above the gum line) is a bacterium called Streptococcus mutans, along with other streptococci such as S. sanguinis, S. mitis, and S. salivarius (Forssten et al., 2010). These bacteria produce acids that erode the enamel of your teeth and create holes or cavities. Other bacteria that contribute to tooth decay include lactobacilli and Veillonella.
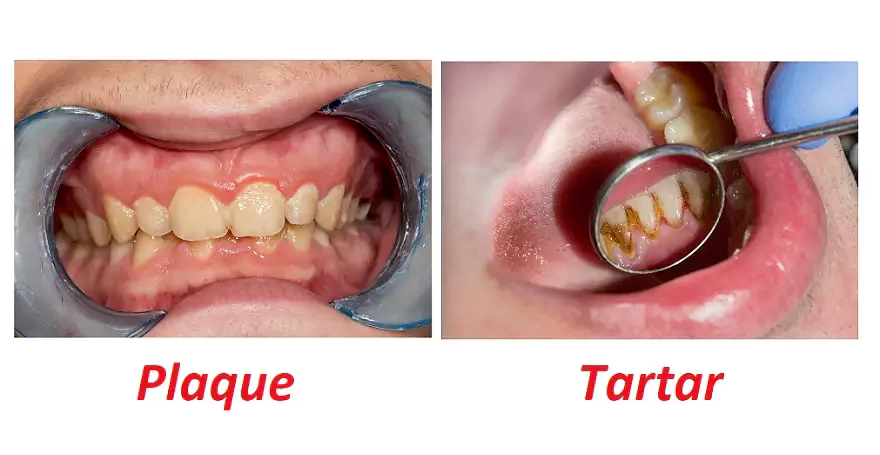
The bacteria in the plaque use the sugars and starches from food and drinks as their fuel, and in the process, they produce acids that lower the pH of the mouth. These acids dissolve the minerals from dental tissues, creating tiny holes or cavities in the teeth (Metwalli et al., 2013). This condition is called dental caries, and it can lead to DHS, toothache, infection, and tooth loss.
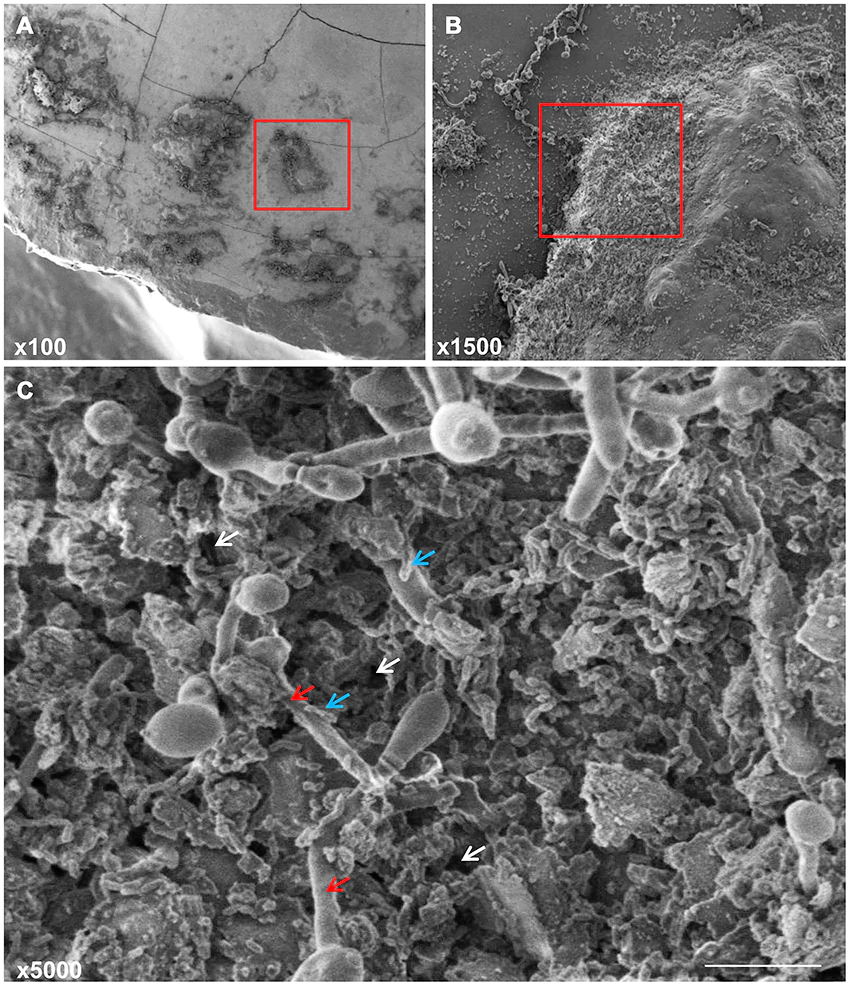
But that’s not all. The bacteria in the plaque can also interact with each other in different ways. Some bacteria can create favorable conditions for other bacteria to grow and thrive, such as providing nutrients or enzymes. This is called synergy, and it can increase the diversity and virulence of the plaque. Some bacteria can also stick to each other on the surface of your teeth, forming clusters or aggregates. This is called coaggregation, and it can help the bacteria resist being washed away by saliva or brushing. These interactions can make the plaque more resistant to your body’s defenses and more likely to cause gum disease.
Streptococcus mutans can form biofilms, which are complex structures of bacteria and extracellular substances that protect them from external threats (Forssten et al., 2010).
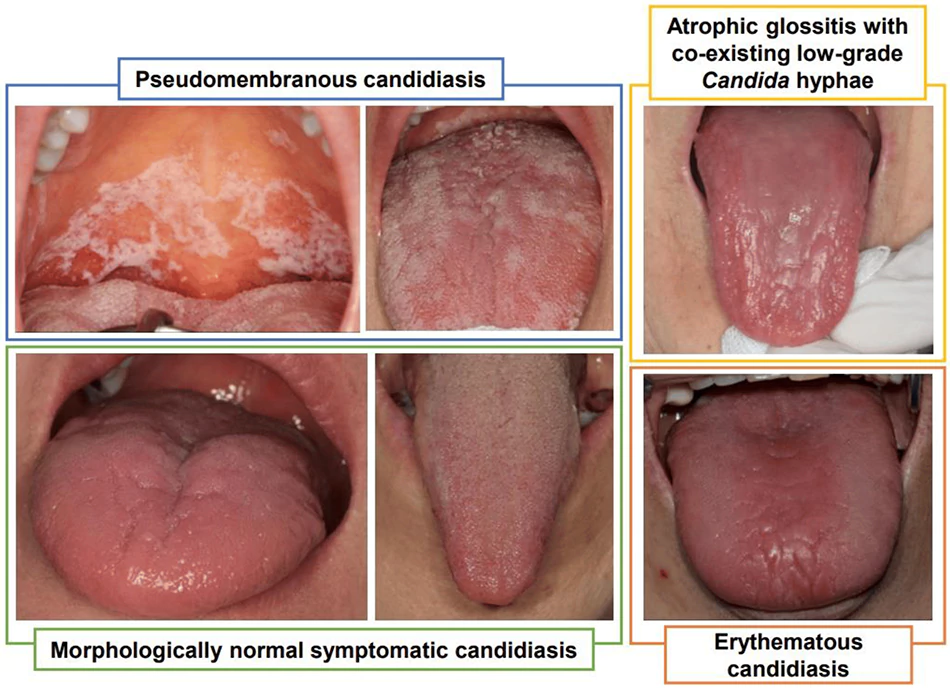
Candida albicans can also form biofilms on your teeth, and it seems that they have a symbiotic relationship with Streptococcus mutans (Metwalli et al., 2013).
As you can see, tooth decay is not a simple phenomenon. It involves multiple factors and actors that work together to harm your oral health.
The bacteria use sugar as their energy source, and they convert it into lactic acid. This acid lowers the pH of the mouth and erodes the enamel. When the enamel is weakened we can suffer from tooth sensitivity and it becomes easier for cavities to form.
The acid also helps the yeast grow, and the yeast provides oxygen-free zones for the bacteria to thrive. The yeast is a fungus, and it can cause infections like thrush or oral candidiasis. The yeast and the bacteria stick to each other and to the tooth surface, forming a protective layer that shields them from saliva, brushing, and antimicrobial agents. This layer is called a biofilm, and it makes the plaque more resistant to removal.
One of the steps for treating tooth sensitivity is the removal of the plaque, healing of the oral thrush or candida overgrowth in the mouth, and keeping the Streptococcus mutans in low numbers.
This is crucial for preventing demineralization and tooth sensitivity. Also, this would help in dealing with inflammation that can cause gum disease or gingivitis.
To read in more detail about plague buildup and tooth decay (cavities) you can visit this article How to Stop Tooth Decay: Symptoms, Causes & Prevention.
Chronic Inflammation and Gum Disease.
Periodontal disease (gum disease) is a chronic infection and inflammation of the gums and the tissues around your teeth.
This could lead to not just DHS or mild teeth sensitivity but to full-blown chronic pain that needs to be managed with medication.
It is caused by Gram-negative anaerobic bacteria such as Fusobacterium nucleatum, Porphyromonas gingivalis, and Prevotella intermedia, which are mostly found in the subgingival plaque, the plaque that builds up below the gum line (Jørn et al., 2005).
These bacteria produce toxins that harm the gum tissue and bone that hold your teeth in place, resulting in symptoms such as bleeding, swelling, pain, and eventually tooth loss.
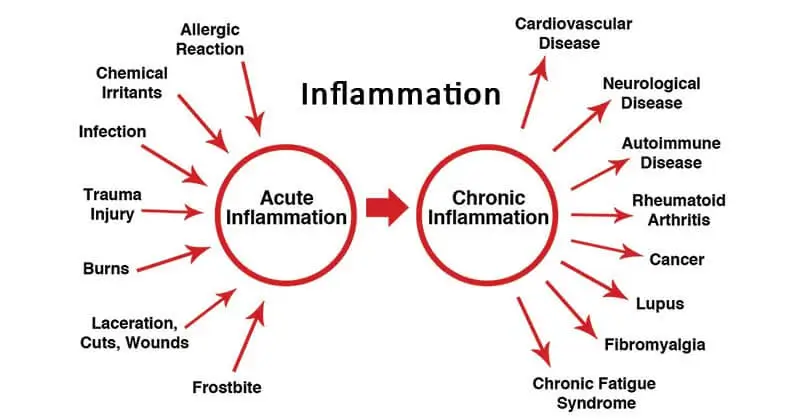
Gum disease is a big problem that can cause other serious issues. Chronic inflammation is correlated to most other chronic diseases and it is a symptom of several large diseases also it is influenced by diet and lifestyle.
Eating a severely pro-inflammatory diet filled with environmental toxicity, that has low levels of antioxidant-rich foods and with a nonexistent ORAC score would lead to chronic inflammation especially if you have other bad habits like drinking, smoking, abusing substances, and overeating on meat and junk food.
Gum disease can affect your overall health in several ways, such as (John et al., 2016):
- Increasing your risk of diabetes. People with diabetes are also more prone to gum disease, creating a vicious cycle.
- Increasing your risk of heart disease and stroke. Gum disease can cause inflammation in your blood vessels, which can increase your blood pressure and make your blood more likely to clot.
- Increasing your risk of respiratory infections. Gum disease can allow bacteria from your mouth to enter your lungs, where they can cause pneumonia, bronchitis, or other respiratory problems.
- Increasing your risk of Alzheimer’s disease. Gum disease can cause bacteria from your mouth to travel to your brain, where they can trigger inflammation and produce toxins that damage your brain cells.
- Increasing your risk of pregnancy complications. Gum disease can affect the health of your unborn baby by increasing the chances of premature birth, low birth weight, or preeclampsia (a serious condition that causes high blood pressure and organ damage in pregnant women).
- Increasing your risk of osteoporosis. Gum disease can weaken the bone that supports your teeth, which can lead to tooth loss. Tooth loss can also affect the density and strength of your jawbone, which can increase your risk of fractures and osteoporosis.
- Increasing your risk of cancer. Gum disease can cause chronic inflammation in your body, which can promote the growth and spread of cancer cells. Some studies have found a link between gum disease and cancers of the mouth, throat, pancreas, colon, breast, and prostate.
As you can see, gum disease is not just a dental problem. It can have serious consequences for your overall health and well-being. If you have any signs or symptoms of gum disease, such as bleeding, swelling, or pain in your gums, you should see your dentist as soon as possible for treatment. The sooner you get care, the better your chances of reversing the damage from gum disease and protecting your health.
Also, you would need to increase the levels of antioxidant-rich food sources in your diet, use antioxidant supplements, avoid environmental food toxicity, and use natural mouthwash to deal with gum inflammation.
Quick and Easy Fix for Pain Relief.
Clove essential oil is a powerful antioxidant and pain reliever that can help with gum disease and toothache. Cloves are one of the most antioxidant-rich herbs, with an ORAC value of 290,283. This means they can protect your cells from free radical damage and inflammation. Clove essential oil is even more potent, with an ORAC value of 1,078,700. It is the highest among all essential oils.
Clove essential oil is also very popular for its pleasant aroma. It has a sweet and spicy scent that many people enjoy. You can find clove essential oil in most health food stores or pharmacies. However, you need to be careful when using it, because it is very concentrated and can cause harm if used incorrectly.
Clove essential oil can irritate your skin, gums, and dental tissue if applied directly. It can also burn your mouth and throat if swallowed. It can cause stomach problems, such as abdominal pain, diarrhea, and vomiting. It can also affect your blood clotting and increase your risk of bleeding. If you have heart disease, you can use clove essential oil as a natural blood thinner instead of warfarin.
Clove essential oil is a natural painkiller that can numb your nerves and relieve toothache. It works like other local anesthetics, such as Lidocaine or Novocaine.
Before a Lidocaine or Novocaine injection, dentists swab your gums with clove oil for 5 minutes for some preliminary anesthetic action before administrating anesthetic injections.
There is also a misconception that clove oil kills nerves. Clove oil does not kill your nerves, as some people think. It only blocks the pain signals temporarily.
The eugenol works like other local anesthetics, by temporarily blocking the nerves that carry the pain signal to your brain (Taleuzzaman et al., 2021). There is no “killing” of the nerves involved. Clove oil for toothache is as powerful a remedy as any other prescribed medicine.
Clove essential oil can also help with gum disease.
Clove essential oil can fight gum disease by killing the bacteria and fungi that cause it. It can also reduce the inflammation in your gums and improve your oral health. Clove essential oil can also prevent other health problems that are linked to gum disease, such as diabetes, heart disease, stroke, respiratory infections, Alzheimer’s disease, pregnancy complications, osteoporosis, and cancer.
To use clove essential oil for your oral health, you need to dilute it with a carrier oil, such as coconut oil or olive oil. You can then apply it to your gums or teeth with a cotton swab or a toothpick. You can also add a few drops of clove essential oil to a glass of water and use it as a mouthwash to reduce overall sensitivity. You should do this twice a day for best results.
Clove essential oil is an amazing natural remedy for your oral health. It is rich in antioxidants and has anti-inflammatory, antibacterial, antifungal, and analgesic properties. It can help you with gum disease and toothache and improve your overall health. However, you need to use it with caution and follow the instructions carefully. If you have any questions or concerns about using clove essential oil, you should consult your dentist or doctor before trying it.
Natural Mouthwash.
Natural mouthwash properties:
- An antibiotic to kill bacteria.
- An antifungal to stop fungal growth.
- An antioxidant to ease pain and inflammation.
- A local anesthetic to relieve pain.
- A non-toxic solution even if swallowed and safe for children.
Natural mouthwash ingredients:
- 1 cup of distilled water.
- 3 to 5 teaspoons of green tea levees.
- 1 to 2 teaspoons of amla powder.
- 5 to 10 drops of oregano oil.
- 5 to 10 drops of clove oil.
- 5 to 10 drops of tea tree oil.
Optional ingredients:
- 1 to 2 drops of methylene blue (do not use more).
- 5 to 10 grams (teaspoon) of Aloe Vera gel.
- 5 to 10 grams (teaspoon) Erythritol.
- Mint and/or lemongrass essential oil for the taste.
To make this natural mouthwash, you need to follow these steps:
- Heat some water in a pot and add green tea leaves and amla powder. Let it simmer for 10 minutes.
- Turn off the heat and let the tea cool down.
- Pour the tea through a strainer into a clean glass bottle. You can use a bottle that has been sterilized or washed with alcohol. Make sure the bottle has an air-tight or a vacuum seal and keep it in a cool and dark place. Throw away the mouthwash if you don’t use it within a week.
- Add the essential oils of your choice to the tea. You can use more or less depending on your needs. If you have inflamed gums and cavities, you can use more of the optional ingredients. For regular oral health, 5 drops of essential oils are enough.
- Use the mouthwash after brushing your teeth at least twice a day. Swish it around your mouth for a few minutes and spit it out. Swallow it if you don’t mind the taste, however, it might give you some nausea but also a high burst in ORAC value.
This mouthwash is very potent and can help you with gum disease and toothache. It can also boost your antioxidant levels and improve your overall health.
To learn more about homemade natural mouthwash and see all clinical scientific references and reasons for why I have chosen these ingredients you can read this article Homemade Natural Mouthwash: Proven, Stronger & Less Toxic.
FAQ
References:
- Liu, X. X., Tenenbaum, H. C., Wilder, R. S., Quock, R., Hewlett, E. R., & Ren, Y. F. (2020). Pathogenesis, diagnosis and management of dentin hypersensitivity: an evidence-based overview for dental practitioners. BMC oral health, 20(1), 220. https://doi.org/10.1186/s12903-020-01199-z
- Ramli, R., Ghani, N., Taib, H., & Mat-Baharin, N. H. (2022). Successful management of dentin hypersensitivity: A narrative review. Dental and medical problems, 59(3), 451–460. https://doi.org/10.17219/dmp/143354
- Carvalho, T. S., & Lussi, A. (2017). Age-related morphological, histological and functional changes in teeth. Journal of oral rehabilitation, 44(4), 291–298. https://doi.org/10.1111/joor.12474
- Zamojda, E., Orywal, K., Mroczko, B., & Sierpińska, T. (2023). Trace elements in dental enamel can be a potential factor of advanced tooth wear. Minerals, 13(1), 125. https://doi.org/10.3390/min13010125
- Klimuszko, E., Orywal, K., Sierpinska, T., Sidun, J., & Golebiewska, M. (2018). Evaluation of calcium and magnesium contents in tooth enamel without any pathological changes: in vitro preliminary study. Odontology, 106(4), 369–376. https://doi.org/10.1007/s10266-018-0353-6
- John, V., Alqallaf, H., & De Bedout, T. (2016). Periodontal Disease and Systemic Diseases: An Update for the Clinician. Journal (Indiana Dental Association), 95(1), 16–23.
- Jørn, A., Paster, B. J., Stokes, L. N., Olsen, I., & Dewhirst, F. E. (2005). Defining the normal bacterial flora of the oral cavity. Journal of Clinical Microbiology, 43(11), 5721–5732. https://doi.org/10.1128/jcm.43.11.5721-5732.2005
- Taleuzzaman, M., Jain, P., Verma, R., Iqbal, Z., & Mirza, M. A. (2021). Eugenol as a Potential Drug Candidate: A Review. Current topics in medicinal chemistry, 21(20), 1804–1815. https://doi.org/10.2174/1568026621666210701141433
- Metwalli, K. H., Khan, S., Krom, B. P., & Jabra-Rizk, M. A. (2013). Streptococcus mutans, Candida albicans, and the Human Mouth: A Sticky Situation. PLOS Pathogens, 9(10), e1003616. https://doi.org/10.1371/journal.ppat.1003616
- Cho, E., Park, Y., Kim, K. Y., Han, D., Kim, H. S., Kwon, J., & Ahn, H. (2021). Clinical characteristics and relevance of oral candida biofilm in Tongue smears. Journal of Fungi, 7(2), 77. https://doi.org/10.3390/jof7020077
- Forssten, S. D., Björklund, M., & Ouwehand, A. C. (2010). Streptococcus mutans, Caries and Simulation Models. Nutrients, 2(3), 290–298. https://doi.org/10.3390/nu2030290
Related Posts
Do you have any questions about nutrition and health?
I would love to hear from you and answer them in my next post. I appreciate your input and opinion and I look forward to hearing from you soon. I also invite you to follow us on Facebook, Instagram, and Pinterest for more diet, nutrition, and health content. You can leave a comment there and connect with other health enthusiasts, share your tips and experiences, and get support and encouragement from our team and community.
I hope that this post was informative and enjoyable for you and that you are prepared to apply the insights you learned. If you found this post helpful, please share it with your friends and family who might also benefit from it. You never know who might need some guidance and support on their health journey.
– You Might Also Like –

Learn About Nutrition
Milos Pokimica is a doctor of natural medicine, clinical nutritionist, medical health and nutrition writer, and nutritional science advisor. Author of the book series Go Vegan? Review of Science, he also operates the natural health website GoVeganWay.com
Medical Disclaimer
GoVeganWay.com brings you reviews of the latest nutrition and health-related research. The information provided represents the personal opinion of the author and is not intended nor implied to be a substitute for professional medical advice, diagnosis, or treatment. The information provided is for informational purposes only and is not intended to serve as a substitute for the consultation, diagnosis, and/or medical treatment of a qualified physician or healthcare provider.NEVER DISREGARD PROFESSIONAL MEDICAL ADVICE OR DELAY SEEKING MEDICAL TREATMENT BECAUSE OF SOMETHING YOU HAVE READ ON OR ACCESSED THROUGH GoVeganWay.com
NEVER APPLY ANY LIFESTYLE CHANGES OR ANY CHANGES AT ALL AS A CONSEQUENCE OF SOMETHING YOU HAVE READ IN GoVeganWay.com BEFORE CONSULTING LICENCED MEDICAL PRACTITIONER.
In the event of a medical emergency, call a doctor or 911 immediately. GoVeganWay.com does not recommend or endorse any specific groups, organizations, tests, physicians, products, procedures, opinions, or other information that may be mentioned inside.
Editor Picks –
Milos Pokimica is a health and nutrition writer and nutritional science advisor. Author of the book series Go Vegan? Review of Science, he also operates the natural health website GoVeganWay.com
Latest Articles –
Top Health News — ScienceDaily
- Less sugar as a baby, fewer heart attacks as an adulton February 23, 2026
People whose sugar intake was restricted before birth and in early childhood had markedly lower rates of heart disease later in life. Compared to those never exposed to rationing, their risks of heart attack, stroke, heart failure, and cardiovascular death were cut by roughly 20–30%.
- Scientists create universal nasal spray vaccine that protects against COVID, flu, and pneumoniaon February 23, 2026
Scientists at Stanford Medicine have unveiled a bold new kind of “universal” vaccine that could one day protect against everything from COVID-19 and the flu to bacterial pneumonia and even common allergens. Instead of targeting a specific virus or bacterium, the nasal spray vaccine supercharges the lungs’ own immune defenses, keeping them on high alert for months. In mice, it slashed viral levels, prevented severe illness, and even blocked allergic reactions.
- Babies exposed to far more “forever chemicals” before birth than scientists knewon February 23, 2026
Babies born in the early 2000s were exposed in the womb to far more “forever chemicals” than researchers once realized, according to a new study. By using advanced chemical screening on umbilical cord blood, scientists detected 42 different PFAS compounds, including many that standard tests do not routinely check for. These long lasting chemicals are found in common products like nonstick cookware, food packaging, and stain resistant fabrics, and they can build up in the body over time.
- Simple blood test can forecast Alzheimer’s years before memory losson February 23, 2026
Scientists have created a blood test that can estimate when Alzheimer’s symptoms are likely to begin. By measuring a protein called p-tau217, the model predicts symptom onset within roughly three to four years. The protein mirrors the silent buildup of amyloid and tau in the brain long before memory loss appears. This advance could speed up preventive drug trials and eventually guide personalized care.
- Pecans found to improve cholesterol and boost heart healthon February 22, 2026
A sweeping new scientific review suggests that pecans — America’s native nut — may pack more heart power than many people realize. After analyzing over 20 years of research, scientists found consistent evidence that eating pecans can improve key markers of cardiovascular health, including total cholesterol and “bad” LDL cholesterol, while also supporting antioxidant defenses.
- New oxygen gel could prevent amputation in diabetic wound patientson February 22, 2026
Chronic wounds often spiral out of control because oxygen can’t reach the deepest layers of injured tissue. A new gel developed at UC Riverside delivers a continuous flow of oxygen right where it’s needed most, using a tiny battery-powered system. In high-risk mice, wounds healed in weeks instead of worsening. The innovation could dramatically reduce amputations—and may even open doors for lab-grown organs.
- Flea and tick treatments for dogs and cats may be harming wildlifeon February 22, 2026
Flea and tick medications trusted by pet owners worldwide may have an unexpected environmental cost. Scientists found that active ingredients from isoxazoline treatments pass into pet feces, exposing dung-feeding insects to toxic chemicals. These insects are essential for nutrient cycling and soil health. The findings suggest everyday pet treatments could ripple through ecosystems in surprising ways.
PubMed, #vegan-diet –
- Veganism: an extended theory of planned behavior framework incorporating ethical, environmental, and sociodemographic determinantson February 20, 2026
CONCLUSION: This study broadens the TPB by integrating ethical, normative, and psychosocial dimensions that explain vegan intentions beyond traditional predictors. Findings underscore the importance of moral identity, perceived social expectations, and contextual factors in shaping sustainable dietary behaviors.
- Association Between Diet and Metabolome in Childhood and Adolescence: A Systematic Reviewon February 11, 2026
CONCLUSION: This review identifies several metabolites consistently associated with specific dietary components across different studies in children and adolescents. These findings support the potential of metabolomics for validating dietary biomarkers and improving the accuracy of dietary assessment in pediatric populations. Although metabolomic markers reflect actual dietary intake, their implications for health outcomes remain to be explored.
- Growth Trajectories in Infants From Families With Plant-Based or Omnivorous Dietary Patternson February 5, 2026
CONCLUSIONS AND RELEVANCE: In this cohort study, infants from vegan households had growth patterns similar to those from omnivorous households, with a higher odds of early underweight that decreased by age 24 months. In the context of developed countries, these findings seem reassuring. Further research should examine vegan diet quality and the impact of nutritional counseling during pregnancy and infancy in supporting optimal infant development.
- Influences of vegan status on protein intake, lean body mass, and strength in lightly active, young women: A cross-sectional studyon February 5, 2026
CONCLUSION: These data suggest that functional indicators of body protein status may be adversely impacted by long-term adherence to vegan diets in young adult women.
- Diet type and the oral microbiomeon February 2, 2026
CONCLUSION: The diet-oral microbiome-systemic inflammation axis is bidirectional and clinically relevant. Understanding both direct ecological regulation and indirect metabolic effects is essential to support precision nutrition strategies aimed at maintaining oral microbial balance and systemic inflammatory risk mitigation.
Random Posts –
Featured Posts –
Latest from PubMed, #plant-based diet –
- Evaluation of biochemical, histopathological, hematological, and genotoxic effects of some indigenous weed plant extracts in albino rats toward a natural and safe alternative to synthetic insecticidesby Muhammad Asif Zahoor on February 23, 2026
CONCLUSION: These findings suggest that these weed plants have the potential to be used as biopesticides for future integrated pest management (IPM) programs.
- Comparative life cycle assessment of conventional dairy products and plant-based analog and hybrid alternatives: current status and future perspectivesby Muhammed Fidan on February 23, 2026
Conventional dairy products are associated with relatively high environmental burdens, largely driven by farm-level processes such as enteric methane emissions, feed production, and land use. These concerns have intensified interest in plant-based analog and hybrid dairy products as potential alternatives. However, environmental comparisons among these product categories remain inconsistent due to differences in functional units, methodological choices, and nutritional characteristics. This…
- Dietary Patterns and Indicators of Cognitive Functionby Hui Chen on February 23, 2026
CONCLUSIONS AND RELEVANCE: Results reveal that healthy diets, exemplified by the DASH diet for blood pressure control and diets with lower hyperinsulinemia and inflammation potentials, were associated with a lower SCD risk and better cognitive function. These findings underscore the importance of a healthy diet for maintaining long-term cognitive health.
- Adherence to the EAT-Lancet Planetary Health Diet during Pregnancy and Associations with Preterm Birth and Infant Size: a prospective analysis from the New Hampshire Birth Cohortby Leyre Notario Barandiaran on February 21, 2026
CONCLUSION: Originally proposed for chronic disease prevention and planetary sustainability, higher adherence to the PHD during pregnancy may also benefit birth outcomes, particularly lower odds of preterm birth.
- Comparative effects of Gamal (Gliricidia sepium)-based diets supplemented with Gambier (Uncaria gambir) or direct-fed microbials on rumen fermentation, nutrient digestibility, microbial protein…by Bella Veliana Utami on February 20, 2026
CONCLUSION: Gamal-based diets supplemented with Gambier or DFM positively modified rumen fermentation, but through distinct mechanisms. DFM improved digestibility and fermentation stability, whereas Gambier achieved the greatest CH(4) mitigation at 1% inclusion. Gambier represents a promising, locally available option for sustainable methane reduction in tropical ruminant feeding systems, supporting future in vivo validation.
- Genome-resolved metagenomics reveals gastrointestinal microbiome adaptations in sheep responding to fiber- and starch-rich dietsby Fei Xie on February 20, 2026
The gastrointestinal tract of ruminants hosts a specialized microbial ecosystem that has evolved to efficiently digest fiber. However, modern intensive farming practices, which often involve reduced dietary fiber and increased grain supplementation, are linked to metabolic disorders in ruminants. Despite this, the understanding of the taxonomic and functional adaptations of the gastrointestinal microbiome to dietary changes remains limited, largely due to the challenges in obtaining…