Low Histamine Diet and Histamine Intolerance: Complete Gide
One way to manage histamine intolerance is to follow a low histamine diet. This means avoiding foods that are high in histamine or that can trigger its release.
Milos Pokimica
Written By: Milos Pokimica
Medically Reviewed by: Dr. Xiùying Wáng, M.D.
Updated January 5, 2026Key Takeaways:
– Histamine is a natural chemical that the body produces to fight off foreign invaders and protect us from harm. It plays a vital role in immune responses, gut functions, brain functions, and other bodily processes.
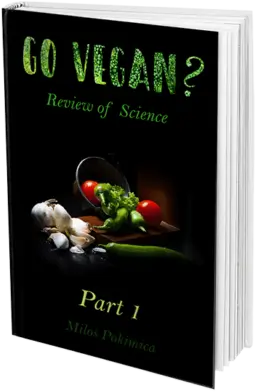
– Histamine works by binding to specific receptors. There are four types of these receptors: H1R, H2R, H3R, and H4R. Each one has a different function and location in the body and affects different aspects of health.
– Histamine intolerance is a condition where the body cannot tolerate normal amounts of histamine and reacts with symptoms like headaches, nasal congestion, fatigue, hives, digestive issues, irregular menstrual cycle, nausea, and vomiting. In severe cases, it can also cause abdominal cramping, tissue swelling, high blood pressure, irregular heart rate, anxiety, difficulty regulating body temperature, and dizziness.
– Histamine intolerance can be caused by various factors such as allergies, medications, gastrointestinal disorders, histamine-rich foods, or genetics. To lower the levels and symptoms, one can avoid or reduce exposure to these triggers, support the enzyme that breaks down histamine (DAO), eat a low histamine diet, and take supplements or medications that help regulate high levels.
What is Histamine and Why Should You Care?
Have you ever wondered what causes allergy symptoms? You know, the sneezing, itching, swelling, redness, and other unpleasant reactions that make you feel miserable. Beyond the initial allergen, what is the substance that actually creates allergy symptoms? Well, the answer is histamine.
Histamine is a natural chemical that our body produces to fight off foreign invaders and protect us from harm.
Although necessary for our body’s normal functions, sometimes it can do more harm than good. This article will explain what histamine is, what can go wrong when the levels get out of balance, and different methods we can use including our diet to get the histamine intolerance under control.
Summary:
Histamine, a natural immune response chemical, can trigger allergy symptoms when levels are imbalanced.
Histamine: The Good and the Bad.
Histamine is categorized as a substance called amine. Amine is a type of molecule that is derived from amino acids and in this case from L-histidine. Amino acids act as the basic components required for protein formation in the body. Histamine also plays a vital role in several bodily processes such as:
- Immune responses: It is released by special cells called basophils and mast cells when they detect a foreign substance or pathogen in your body. It helps the immune system to fight off the infection by making your blood vessels leaky. This creates swelling but also increases inflammation by allowing white blood cells and proteins to reach the infected area (King et al., 2000). It also makes you itch and sneeze to get rid of the allergen.
- Gut functions: Within the gastrointestinal tract, histamine is present at relatively high concentrations, especially if there is inflammation (Smolinska et al, 2022). It regulates the movement and secretion of your digestive tract. It helps you digest food by stimulating the production of stomach acid and enzymes (Hirschowitz, 1985). It also controls the contraction of your intestines and the absorption of nutrients (Hirschowitz, 1985).
- Brain functions: It acts as a neurotransmitter in your brain and spinal cord. It affects your mood, sleep, appetite, learning, memory, and pain perception (Obara et al., 2020).
As we can see, it plays a vital and versatile role in regulating different bodily functions and this is exactly why we can just take antihistaminic drugs out of the box. It needs to be in balance. An excess or deficiency can lead to complications.

This can happen for various reasons, such as:
- Histamine intolerance: It is a health condition in which individuals face difficulty breaking down regular histamine that they obtain from their food or body (Pinzer et al., 2018). This can result in chronically elevated levels in their blood and tissues. In the time period if not corrected this condition can lead to various symptoms like fatigue, headaches (Wantke et al.,1993), hives (Son et al., 2018), nasal congestion, digestive issues, and more. Deficiency or dysfunction of one specific enzyme called diamine oxidase (DAO), which breaks down histamine in the gut and other organs, is the usual cause of intolerance in almost all cases (Mušič et al., 2013).
- Histamine poisoning: Consuming foods that have high amounts or those that stimulate the release in the body is another way we can get exposed to excessive levels. These foods include alcohol, fermented foods, dried fruits, shellfish, aged cheese, etc. The consumption of these foods may lead to symptoms including flushing, rash, diarrhea, vomiting, headache (Wantke et al.,1993), and so on. To prevent poisoning if we are sensitive, we have to avoid such foods or take antihistamines before consuming them.
- Histamine imbalance: Imbalance may occur due to several factors including stress, medications, infections, hormones, or inflammation resulting in either excess or insufficient levels. Consequently, histamine imbalance can trigger symptoms and disorders like asthma, allergies, migraine, depression, anxiety, eczema (Maintz et al., 2006), irritable bowel syndrome (IBS)(Böhn et al., 2013), etc. Treatment of this condition involves identifying and addressing the underlying cause, as well as using natural or pharmacological therapies to restore the balance.
Summary:
Histamine imbalance due to intolerance, poisoning, or other factors can trigger various symptoms and disorders like allergies, migraines, and IBS.
How Histamine Works.
It works by binding to specific receptors called histamine receptors. Think of them as hands that grab onto histamine molecules. They’re located on the surface of different cells and tissues throughout the body. They are divided into four categories, called H1R, H2R, H3R, and H4R and each one has a different function (Obara et al., 2020).
Each type of receptor has a different function and effect on allergic responses. For example:
H1R: Found on smooth muscle cells (like those in airways and blood vessels), endothelial cells (lining the walls of your blood vessels), nerve cells (such as those which regulate pain and itching) as well as many different types of immune cells (such as mast cells and basophils). When it binds to the H1R receptor, it instigates a series of effects. You feel the constriction of your smooth muscle cells, increased permeability of the walls of your blood vessels, and swelling; it turns on alarm bells to your nerves pricking them up for a potential itch attack; sets-off fireworks to your mast cell activation sending hints of inflammation round-your body. All this with end result being allergic rhinitis (hay fever), atopic dermatitis (eczema) (Maintz et al., 2006), asthma, anaphylaxis, or urticaria (hives).
H2R: H2R is found in different places in your body, such as the stomach, heart, skin, and immune system. Let me tell you what H2R does in each of these places.
In the stomach (Prinz et al., 1999), H2R is on the gastric parietal cells that make stomach acid. When histamine attaches to H2R, it tells these cells to make more acid. This helps you digest food, but too much acid can cause ulcers or sores in the stomach lining.
In the heart, H2R is on the cardiac muscle cells (the cells that make up the heart). When histamine attaches to H2R, it makes the heart beat faster and stronger. This helps you pump blood around your body, but too much stimulation can cause arrhythmias or abnormal heart rhythms.
In the skin, H2R is present in the mast cells that release histamine. When histamine attaches to H2R, it stops these cells from releasing more of it. This is a feedback loop that our body uses to keep the level in balance. This helps in the control of inflammation and itching, but too little can impair wound healing or infection-fighting and this is a reason why we should not take antihistamines out of the box.
In the immune system, H2R is on immune cells (such as T cells and macrophages). When histamine attaches to H2R, it changes how these cells behave. This helps regulate immune response, but too much or too little modulation can cause autoimmune diseases or allergies.
As you can see, H2R is a very important receptor that affects many aspects of our health. Histamine and H2R work together to keep the body in balance, but sometimes they can go out of sync and cause problems. That’s why some people take drugs that block H2R to treat ulcers, arrhythmias, or allergies. These drugs are called H2 blockers or antihistamines. Maybe you have heard of them or used them before.
H3R: Histamine is also a neurotransmitter, and one of the most important ones, that sends signals between nerve cells. To do this, it needs a receptor called H3R. H3R is found in nerve cells, in the brain and spinal cord which makes the central nervous system (CNS), and in the arms and legs which makes the peripheral nervous system (PNS).
In CNS, H3R acts like a brake on nerve cells. When histamine attaches to H3R, it slows down the nerve cells and makes them release fewer neurotransmitters. H3R modulates the release and action of various neurotransmitters, such as acetylcholine, dopamine, serotonin, norepinephrine, etc. This affects how you feel and think. For example, H3R is involved in sleep-wake regulation. It helps you stay awake by blocking HR3. H3R also helps you learn and remember by controlling the release and action of other neurotransmitters, such as acetylcholine, dopamine, serotonin, etc.
In PNS, H3R also acts like a brake on nerve cells. When histamine attaches to H3R, it reduces the activity of nerve cells that carry signals from your body to the brain. This affects how you sense and react. For example, H3R helps you control your appetite and metabolism by regulating the signals that tell you when you are hungry or full. H3R also helps you cope with pain by modulating the signals that make you feel pain (Obara et al., 2020).
H3R also acts as a gatekeeper on the blood-brain barrier. This is a layer of cells that separates your blood from your brain and protects your brain from harmful substances. When histamine attaches to H3R, it changes the permeability of the blood-brain barrier and allows more or less substances to pass through.
As you can see, H3R is a very important receptor that affects many aspects of your health. Histamine and H3R work together to keep the brain and nerves in balance, but sometimes they can go out of sync and cause problems. That’s why some people take drugs that activate H3R to treat sleep disorders, cognitive impairments, obesity, pain, or brain injuries. These drugs are called H3 agonists or enhancers.
Histamine effects on the nervous system:
- Sleep-wake cycle: It helps with wakefulness and alertness, but too much of it can disrupt our normal sleep patterns and cause insomnia or excessive daytime sleepiness.
- Neurotransmitter regulation: It interacts with other neurotransmitters and with the brain as a whole. Too much of it slows down the nerve cells and makes them release fewer neurotransmitters.
- Stress response: It helps you cope with stress, but too much can make you more anxious, irritable, or depressed.
- Pain perception: It helps with pain sensation, but too much of it can make us more sensitive to pain (Obara et al., 2020) or cause headaches or migraines (Wantke et al.,1993).
- Satiety, taste perception, and feeding behaviors: It helps you regulate your appetite and metabolism, but too much of it can make us lose or gain weight, crave certain foods, or have digestive issues.
- Addictive behaviors: It helps with the control of impulses and rewards, but too much of it can make us more prone to addiction or compulsive behaviors.
- Memory formation: It helps with learning and remembering, but too much of it can impair memory or cause confusion or brain fog.
- Motivation and goal-setting behaviors: It helps us set and pursue goals, but too much of it can make us lose interest or focus.
H4R: This receptor is found on immune cells and some nerve cells (such as those in your skin and spinal cord). When histamine binds to H4R, it causes activation of immune cells (leading to increased histamine release and inflammatory cytokine production) and stimulation of nerve cells (leading to itching and pain).
H4R is found in different places in the body, such as the immune system and nerves.
In the immune system, H4R is on the cells that protect us from germs and allergens. These include mast cells, basophils, eosinophils, dendritic cells, T cells, B cells, and so on. When histamine attaches to H4R, it activates these cells and makes them release more histamine and other inflammatory substances (inflammatory cytokine production). This helps fight off infections and allergies, but too much inflammation can cause damage.
In nerves, H4R is on some of the cells that carry signals from the skin and spinal cord to the brain. These include sensory neurons and glial cells. H4R mediates mast cell activation (which triggers allergic reactions), chemotaxis of inflammatory cells (which attracts them to the site of inflammation), modulation of immune responses (such as Th1/Th2 balance and antibody production), and pruritus (itching). When histamine attaches to H4R, it stimulates these cells and makes them send signals of itching and pain. This helps you notice when something is wrong with your skin or body, but too much stimulation can cause discomfort or distress.
Histamine and H4R work together to keep the immune system and nerves in balance, but sometimes they can go out of sync and cause problems. That’s why some people take drugs that block H4R to treat inflammation, allergies, itching, or pain. These drugs are called H4 antagonists or inhibitors.
As you can see, histamine receptors have diverse and complex roles. They are like switches that can turn on or off the actions of histamine in different parts of the body. Depending on which receptor histamine binds to effects will be different. Also where the receptor is located, there are different receptors in the same cells. Also how much of it is present, the receptor can either boost or reduce the effects of histamine. This means that by knowing how histamine receptors work, you can find ways to control your histamine levels and symptoms.
| Symptom | Explanation |
| Itching, redness, hives and/or swelling of the lips, tongue, or skin | These are signs of an allergic skin reaction (Maintz & Novak, 2007). |
| Red eyes | This is a symptom of conjunctivitis, an inflammation of the eye membrane (Maintz & Novak, 2007). |
| Swollen eyelids | This is a sign of angioedema, a swelling of the deeper layers of the skin (Maintz & Novak, 2007). |
| Atopic eczema | This is a chronic inflammatory skin condition that can be worsened by histamine intolerance (Maintz & Novak, 2007). |
| Sneezing and nasal congestion | These are symptoms of rhinitis, an inflammation of the nasal mucosa (Maintz & Novak, 2007). |
| Asthma | This is a chronic respiratory disorder that can be aggravated by histamine intolerance due to bronchoconstriction and mucus secretion (Maintz & Novak, 2007). |
| Low blood pressure | This is a result of vasodilation and hypotension caused (Maintz & Novak, 2007). |
| Heart arrhythmia | This is an abnormal heart rhythm that can be triggered due to the cardiac effects of histamine. (Maintz & Novak, 2007). |
| Abdominal pain | This is a symptom of gastrointestinal distress caused by histamine affecting the stomach and intestines (Comas-Basté et al., 2020). |
| Bloating | This is a symptom of gas accumulation in the digestive tract caused by effects on intestinal motility and permeability. (Comas-Basté et al., 2020). |
| Diarrhea | This is a symptom of increased intestinal fluid secretion caused by effects on the intestinal epithelium (Comas-Basté et al., 2020). |
| Gas | This is a symptom of gas accumulation in the digestive tract caused by effects on intestinal motility and permeability (Comas-Basté et al., 2020). |
| Nausea | This is a symptom of gastric irritation and stimulation of the vomiting center in the brain caused by effects on the stomach and central nervous system. (Comas-Basté et al., 2020). |
| Vomiting | This is a symptom of the forceful expulsion of stomach contents caused by histamine affecting the stomach and central nervous system (Comas-Basté et al., 2020). |
| Headache | This is a symptom of the dilation of blood vessels in the brain (Maintz & Novak, 2007). |
| Dizziness | This is a symptom of altered balance and spatial orientation caused by effects on the inner ear and central nervous system (Maintz & Novak, 2007). |
| Sleep disturbances | This is a symptom of an altered sleep-wake cycle and quality caused by effects on the brain and circadian rhythm (Comas-Basté et al., 2020). |
| Menstrual irregularity | This is a symptom of altered hormonal balance and uterine contraction caused by caused by effects on the reproductive system (Maintz & Novak, 2007). |
| Chronic fatigue | This is a symptom of reduced energy production and increased inflammation caused by effects on the cellular metabolism and immune system (Comas-Basté et al., 2020). |
| Anxiety | This is a symptom of increased nervousness and stress caused by effects on the brain and neurotransmitters (Comas-Basté et al., 2020). |
| Depression | This is a symptom of decreased mood and motivation caused by effects on the brain and neurotransmitters (Comas-Basté et al., 2020). |
Summary:
Histamine binds to various receptors throughout your body, triggering different responses like airway constriction, inflammation, or allergic reactions depending on the receptor type.
What Causes High Histamine Levels and How to Lower Them.
You may be curious about what makes histamine levels go up in the first place and what to do to lower them. Let’s explore some of the common causes and solutions for high histamine levels.
Allergies: The Most Common Cause of High Histamine Levels.
One of the most common causes of high histamine levels is allergies. When you’re allergic to something, your immune system sees it as a threat and releases histamine to fight it off. The immune system for example does not recognize pollen as a dead plant molecule, it does not know what it is, so it might be a foreign invader and there is an immune response that follows.
But allergies are not the only reason why the body may release histamine. Sometimes, the body may react to non-allergic triggers like stress, temperature changes, or hormonal fluctuations. These can also cause release and trigger similar symptoms.
Medications: How They Can Interfere with Your Histamine Metabolism.
Another factor that can affect histamine levels is the medications you take. Some medications or supplements that can interfere with your histamine metabolism are:
- Antihistamines: These are drugs that block histamine receptors and reduce the effects of histamine in your body. They are commonly used to treat allergies, motion sickness, insomnia, and nausea. However, they can also have some side effects, such as drowsiness, dry mouth, blurred vision, difficulty urinating, and increased appetite. Some antihistamines can also interact with other drugs, such as antidepressants, alcohol, or sedatives, and increase the risk of drowsiness or impaired coordination. You should consult your doctor before taking antihistamines if you have any medical conditions or are taking any other medications.
- DAO inhibitors: These are drugs that inhibit the enzyme diamine oxidase (DAO), which is responsible for breaking down histamine in your body. They include some antidepressants, antipsychotics, antibiotics, painkillers, anti-inflammatory drugs, and blood pressure drugs. By inhibiting DAO, these drugs can increase your histamine levels and cause symptoms of histamine intolerance, such as headaches, nasal congestion, hives, digestive issues, and irregular heart rate. You should avoid taking these drugs if you have histamine intolerance or low DAO levels. You should also check with your doctor before taking any new medications or supplements that may affect your DAO activity.
- Histamine liberators: These are substances that can trigger the release of histamine from mast cells or basophils in your body. They include some foods, such as alcohol, aged cheese, vinegar, pickles, and cured meats; some additives, such as sulfites, benzoates, and tartrazine; and some drugs, such as morphine, tubocurarine, and dextran. By releasing histamine, these substances can cause allergic reactions or worsen histamine intolerance symptoms. You should avoid or limit these substances if you have high histamine levels or histamine intolerance. You should also be aware of the potential interactions between these substances and antihistamines or DAO inhibitors.
Some of the medications that can interfere with DAO include:
- Antidepressants
- Antihistamines
- Antibiotics
- Painkillers
- Anti-inflammatory drugs
- Blood pressure drugs
If you take any of these medications regularly, you may want to talk to your doctor about alternative options or ways to support your DAO levels.
Summary:
Medications like antihistamines, DAO inhibitors, and histamine liberators can impact your histamine levels, potentially causing side effects or worsening symptoms.
Gastrointestinal Disorders: How They Can Affect Your Histamine Levels.
Gut health can also influence histamine levels. The gut is home to trillions of bacteria that help us digest food, produce vitamins and hormones and protect us from infections. But sometimes, these bacteria can get out of balance and cause problems.
One of the problems that can arise from a dysbiotic gut is high histamine levels. Some gut bacteria produce histamine as part of their metabolism. If you have too many of these bacteria in your gut, they can flood your body with histamine and cause symptoms like bloating, gas, diarrhea, or constipation.
Researchers found that in mice, bacteria that make histamine in the gut caused an immune reaction in the lung (Barcik et al., 2019). This implies that gut histamine may affect other parts of the body as well, but more studies in humans are needed.
Another problem that can affect histamine levels is a leaky gut syndrome. This is a condition where the lining of the intestines becomes damaged due to inflammation or some other factors and allows toxins, bacteria, and undigested food particles to enter the bloodstream. This can trigger inflammation in the rest of the body and immune reactions that can increase histamine production.
Other gastrointestinal disorders that can impact your histamine levels include:
- SIBO: Small intestinal bacterial overgrowth is a condition where too many bacteria grow in your small intestine and cause digestive issues.
- Gluten intolerance: Gluten is a protein found in wheat and other grains that some people cannot digest properly. It can cause inflammation and damage to your gut lining.
- IBS: Irritable bowel syndrome is a disorder that affects the movement of your intestines and causes abdominal pain, cramping, diarrhea, or constipation (Böhn et al., 2013).
- Inflammatory bowel disease: This is a group of conditions that cause chronic inflammation and ulcers in your digestive tract.
- Food allergies: Sometimes people might have unregistered food allergies or allergies that are not severe enough but still are present to create chronic inflammation in the gastrointestinal tract. You might want to do a full spectrum analysis of food allergy tests.
If any of these conditions sound familiar, you may want to talk to a gastroenterologist. This is very common in people that have chronic inflammation due to the standard American diet that lacks both fiber and antioxidants and is overloaded with meat and animal products that feed non-probiotic meat putrefying bacteria in the colon where meat ferments for more than a day in human digestion. In carnivores species for this specific reason, the colon is very short, there is no fermentation, and transit time is measured in hours. Functional medicine practitioners can help you fix your gut and reduce your histamine levels but you will have to change your diet.
Summary:
Gut issues like dysbiosis, leaky gut, and various disorders can contribute to high histamine levels, causing digestive symptoms and potentially affecting other organs. Addressing gut health through diet changes and consulting a specialist might be crucial to managing histamine levels.
Histamine-Rich Foods: How They Can Trigger Histamine Release in Your Body.
The last thing that affects your levels is the food you eat. Some foods have a lot of it or can make your body release more of it.
If you have high levels or full-blown histamine intolerance, you may want to stay away from or cut down on these foods and see if you feel better. You may also want to eat more foods that are low in histamine or help bring down the levels in your body.
Genetics: How They Can Predispose You to High Histamine Levels.
Sometimes, high levels are not caused by external factors like allergies, medications, or food. Sometimes, they are caused by internal factors like genes. Genes are the blueprint that determines how we produce and break down histamine.
There are two genes that are particularly important for your histamine metabolism: AOC1 and MTHFR. These genes code for enzymes that help us regulate histamine levels. But sometimes, these genes can have mutations that affect their function.
AOC1: The Gene That Breaks Down Histamine.
One of the genes that can affect your histamine levels is AOC1 known as the DAO gene. This gene produces an enzyme called diamine oxidase (DAO). DAO is responsible for breaking down histamine. It acts like scissors that cut histamine molecules into smaller pieces that can be easily eliminated.
But what if your scissors are dull or broken? What if you have a mutation in the AOC1 gene that lowers DAO levels? Then you may not be able to break down histamine properly and end up with excess levels in your system. This can lead to a condition called histamine intolerance.
Histamine intolerance is a condition where your body cannot tolerate normal amounts of histamine and reacts with symptoms like headaches, nasal congestion, fatigue, hives, digestive issues, irregular menstrual cycle, nausea, and vomiting. In severe cases, you may also have abdominal cramping, tissue swelling, high blood pressure, irregular heart rate, anxiety, difficulty regulating body temperature, and dizziness.
If you have histamine intolerance or suspect that you do, you may want to get tested for the AOC1 gene mutation or take supplements that contain DAO or help boost its production.
Summary:
AOC1, the DAO gene, plays a crucial role in breaking down histamine in your body. A mutation in this gene can lead to histamine intolerance, causing various symptoms like headaches, fatigue, and digestive issues. Testing for the AOC1 mutation or taking DAO supplements can help manage histamine levels.
MTHFR: The Gene That Regulates Histamine Production.
Another gene that can affect your levels is MTHFR. This gene affects the methylation cycle in your body. Methylation is a process that helps regulate histamine production and degradation. It also helps with many other functions like DNA repair, detoxification, and neurotransmitter synthesis.
Methylation works like a switch that turns on or off certain genes or enzymes in your body. It does this by adding or removing a small chemical group called a methyl group to different molecules. This changes their shape and function
But what if your switch is faulty? What if you have a mutation in the MTHFR gene that impairs your methylation? Then you may have trouble regulating your levels.
If you have impaired methylation and higher levels, you may experience symptoms like mood swings, depression, anxiety, insomnia, allergies, asthma, or eczema. You may also have an increased risk of cardiovascular disease, cancer, or neurological disorders.
If you have impaired methylation or suspect that you do, you may want to get tested for the MTHFR gene mutation or take supplements that support methylation like folate (B9), B12, or SAMe.
Summary:
The MTHFR gene, crucial for methylation, regulates histamine, influencing mood, sleep, allergies, and various disorders. Consider testing for gene variations and supporting methylation through supplements if needed.
Histamine Intolerance Symptoms
| Symptoms | Explanation | Mode of action |
| Migraine headaches | Severe throbbing pain in one or both sides of the head, often accompanied by nausea, vomiting, and sensitivity to light and sound. | It can dilate blood vessels in the brain and cause inflammation and pain (Wantke et al.,1993). |
| Digestive symptoms, such as diarrhea | Loose and watery stools that occur more than three times a day. | It can stimulate the production of stomach acid and increase intestinal motility, leading to digestive discomfort and diarrhea. |
| Flushed skin | Redness and warmth of the skin, especially on the face, neck, and chest. | It can cause blood vessels to dilate and increase blood flow to the skin, resulting in flushing. |
| Hives or an itchy skin rash | Raised, red, and itchy bumps or patches on the skin that can vary in size and shape. | It can activate mast cells in the skin and cause them to release more histamine and other inflammatory substances that cause itching and swelling (Son et al., 2018). |
| Worsening eczema | A chronic condition that causes dry, itchy, and inflamed skin that can crack and bleed. | Histamine can worsen eczema by increasing inflammation and itching in the skin (Maintz et al., 2006). |
| Congested, runny, or itchy nose | A blocked or dripping nose that may be accompanied by sneezing and itching. | It can stimulate nerve endings in the nose and cause mucus production and nasal inflammation. |
| Red, itchy, or watery eyes | Irritation and inflammation of the eyes that may cause tearing and burning sensations. | Histamine can activate mast cells in the eyes and cause them to release more of it and other inflammatory substances that cause itching and swelling. |
Some of the less common but more serious symptoms are:
| Symptoms | Explanation | Possible triggers |
| Abdominal cramping | Painful contractions or spasms of the abdominal muscles. | It can cause smooth muscle contraction in the gut and increase intestinal motility, leading to cramping and diarrhea. |
| Tissue swelling | Swelling or edema of the skin or mucous membranes, such as the lips, tongue, throat, or eyelids. | It can cause blood vessels to become leaky and allow fluid to accumulate in the tissues, causing swelling and inflammation (King et al., 2000). |
| High blood pressure | A condition where the force of blood against the artery walls is too high, usually above 130/80 mm Hg. | It can cause blood vessels to constrict and increase blood pressure. Foods high in histamine or that release histamine, such as alcohol, cheese, vinegar, pickles, and cured meats. |
| Irregular heart rate | A condition where the heart beats too fast, too slow, or irregularly. | It can affect the electrical activity of the heart and cause arrhythmias or palpitations. |
| Anxiety | A feeling of nervousness, worry, or fear that interferes with daily life. | It can act as a neurotransmitter and affect mood and cognition. |
| Dizziness | A sensation of lightheadedness, faintness, or unsteadiness. | It can cause blood pressure to drop suddenly and reduce blood flow to the brain, causing dizziness. |
How to Find Out If You Have Histamine Intolerance.
Allergy vs. Intolerance
Intolerance means that your body can’t break down or handle food or a chemical. An allergy means that your body’s immune system sees and fights an allergen.
Do you suffer from headaches, hives, stuffy nose, or stomach problems after eating certain foods? If so, you might have histamine intolerance.
Normally, the body can handle a certain amount of histamine without any problems. But sometimes, too much can build up and cause symptoms like itching, sneezing, hives, headaches, and digestive issues. This is called histamine intolerance.
There is no standardized or validated test for intolerance, and the symptoms are often nonspecific and overlap with other conditions. Therefore, the diagnosis of histamine intolerance may be underreported or overdiagnosed (Comas-Basté et al., 2020). Some people may have mutations in the genes that code for the enzymes that can increase the risk of intolerance. The frequency of these mutations may differ among different populations or ethnic groups (Comas-Basté et al., 2020). Dietary habits may increase the levels and cause symptoms of intolerance in some people. The dietary intake of these foods may vary depending on cultural, geographical, or personal preferences (Comas-Basté et al., 2020).
As a general rule, intolerance is not very common, and it affects more women than men. Only about 1% of the entire population has this condition and we are talking about full-blown intolerance (Maintz & Novak, 2007). This still doesn’t mean that you do not have some sort of sensitivity that is not on a clinical scale especially if you have dysregulated microbiome. Most of the patients that have intolerance are middle-aged women. Women mostly suffer from this condition and one possible reason is that female hormones play a role in how much of it the body produces and releases.
Estrogen and progesterone are two hormones that regulate many functions. They also affect how your mast cells behave. Mast cells are the cells that store and release histamine when they sense something harmful or irritating in your tissues. Estrogen makes mast cells release histamine, while progesterone inhibits it (Jing et al., 2012), (Vasiadi et al., 2006).
So, if you have more estrogen than progesterone, you may end up with more histamine than you can handle. This usually happens in situations when hormones change. Hormonal fluctuations happen during some parts of your menstrual cycle, during pregnancy, or during menopause.
It can also happen if you take certain medications or supplements that affect hormone levels.
But how can you tell if you have histamine intolerance? Unfortunately, there is no easy or definitive way to diagnose it. The only way to confirm intolerance with certainty is to do an oral challenge test, which involves eating a histamine-free diet for four weeks and then reintroducing high-histamine foods to see if symptoms occur. Other tests that measure histamine levels or DAO activity in the blood are not accurate or consistent enough to diagnose this condition. Regardless, there are some methods that can give you some clues. Let’s take a look at them.
Summary:
Histamine intolerance, affecting roughly 1% of the population, causes allergic-like symptoms due to an inability to break down histamine. While diagnosis is complex, dietary adjustments and managing hormone fluctuations can be key to managing symptoms.
Measuring Your DAO Levels.
One of the methods is to measure the level or activity of diamine oxidase (DAO) in the blood. If you have low DAO levels, it could mean that you have intolerance (Mušič et al., 2013).
However, this method is not very reliable or accurate. That’s because your DAO levels can change depending on many things, such as the medicines you take, the health of your gut, or your genes. Also, having low DAO levels does not necessarily mean that you have too much histamine in your body or that you can’t handle it well.
Doing a Prick Test.
Another way to test for intolerance is to prick your skin with a 1 percent histamine solution. This is like an allergy test. The idea is that if you have histamine intolerance, your skin will react more to the prick test than normal. According to one study, a skin prick test that tracks how fast the reaction goes away was able to correctly identify histamine intolerance in 79% of cases and rule it out in 81% of cases (Kofler et al., 2011). But this way is still considered to be not very accurate or specific. That’s because your skin reaction can change depending on other things, such as antihistamines or other drugs that you may be taking.
Following an Elimination Diet.
The third method is to follow an elimination diet where you avoid foods that are high in histamine or trigger its release for a few weeks. Then you reintroduce them one by one and see if your symptoms come back.
This method can be helpful to identify which foods cause you problems and how much of them you can tolerate. However, it can also be hard to do and may not be enough to diagnose intolerance. That’s because there are many other things that can affect your symptoms besides food, such as stress, infections, or environmental allergens.
Consulting with a Doctor or an Allergist.
As you can see, none of these methods are perfect or conclusive for diagnosing histamine intolerance. That’s why it is important to talk to a doctor or an allergist before trying any of them. They can help you rule out other possible causes of your symptoms and advise you on the best way to manage them for your individual case.
Intolerance can be tricky to deal with, but it doesn’t have to ruin your life. With the right guidance and support, you can find out what works for you and enjoy food without fear.
How to Lower Your Histamine Levels.
Here are some tips to help you reduce histamine levels:
1) Identify and avoid your triggers: The first step is to figure out what causes high histamine levels in your case. It could be allergies, medications, gut issues, or food sensitivities. You may want to keep a journal of what you eat and how you feel or do some tests with the help of a doctor or nutritionist.
2) Support your DAO levels: The next step is to support your DAO levels by taking supplements or eating foods that contain DAO or help boost its production. Some examples are vitamin C, vitamin B6, zinc, copper, magnesium, and quercetin.
3) Heal your gut: The third step is to heal your gut by correcting microbiome composition and lowering inflammation in the gastrointestinal tract. Taking probiotics is beneficial but to a limited extent. Most efficient is to take prebiotics because if you feed meat putrifying bacteria no amount of probiotics will help. This is a vast subject but by general rule, fiber needs to increase, antioxidant consumption needs to increase, learn your ORAC values, toxicity exposure needs to decrease, and all non-probiotic foods need to decrease meaning meat and animal products. You may also want to take digestive enzymes or eat foods that contain them like pineapple or papaya to help break down food better. Studies have found that people with this condition have lower levels of beneficial Bifidobacteria, that feed on sugar (degrade hexose sugars through a particular metabolic pathway, termed the “bifid shunt”,) and instead have higher levels of harmful Proteobacteria, and also have less variety of microbes in their guts than healthy individuals (Schink et al, 2018). Proteobacteria include a wide variety of pathogens, such as Escherichia, Salmonella, Vibrio, Helicobacter, and others and all of them are non-probiotic and are able to eat meat or ie. metabolize protein as well as lipids.
4) Reduce inflammation: The fourth step is to reduce inflammation by eating anti-inflammatory foods high in antioxidants and taking supplemental antioxidants like turmeric, spices, astaxanthin, and essential oils. You may also want to avoid inflammatory foods like sugar, meat, dairy, fish, and processed foods.
5) Manage stress: The last step is to manage stress by optimizing stress hormone levels like cortisol, avoiding stimulants like coffee or nicotine, avoiding alcohol and other psychoactive substances and exercising, sauna, going to nature, and practicing relaxation techniques like meditation, yoga, breathing exercises or massage therapy. Stress can trigger histamine release and worsen your symptoms so it’s important to find healthy ways to cope with it.
6) Antihistamines: If everything else fails you can always take oral antihistamine medicine prescribed to you by your Allergist.
Elimination diet.
To implement an elimination diet, you need to follow these general steps:
- Choose which foods or food groups you want to eliminate based on your symptoms and suspected triggers. You can use a food diary to track what you eat and how you feel for a few weeks before starting the diet.
- Remove all the foods or food groups you have chosen from your diet for a period of 2–3 weeks, or longer if needed. Make sure to read food labels carefully and avoid any hidden sources of the foods you are eliminating.
- Eat only foods that are low in histamine or unlikely to cause reactions, such as fresh meat, fresh fruit (except citrus and plantains), fresh vegetables (except tomato, eggplant, and spinach), rice, coconut milk, herbal tea, olive oil, garlic, and herbs.
- After the elimination period, reintroduce one food or food group at a time, every 2–3 days, and monitor your symptoms. Start with small amounts and gradually increase them as tolerated. If you notice any adverse reactions, such as rashes, headaches, bloating, or diarrhea, stop eating that food and wait until your symptoms subside before reintroducing another food.
- Repeat this process until you have tested all the foods or food groups you have eliminated. You may find that some foods cause mild symptoms that you can tolerate occasionally, while others cause severe symptoms that you need to avoid completely.
- Once you have identified your trigger foods, you can create a personalized diet plan that excludes them and includes foods that are safe and nutritious for you. You may also consult with a doctor or a nutritionist for guidance and support.
Some practical tips and strategies to help you implement an elimination diet are:
- Plan your meals and snacks ahead of time and prepare them at home as much as possible.
- Use a food diary or an app to record what you eat and how you feel during the elimination and reintroduction phases.
- Choose simple recipes that use few ingredients and avoid sauces, dressings, marinades, and spices that may contain hidden sources of the foods you are eliminating.
- Shop for fresh and unprocessed foods and avoid packaged and processed foods that may have additives or preservatives that can trigger reactions.
- Read food labels carefully and look for allergen warnings or ingredient lists that indicate the presence of the foods you are eliminating.
- Inform your family, friends, co-workers, and healthcare providers about your elimination diet and ask for their support and understanding.
- If you eat out or travel, be cautious about what you order and ask questions about how the food is prepared and what ingredients are used. You may also bring your own food or snacks if needed.
Summary:
Summary:
An elimination diet involves removing foods that may cause symptoms for a period of time and then reintroducing them one by one to identify your triggers. To implement an elimination diet successfully, you need to plan ahead, keep track of what you eat and how you feel, avoid hidden sources of the foods you are eliminating, and seek professional advice if needed.
Support your DAO levels.
| Nutrient | Foods that can boost DAO levels | Benefits of nutrient |
| Omega-3 | Algae-based DHA supplement, flaxseeds, chia seeds, walnuts | Omega-3 has been shown to release DAO and improve histamine breakdown |
| Phosphorus | Almonds, broccoli, white beans | Phosphorus is a mineral that helps form the structure of DAO. DAO contains a cofactor called pyridoxal 5′-phosphate (PLP), which is derived from vitamin B6. PLP binds to a lysine residue in the active site of DAO and forms a Schiff base with histamine, facilitating its oxidation. Phosphorus is involved in the synthesis of PLP and the stabilization of its structure. |
| Calcium | Dark leafy greens, poppy seeds, sesame seeds, beans | Calcium is a cofactor for DAO activity and may enhance its function |
| Zinc | Pumpkin seeds, almonds, lentils, spinach | Zinc is another cofactor for DAO activity and may improve its stability |
| Magnesium | Dark leafy greens, cocoa or dark chocolate | Magnesium is also a cofactor for DAO activity and may increase its efficiency |
| Vitamin B12 | Supplement, fortified foods or meat and animal products | Vitamin B12 is involved in the metabolism of histamine and may help lower its levels |
| Iron | Iron is essential for the synthesis of DAO and may regulate its expression |
There are oral DAO supplements available. DAO enzymes are supplements that mimic the action of the natural DAO produced by your gut cells. They are supposed to provide extra DAO enzymes to help break down histamine from foods you eat, so less of it gets into your bloodstream and prevent or reduce symptoms of intolerance and there is some evidence that this approach might be helpful (Schnedl et al, 2019). They are sold as supplements but my suggestion is to visit Allergist before taking any DAO supplements.
Some people may benefit from taking DAO enzymes before meals, especially if they have low DAO activity in their gut. However, the research on DAO supplements is still limited and not very conclusive. Schnedl et al, (2019), challenged the previous assumption that DAO enzymes cannot be absorbed from the gut into the blood. There was a slight increase in blood DAO levels after taking the supplements orally. The study showed that taking 0.3mg of DAO before each meal for a month significantly reduced all symptoms of histamine intolerance in 14 participants. But when they stopped taking the supplements, their symptoms came back. Few other studies have suggested that DAO supplements may improve some symptoms of intolerance, such as hives (Yacoub et al., 2018) and migraines (Izquierdo-Casas et al, 2019).
More research is needed to confirm the safety and effectiveness of DAO supplements for histamine intolerance.
Some practical tips for taking DAO supplements are:
- Take it before meals that contain high-histamine foods or trigger histamine release.
- Follow the dosage instructions on the label or as prescribed by your healthcare provider.
- Store it in a cool and dry place away from direct sunlight.
- Keep track of your symptoms and report any changes to your healthcare provider.
Some limitations of DAO supplements are:
- It may not work for everyone or for all symptoms of intolerance.
- It may interact with certain medications or supplements that affect histamine levels or DAO activity.
- It may cause side effects such as headache, nausea, diarrhea, or allergic reactions in some people.
- It may not address the underlying causes of intolerance or DAO deficiency.
Summary:
DAO enzyme supplements show promise for managing some histamine intolerance symptoms like hives and migraines, but more research is needed to confirm their effectiveness and safety. Consult an allergist before taking them.
How to Boost Your DAO Activity with Vitamins and Minerals.
You may have heard that DAO is the enzyme that helps your body get rid of excess histamine. But did you know that some vitamins and minerals can also help your DAO work better? That’s right, some nutrients can either increase the amount of DAO in your blood or help it break down histamine faster. Let’s take a look at what they are and how they work.
Vitamin B6: The DAO Booster.
Vitamin B6 is like fuel for your DAO. It helps your body produce more DAO and keep it active. Some studies have found that people who don’t get enough vitamin B6 have lower levels of DAO in their blood (Martner-Hewes et al., 1986). This means they may be more prone to histamine intolerance and its symptoms.
So how can you get more vitamin B6 in your diet? Some good sources are nuts, seeds, beans, and whole grains. You can also take a vitamin B6 supplement if your doctor recommends it.
Vitamin C: The Histamine Destroyer.
Vitamin C is not only good for your immune system and skin health. It can also help you lower your levels by literally destroying histamine molecules in the blood (Johnston, 1996). One study showed that giving vitamin C by IV to people with allergies reduced their levels significantly (Hagel et al., 2013).
Vitamin C is easy to find in many fruits and vegetables. Some of the best sources are citrus fruits, berries, kiwis, peppers, broccoli, and kale. You can also take a vitamin C supplement if you need extra support.
Copper: The Histamine Blocker.
Copper is a mineral that may have a surprising effect on histamine. It may actually stop histamine from being released from your mast cells (Sharma & Jande, 1989). Mast cells are the cells that store histamine and release it when they sense an allergen or an irritant. One study found that adding copper to mast cells in a test tube prevented them from releasing histamine.
Some of the best sources of copper are dark chocolate, nuts, seeds, and mushrooms.
Title
While DAO enzymes help combat histamine, boosting levels with vitamins B6 and C and incorporating copper-rich foods can also improve histamine tolerance.
How to Choose the Right Probiotics for Histamine Intolerance.
A healthy gut is essential for overall well-being and disease prevention, not just for histamine intolerance. But if you have an intolerance, you may find it hard to balance your gut bacteria because many of the foods that contain good bacteria (probiotics) are also high in histamine. Think yogurt, kefir, kombucha, and so on. These foods can trigger or worsen your intolerance symptoms.
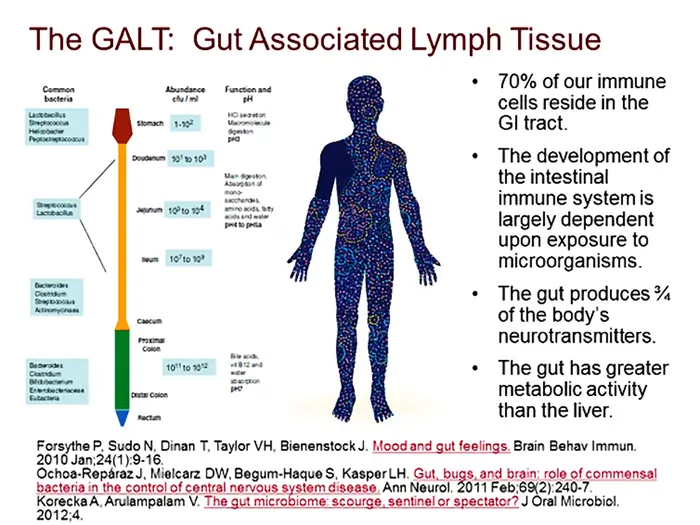
Most people go with the option to take probiotic supplements. This will generally not help to the full extent if you keep feeding flesh-eating non-probiotic bacteria by consuming animal products. There are only two types of bacteria. The bacteria are very specialized in what they eat. They metabolize only one thing. There are thousands of different bacteria but only two main groups. Fiber and sugar fermenting ones that do not attack our flesh and are considered probiotic and meat-eating flesh-putrefying bacteria that are considered non-probiotic because our flesh is tasty too. This creates inflammation and most of our immune system is designed to deal with this type of bacteria. More than 70 percent of lymph nodes are in the gut, a network known as gut-associated lymphoid tissue or GALT.
You will first need to change your diet and if you opt for probiotic supplements not all of them are the same either. Some of them can actually produce histamine in your gut and make things worse. Others can help break down or lower histamine and make things better.
Summary:
Choosing probiotics for histamine intolerance requires caution: avoid histamine-producing strains and focus on those that break down histamine, like Lactobacillus plantarum and Bifidobacterium longum. Prioritize dietary changes over supplements, as animal products feed histamine-producing bacteria.
Probiotic Strains to Look For.
If you want to take probiotic supplements you need to be careful about which strains you choose. Here are some of the strains that may be beneficial for you because they can degrade or reduce histamine in your gut:
Lactobacillus plantarum (Capozzi et al., 2012); Lactobacillus rhamnosus (Forsythe et al., 2012), (Oksaharju et al., 2011); Bifidobacterium infantis (Dev et al., 2008); Bifidobacterium lactis (Mokhtar et al., 2012); Bifidobacterium longum (Dev et al., 2008).
Probiotic Strains to Avoid.
On the other hand, here are some of the strains that may be harmful to you because they can produce histamine in your gut:
Lactobacillus brevis (Rai et al., 2014); Lactobacillus casei (Priyadarshani & Rakshit, 2011), (Herrero-Fresno et al., 2012); Lactobacillus delbrueckii (Priyadarshani & Rakshit, 2011); Lactobacillus fermentum (Stratton et al., 1992); Lactobacillus helveticus (Stratton et al., 1992); Lactobacillus hilgardii (Rai et al., 2014); Lactobacillus lactis (Stratton et al., 1992); Enterococcus faecium (Stratton et al., 1992); Streptococcus thermophilus (Gezginc et al., 2013), (Rossi et al., 2011).
Summary:
Probiotics can be one way to support your gut health and immune system. However, if you have histamine intolerance, you need to be selective about which ones you take. Some probiotics can help you lower your levels and ease your symptoms while others can do the opposite. Use the lists above as a guide when shopping for probiotic supplements and always consult your doctor before starting any new supplement regimen.
How Cooking Methods Affect Histamine Levels in Foods.
The way the food is cooked can also make a difference.
In this study (Chung et al., 2017), they wanted to find out how different cooking methods influence the histamine levels in foods. They have chosen some common foods that people eat often and cooked them by grilling, boiling, and frying. Then they measured the level in each food using a special test.
Here are the main findings of the study:
- Grilling seafood made it have more histamine than raw or boiled seafood. This means that grilled seafood may be more likely to cause histamine-related problems for some people.
- For meat, grilling also increased the level, while boiling decreased it. This suggests that boiling meat may be a safer option for people who are sensitive.
- For eggs, the cooking method didn’t affect the level much. This means that eggs are not a major source of histamine in food.
- Frying vegetables made them have more than raw vegetables. This implies that fried vegetables may trigger histamine reactions more easily than raw ones.
- Fermented foods didn’t change much in level after being boiled. This indicates that boiling fermented foods doesn’t reduce their histamine content.
This study shows that cooking methods can change the histamine level in foods. Frying and grilling tend to increase the levels while boiling has little effect or even lowers them.
Summary:
Cooking methods matter for histamine levels: Frying and grilling generally raise them while boiling often reduces them. Opt for boiling to minimize histamine if you have intolerance or allergies.
How to Eat Low Histamine for Better Health.
One way to manage histamine intolerance is to follow a low histamine diet. This means avoiding foods that are high in histamine or that can trigger its release. By doing so, you can reduce your symptoms and improve your quality of life.
Tips for a Low Histamine Diet.
A low histamine diet is not a one-size-fits-all approach. Some people may be more sensitive to certain foods than others. Some people may need to avoid more foods than others. Some people may need to follow a low histamine diet for a short time, while others may need to follow it for longer.
That’s why it’s important to consult with a nutrition professional who can guide you through this process. They can help you identify your triggers, plan your meals, monitor your progress, and adjust your diet as needed.
But in general, here are some tips that can help you eat low histamine:
- Eat fresh foods as much as possible. Fresh foods have less than aged, fermented, or processed foods. For example, fresh meat has less histamine than cured meat, fresh cheese has less than aged cheese, and fresh fruit has less than dried fruit.
- Avoid foods that are known to be high in histamine or that can trigger its release. I’ll give you a list of these foods later in this article.
- Eat foods that have natural antihistamines. These are substances that can help lower the amount of histamine in your body or block its effects. Some examples are vitamin C-rich foods (berries, kiwi, broccoli), vitamin D-rich foods (mushrooms, fortified dairy), quercetin-rich foods (apples, onions, green tea), bromelain-rich foods (pineapple) and curcumin-rich foods (turmeric).
- Drink plenty of water. Water helps flush out excess histamine from your body and keeps you hydrated.
- Use fresh herbs and spices for seasoning. Avoid vinegar, soy sauce, ketchup, and mustard.
- Keep a food diary. A food diary can help you track what you eat and how you feel after each meal. This can help you identify patterns and correlations between your food intake and your symptoms. You can also share your food diary with your nutrition professional or healthcare provider for further guidance.
Don’t think of a low histamine diet as a magic bullet for intolerance. It can help you feel better and reduce your discomfort, but it won’t fix the root problem. That’s why you should always talk to your doctor and find out what’s really causing your symptoms. They can give you the right diagnosis and treatment to make sure you’re on the right track.
Summary:
Manage histamine intolerance by prioritizing fresh, low-histamine foods, avoiding triggers like cured meats and fermented items, and incorporating natural antihistamines like vitamin C and quercetin. Consult a nutritionist for personalized guidance and remember, a low-histamine diet can alleviate symptoms but isn’t a sole solution.
Foods to Avoid on a Low Histamine Diet.
Now that you know some tips for a low histamine diet, let’s talk about what foods to avoid on this diet. You may have seen some tables or charts online that show the histamine levels of different foods. But the truth is that these data are not very reliable or consistent. They may vary depending on the source, quality, freshness, storage, and preparation of the food. So instead of relying on these tables or charts, I suggest you follow some general guidelines on which foods are likely to be high or trigger its release.
These guidelines are based on the available information from scientific studies and reputable sources.
But keep in mind that these are not absolute rules. You may find that some foods affect you more than others or not at all. You may also find that some foods are fine in small amounts but not in large amounts.
So listen to your body and use these guidelines as a starting point for your low histamine diet.
Some examples of foods that are typically considered high in histamine are:
- Smoked, cured, and aged meats such as bacon, sausage, and salami
- Canned fish, smoked fish, and aged cheeses
- Sauerkraut and other fermented products
- Spinach, eggplant, tomato, and avocado
- Wine, beer, alcohol, coffee, tea, and chocolate
- Citrus fruits, dried fruits, strawberries, bananas, papaya and pineapple
- Nuts, peanuts, cashews, and walnuts
- Soy products, tofu, and tempeh
- Vinegar, soy sauce, ketchup, and mustard
- Yeast and yeast-containing foods such as bread, pizza, and beer
- Shellfish, mussels, and shrimp
- Mushrooms and truffles
- Olives and pickles
- Cinnamon, cloves, nutmeg, and curry powder
- Asparagus, artichokes, and broccoli
- Citrus fruits, dried fruits, strawberries, bananas, papaya and pineapple
- Nuts, peanuts, cashews, and walnuts
- Soy products, tofu, and tempeh
- Vinegar, soy sauce, ketchup, and mustard
- Yeast and yeast-containing foods such as bread, pizza, and beer
- Shellfish, mussels, and shrimp
- Mushrooms and truffles
- Olives and pickles
- Cinnamon, cloves, nutmeg, and curry powder
- Asparagus, artichokes, and broccoli
Some examples of foods that are typically considered low in histamine are:
- Fresh vegetables and fruits (except for citrus fruits, dried fruits, tomatoes, spinach, and avocado)
- Fresh meat, poultry, fish, and eggs
- Gluten-free grains such as rice, quinoa, millet, and buckwheat
- Water, herbal teas, and non-citrus juices
- Fresh herbs and spices
- Foods that have natural antihistamines, such as vitamin C-rich foods (berries, kiwi, broccoli), vitamin D-rich foods (mushrooms, fortified dairy), quercetin-rich foods (apples, onions, green tea), bromelain-rich foods (pineapple) and curcumin-rich foods (turmeric)
- Fresh or frozen berries, such as blueberries, raspberries, blackberries, and cranberries
- Fresh or frozen cherries, grapes, pears, and melons
- Fresh or frozen green beans, peas, carrots, celery, and lettuce
- Fresh or frozen corn, potatoes, sweet potatoes, and squash
- Rice milk, almond milk, and coconut milk
- Rice cakes, corn cakes, and gluten-free crackers
- Olive oil, coconut oil, and ghee
- Honey, maple syrup, and molasses
In this study (Teresa et al., 2021) they did a complete analysis of the available literature on histamine avoidance diets. Different sources have different opinions on what foods have high levels. In the study, they looked at various low histamine diets and compared them to see what they have in common and what they disagree on. Figure 1 shows the results of their analysis. You can see that some foods are avoided by all the diets, such as fermented foods and drinks like salami, cheese, wine, and beer. But most foods are only avoided by some of the diets, not all of them. This shows how much confusion there is about what foods are safe for histamine-intolerant people. We need more research and evidence on this topic.
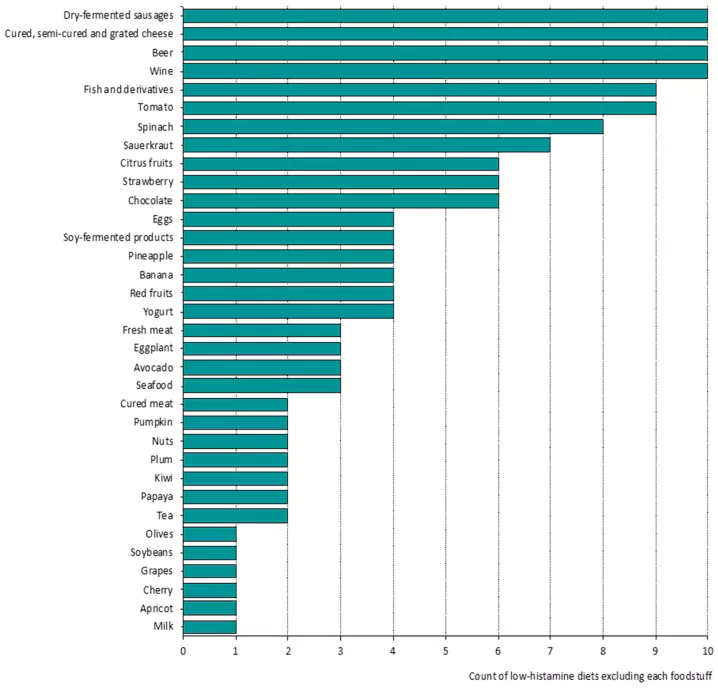
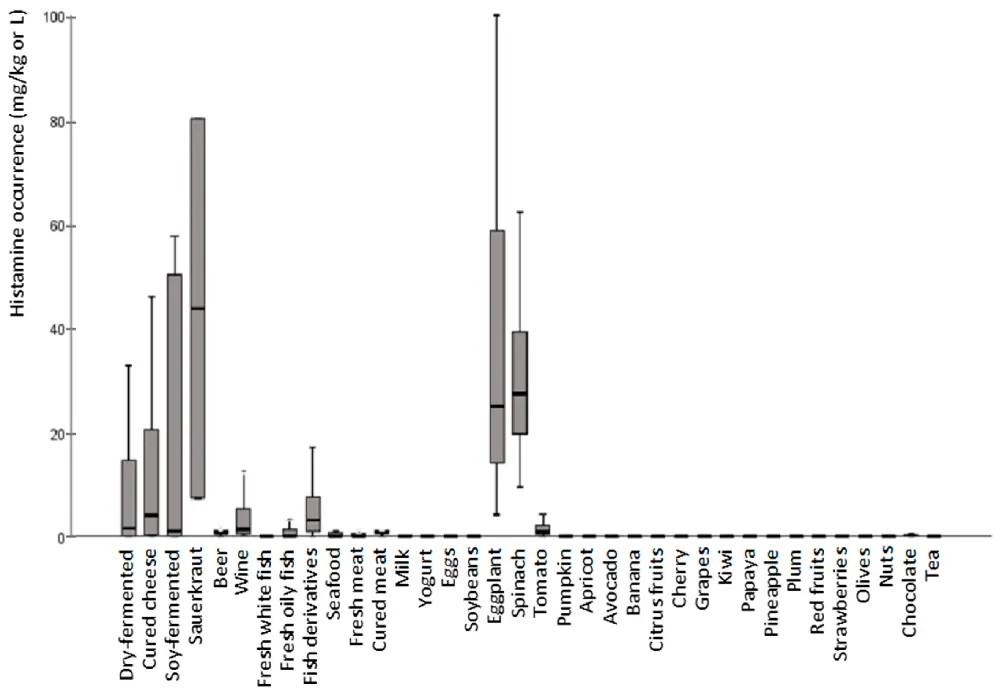
How much is in the foods that are excluded by low histamine diets? Figure 2 shows the answer. You might be surprised to see that most of the foods have very low histamine levels, less than 1 mg/kg. Some experts say that this is the limit for a food to be considered low in histamine. So why are these foods banned by some diets? The reason is that fermented foods are tricky. They can have very different levels depending on how they are made and stored. Histamine is produced by bacteria, and bacteria can grow and change depending on many factors. This makes it hard to predict how much of it is in fermented food. To be safe, some diets avoid all fermented foods, even if they might not have much histamine. But this might not be necessary for everyone.
Fermented Foods.
You might love cheese, sausages, sauerkraut, and soy sauce, but did you know that these are all fermented foods? That means they are made by bacteria that change the original ingredients into something new and tasty.
But there is a downside: some of these bacteria can also make histamine and other chemicals called biogenic amines.
These can cause problems for some people who are sensitive to them. Figure 2 shows how much histamine is in different fermented foods sold in Spain. You can see that most of them have low levels, between 22 and 74 mg/kg on average. But some of them can have much more, up to 203 mg/kg in cheese, 130 mg/kg in sausages, and 486 mg/kg in soy products. That’s a lot of histamine. And that’s not all: some fermented foods also have other biogenic amines, like tyramine, putrescine, and cadaverine. These can also cause headaches, nausea, and other symptoms. Table 1 shows the levels of these chemicals in different foods and drinks from Spain. You can see that tyramine is very common and high in some foods, especially cheese and fermented vegetables. Putrescine and cadaverine are also found in some foods but at lower levels. So if you have histamine intolerance or biogenic amine intolerance, you might want to be careful with fermented foods. They might taste good, but they might not make you feel good.
| Foods | n | Occurrence of Biogenic Amines (mg/kg or L) | |||||
| Histamine | Putrescine | Cadaverine | Tyramine | Spermidine | Spermine | ||
| Dry-fermented | 424 | 21.57 (52.10) | 68.23 (101.40) | 32.45 (72.96) | 140.9 (119.59) | 5.39 (5.94) | 25.12 (23.85) |
| sausages | 129.95 | 280.3 | 172.10 | 378.51 | 18.80 | 59.94 | |
| ND-474.82 | ND-537.05 | ND-658.05 | ND-742.60 | 3.04–32.65 | 0.34–224.15 | ||
| Cured, semi-cured | 80 | 33.10 (77.10) | 68.90 (141.30) | 87.25 (283.55) | 128 (264.41) | 8.49 (12.40) | 1.84 (4.46) |
| and | 203.30 | 423.00 | 356.52 | 613.46 | 36.38 | 12.58 | |
| grated cheese | ND-389.86 | ND-666.92 | ND-2036.90 | ND-1567.50 | ND-68.92 | ND-21.03 | |
| Soy-fermented | 21 | 73.95 (184.51) | 13.48 (6.71) | 6.88 (11.97) | 187.24 (446.59) | 34.84 (38.23) | 4.81 (5.24) |
| products | 486.31 | 22.2 | 35.08 | 930 | 105.47 | 11.15 | |
| ND-730.06 | 2.73–31.06 | ND-36.95 | ND-1730.17 | ND-124.03 | ND-21.89 | ||
| Sauerkraut | 5 | 43.74 (51.45) | 232.66 (148.53) | 76.49 (73.85) | 43.47 (28.05) | 5.29 (3.86) | 0.85 (0.40) |
| 76.48 | 327.18 | 123.49 | 61.32 | 7.75 | 1.10 | ||
| 7.36–80.12 | 127.63–337.68 | 24.27–128.71 | 23.63–63.3 | 2.56–8.02 | 0.56–1.13 | ||
| Beer | 176 | 1.23 (2.47) | 3.16 (2.89) | 1.28 (3.94) | 6.31 (8.04) | 0.48 (0.81) | 0.19 (0.61) |
| 3.28 | 7.61 | 4.66 | 25.44 | 1.7 | 1.14 | ||
| ND-21.60 | ND-14.50 | ND-31.40 | 0.55–46.80 | ND-6.30 | ND-3.90 | ||
| Wine | 299 | 3.63 (5.86) | ND | ND | 2.42 (2.47) | ND | ND |
| 12.3 | 7.5 | ||||||
| 0.09–34.25 | ND-15.85 | ||||||
| Fresh white fish | 31 | 1.14 (6.46) | 1.33 (2.67) | 1.61 (6.01) | 1.03 (3.39) | 2.25 (1.91) | 6.78 (2.65) |
| ND | 7.43 | 4.8 | 6.51 | 5.32 | 11.27 | ||
| ND-36.55 | ND-10.50 | ND-33.65 | ND-17.10 | ND-7.85 | 2.05–13.50 | ||
| Fresh oily fish | 49 | 3.27 (15.71) | 2.37 (6.71) | 13.22 (67.40) | 1.18 (5.43) | 6.69 (3.09) | 14.47 (9.75) |
| 6.66 | 5.02 | 10.45 | 2.19 | 11.39 | 31.67 | ||
| ND-111.26 | ND-39.89 | ND-400.23 | ND-37.20 | 1.20–11.90 | 1.05 -37.03 | ||
| Preserved and | 151 | 10.03 (53.32) | 2.79 (3.81) | 7.41 (10.79) | 8.23 (14.87) | 3.61 (2.78) | 7.48 (6.05) |
| semi-preserved | 20.39 | 9.02 | 29.23 | 40.6 | 7.94 | 17.05 | |
| fish | ND-657.05 | ND-21.15 | ND-55.80 | ND-88.50 | 0.37–11.80 | ND-35.20 | |
| Seafood | 7 | ND | 3.02 (3.01) | ND | 0.15 (0.27) | 4.03 (3.23) | 10.63 (6.92) |
| 7.62 | 0.58 | 7.94 | 19.21 | ||||
| 1.44–9.79 | ND-0.65 | 0.82–8.37 | 4.93–19.73 | ||||
| Fresh meat | 199 | ND | 1.35 (2.66) | 5.02 (14.55) | 4.32 (8.62) | 1.16 (4.59) | 17.08 (4.59) |
| 3.04 | 28.71 | 35.89 | 3.4 | 29.55 | |||
| ND-9.68 | ND-51.16 | ND-38.77 | ND-13.96 | 9.70–25.69 | |||
| Cured meat | 23 | 4.89 (22.70) | 4.65 (5.18) | 38.03 (92.82) | 3.43 (10.56) | 6.05 (0.92) | 37.82 (10.46) |
| 3.54 | 9.24 | 49.64 | 42.58 | 6.88 | 42.58 | ||
| ND-150 | ND-17.40 | ND-305 | ND-46.50 | 4.5–7.30 | 24.9–62.10 | ||
| Milk | 5 | ND | ND | ND | ND | ND | ND |
| Yogurt | 5 | ND | 2.04 (2.01) | ND | ND | 1.07 (0.75) | 0.28 (0.39) |
| 2.23 | 0.69 | 0.3 | |||||
| ND-4.05 | 0.50–1.75 | ND-0.50 | |||||
| Eggs | 14 | ND | ND | ND | ND | 3.61 (1.54) | 4.48 (1.72) |
| 4.43 | 5.27 | ||||||
| ND-4.47 | 0.32–5.31 | ||||||
| Soybeans | 5 | ND | 19.07 (4.39) | 9.04 (1.09) | ND | 99.55 (3.52) | 25.92 (7.34) |
| 21.86 | 9.74 | 101.79 | 30.58 | ||||
| 15.96–22.17 | 8.27–9.81 | 97.06–102.04 | 20.73–31.10 | ||||
| Eggplant | 23 | 39.42 (30.66) | 34.30 (6.98) | ND | 0.60 (0.90) | 5.06 (1.93) | 0.47 (0.48) |
| 98.84 | 46.29 | 2.24 | 7.7 | 1.29 | |||
| 4.17–100.64 | 24.10–48.63 | ND-2.27 | 2.54–7.97 | ND-1.38 | |||
| Spinach | 18 | 31.77 (17.02) | 4.48 (2.46) | ND (0.02) | 2.05 (0.83) | 28.22 (9.72) | 3.33 (1.89) |
| 63.37 | 7.70 | 0.01 | 3.10 | 44.53 | 6.13 | ||
| 9.46–69.72 | 0.14–9.20 | ND-0.08 | 0.79–4.28 | 15.63–52.98 | ND-8.85 | ||
| Tomato | 53 | 2.51 (4.08) | 16.48 (6.93) | 0.50 (0.48) | 0.49 (0.92) | 3.04 (1.41) | 0.08 (0.16) |
| 13.83 | 30.16 | 1.42 | 1.21 | 5.69 | 0.36 | ||
| ND-17.07 | 6.29–35.55 | ND-2.33 | ND-6.38 | 2.91–7.90 | ND-0.73 | ||
| Pumpkin | 13 | ND | 9.87 (6.19) | 0.58 (0.78) | ND | 10.32 (2.83) | 1.77 (1.99) |
| 19.17 | 1.82 | 13.88 | 5.21 | ||||
| 2.95–24.23 | ND-2.15 | 6.19–14.98 | 0.5–6.88 | ||||
| Apricot | 4 | ND | ND | ND | ND | 5.86 (1.59) | ND |
| 6.50 | |||||||
| 4.16–7.68 | |||||||
| Avocado | 5 | ND | ND | ND | 1.81 (2.06) | 3.15 (3.27) | 4.50 (2.52) |
| 4.65 | 6.69 | 7.61 | |||||
| 0.58–5.44 | 0.18–6.72 | 2.02–7.92 | |||||
| Banana | 8 | ND | 37.94 (8.32) | ND | 0.53 (0.79) | 11.91 (2.90) | 1.33 (0.97) |
| 47.37 | ND | 15.10 | 2.67 | ||||
| 25.50–49.49 | ND-1.85 | 7.62–15.79 | ND- 2.75 | ||||
| Citrus fruits | 38 | ND | 79.75 (44.36) | ND | ND | 2.57 (1.28) | 0.12 (0.36) |
| 146.16 | 4.86 | 1.02 | |||||
| 1.21–173.81 | 0.18–6.24 | ND-1.14 | |||||
| Cherry | 5 | ND | 3.42 (0.06) | ND | ND | 2.37 (0.16) | ND |
| 3.46 | 2.47 | ||||||
| 3.42–3.46 | 2.26–2.47 | ||||||
| Grapes | 10 | ND | 2.69 (0.34) | ND | ND | 5.25 (2.61) | 2.59 (0.11) |
| 4.05 | 8.6 | 2.56 | |||||
| 1–4.30 | ND-9.70 | 2.35–2.68 | |||||
| Kiwi | 13 | ND | 1.47 (0.47) | ND | ND | 5.35 (1.06) | 0.73 (0.56) |
| 2.07 | 6.39 | 1.41 | |||||
| 0.48–2.17 | 2.72–6.39 | ND-1.50 | |||||
| Papaya | 6 | ND | 7.25 (5.80) | ND | ND | 14.35 (4.32) | 1.16 (1.59) |
| 11.86 | 15.45 | 2.06 | |||||
| ND-12.48 | 10.32–19.07 | ND-2.99 | |||||
| Pineapple | 5 | ND | 2.69 (1.42) | ND | ND | 1.92 (1.26) | 0.48 (0.21) |
| 3.89 | 3.15 | 0.75 | |||||
| 0.56–3.97 | 0.27–3.18 | 0.32–0.77 | |||||
| Plum | 6 | ND | ND | ND | 4.02 (4.32) | 2.68 (0.30) | 1.74 (2.47) |
| 6.76 | 2.87 | 3.31 | |||||
| 0.96–7.07 | 2.47–2.89 | ND- 3.48 | |||||
| Red fruits | 7 | ND | ND | ND | 7.37 (1.03) | 5.58 (1.16) | 1.97 (1.61) |
| 9.36 | 2.54 | 1.65 | |||||
| 3.34–11.52 | 0.78–3.98 | ND–3.73 | |||||
| Strawberries | 9 | ND | 3.77 (1.52) | ND | ND | 6.00 (1.56) | 0.46 (0.69) |
| 6.09 | 8.52 | 1.5 | |||||
| 2.04–6.41 | 4.62–9.86 | ND-1.62 | |||||
| Olives | 5 | ND | 2.64 (1.58) | ND | 1.95 (1.85) | ND | ND |
| 4.2 | 3.7 | ||||||
| 1.54–4.45 | 0.28–3.94 | ||||||
| Nuts | 47 | ND | 4.40 (7.11) | 0.25 (1.69) | 0.11 (0.41) | 28.64 (24) | 11.14 (8.91) |
| 12.58 | ND | 0.66 | 55.23 | 23.73 | |||
| ND-39.51 | ND-11.58 | ND-2.63 | 6.21–140.55 | ND-50.81 | |||
| Chocolate | 15 | ND | 0.41 (0.65) | 0.42 (0.96) | 3.70 (1.24) | 3.11 (0.70) | 2.00 (0.90) |
| 1.89 | ND | 5.69 | 4.23 | 2.65 | |||
| ND- 1.98 | ND-2.78 | 2.27–5.81 | 2.17–4.65 | ND-2.72 | |||
| Tea | 9 | ND | 2.61 (0.49) | ND | 5.07 (3.80) | 5.86 (1.18) | 18.32 (5.31) |
| 3.12 | 8.34 | 6.59 | 22.84 | ||||
| 2.66–3.37 | ND-10.08 | 3.66–7.64 | 8.23–23.94 | ||||
Some examples of fermented foods that are high in histamine are:
- Sauerkraut and other fermented vegetables
- Yogurt and other fermented dairy products
- Kefir and kombucha
- Soy sauce and tamari
- Miso and tempeh
- Vinegar and pickles
- Wine and beer
If you love fermented foods like I do, don’t worry. You don’t have to give them up completely on a low histamine diet. You just have to be careful about how much you eat and how often you eat them. You may also want to look for alternatives that are lower in levels or have antihistamines.
For example:
- Instead of yogurt or kefir, try coconut milk or almond milk
- Instead of soy sauce or tamari, try coconut aminos or salt
- Instead of miso or tempeh, try tofu or edamame
- Instead of vinegar or pickles, try lemon juice or fresh herbs
- Instead of wine or beer, try water or herbal tea
Summary:
Fermented foods can be tricky for low-histamine diets: while some are naturally low, others can have high histamine and other biogenic amines like tyramine. Cheese, sausages, and sauerkraut are particularly high in histamine, while soy products and some wines have high levels of other amines. Opt for fresh foods and low-histamine fermented options, and be mindful of serving sizes
Alcohol.
Do you like to drink wine or beer? If you do, you should know that these drinks also have histamine and other biogenic amines in them. But they have much less than other fermented foods, so they might not be a big problem. However, there is a catch: alcohol can make histamine more harmful to your body.
Alcohol and histamine are both broken down by the same enzymes in your body, aldehyde dehydrogenase and aldehyde oxidase (Zimatkin & Anichtchik, 1999).
This enzyme can only handle so much at a time. So if you drink alcohol and eat histamine-rich foods at the same time, the enzyme will be overloaded and histamine will build up in your system. This can cause allergic reactions and other symptoms. So be careful when you drink alcohol and eat fermented foods together. You might be getting more histamine than you think.
Also, alcohol liberates histamine from its store in mast cells on top of depressed elimination by inhibition of diamine oxidase. It is not just beer and wine. It is all alcoholic beverages that needs to be avoided.
Summary:
Alcoholic drinks contain less histamine than some fermented foods, but they can hinder your body’s ability to break it down, potentially leading to allergic reactions. Avoid consuming them together with high-histamine foods.
Aged Foods.
Aged foods are foods that have been stored for long periods of time to develop their flavor and texture.
But aging also increases the amount of histamine in the food. That’s because the proteins in the food break down into amino acids over time. And one of these amino acids is called histidine (Moro et al. 2020).
Histidine can be converted into histamine by histidine decarboxylase (HDC), an enzyme that is produced by some bacteria and also inside the body (Mou et al., 2021).
Some examples of aged foods that are high in histamine are:
- Cheese (especially aged cheese like cheddar, parmesan, or blue cheese)
- Meat (especially cured meat like bacon, sausage, or salami)
- Fish (especially canned fish like tuna, sardines, or anchovies)
- Eggs (especially hard-boiled eggs)
You may want to lower your animal products consumption and specially aged cheese or meat. If you don’t want to go the full plant-based diet way then look for alternatives that are lower in levels or have natural antihistamines.
Summary:
Aged foods like cheese and cured meats are high in histamine due to protein breakdown. Eliminate them from the diet completely or opt for fresh or alternative options like mozzarella or fresh meats to lower your histamine intake while still enjoying similar flavors.
Fish.
If you love fish and seafood, you might be disappointed to learn that they are often avoided by low histamine diets. But why is that? Well, fish and seafood can have histamine and other biogenic amines in them, especially if they are not fresh or well-processed. Table 1 shows the levels of these chemicals in different fish and seafood products from Spain. You can see that most of them have very little or no histamine at all (P95 below 20 mg/kg). This is similar to what the EFSA found in their study of European fishery products (Publication, 2011). But some of them can have a lot of it, like fresh salmon (111 mg/kg) and canned sardines (657 mg/kg). That’s because some fish have a lot of free histidine in their flesh, which is a building block of histamine. When these fish are not kept cold or clean enough, bacteria can turn histidine into histamine. And histamine is not the only problem: bacteria can also make other biogenic amines, like putrescine and cadaverine. These are also bad for your health. And cooking or canning the fish won’t help: biogenic amines are heat-resistant, so they won’t go away with heat. That’s why low histamine diets recommend avoiding fish, especially some types like mackerel, tuna, sardines, and anchovies. They are more likely to have high levels than others.
Summary:
Most fish are low in histamine, but fresh salmon and canned options like sardines can be high. To manage histamine intake, prioritize fresh, well-processed fish and avoid high-risk varieties like mackerel, tuna, and sardines.
Tomato, eggplant, and spinach.
You might think that plant-based foods are safe, but that’s not always true. Some vegetables, like tomato, eggplant, and spinach, can have histamine in them (Figure 2). But why is that? Well, some plants naturally have a little bit of it in them. But they can also get more from bacteria.
Bacteria can turn some of the plant’s amino acids into histamine. And this can happen more easily when the vegetables are stored for a long time.
For example, The study performed by Lavizzari et al. (2007), showed spinach can have a lot more histamine after 15 days in the fridge than when it is fresh. That’s because spinach has a high pH, which means it is not very acidic. This makes it easier for some types of bacteria to grow and make histamine (Lavizzari et al., 2007). So if you don’t want to avoid eating tomatoes, eggplant, and spinach, you should eat them fresh and not store them for too long.
Summary:
Though low in histamine, vegetables like tomato, eggplant, and spinach can develop more when levels increase with storage due to bacteria growth. Choose fresh options and avoid prolonged storage for a low-histamine diet.
Putrescine.
Some low histamine diets avoid these vegetables, but not all of them (Figure 1). Some other fruits and vegetables don’t have histamine, but they have another chemical called putrescine. This is also made by bacteria from amino acids. Putrescine is found in citrus fruits, bananas, soybeans, pumpkins, and nuts (Table 1). Citrus fruits have a lot of putrescine, especially mandarines (173 mg/kg). That’s why some low histamine diets avoid citrus fruits, even though they don’t have histamine (Figure 1). But some other vegetables that have putrescine are not avoided by low histamine diets.
These include zucchini, peas, green peppers, and sweet corn (Table 1).
Putrescine might not be as bad as histamine, but it can still cause problems for some people. That’s because putrescine can interfere with an enzyme called DAO that helps break down histamine in the body (Arunlakshana et al., 1954), (MONGAR, 1957), (Hui & Taylor, 1985). Certain biogenic amines, mainly putrescine and cadaverine, interfere with histamine degradation by the DAO enzyme at the intestinal level. The study carried out years ago by Mongar (1957) found that some aliphatic diamines, such as putrescine and cadaverine, could enhance the effects of histamine on guinea pig ileum contractions due to the fact that they could competitively block the DAO enzyme that breaks down histamine (MONGAR, 1957). Without enough DAO, histamine can build up in the body and cause allergic reactions and other symptoms. Putrescine can make this worse by competing with histamine for the DAO enzyme (Arunlakshana et al., 1954), (MONGAR, 1957), (Hui & Taylor, 1985). This means that less histamine can be broken down.
Summary:
Though some vegetables lack histamine, they might contain putrescine which blocks histamine breakdown. If you have low DAO or intolerance, consider avoiding putrescine-rich fruits and vegetables like citrus and soybeans as well as histamine-rich foods.
Chocolate, strawberry, eggs, pineapple, and yogurt.
You might wonder why some foods are excluded by a low histamine diet even though they don’t have histamine or much putrescine in them. These foods include chocolate, strawberry, eggs, pineapple, and yogurt. They also have low or very low levels of other biogenic amines, such as cadaverine, tyramine, spermidine, and spermine. So why are they avoided?
Well, the reason is not very clear. Some people think that these biogenic amines might affect how your body breaks down histamine. They might block the DAO enzyme. But there is not much evidence for this idea. The only study that tested this idea was done in 1985 on rats (Hui & Taylor, 1985). It showed that putrescine and cadaverine could slow down histamine breakdown, but only when they were much higher than normal levels (Hui & Taylor, 1985). So we don’t know if this happens in humans or with other biogenic amines. And we don’t know if low levels of these amines can cause problems for people who are intolerant. That’s why some low histamine diets avoid these foods, but not all of them (Figure 1). Maybe they are being too cautious, or maybe they are right. We need more research to find out.
Summary:
Though low in histamine and other biogenic amines, chocolate, strawberries, eggs, pineapple, and yogurt are sometimes excluded in low-histamine diets due to potential interference with histamine breakdown. However, the evidence is limited, and further research is needed.
Histamine-liberators.
You might have heard that some foods can make the body release more histamine. These foods are called histamine-liberators.
Some examples are citrus fruits, seafood, papaya, tomato, nuts, pineapple, spinach, chocolate, and strawberries (Vlieg-Boerstra et al., 2005).
But is this true? How do these foods make the body release more? The truth is that we don’t know. There is no clear explanation for how this might happen. And there is no solid evidence that it does happen. The only review that looked at this issue found that there are no clinical studies in humans that show that foods can release histamine in the body (Vlieg-Boerstra et al., 2005). The only studies that suggest this possibility are few and not convincing. They are done in test tubes or animals, not in people (Vlieg-Boerstra et al., 2005). So we don’t know for sure if histamine liberators are real or not. Maybe they are, maybe they aren’t. We need more research to find out.
These include:
- Fruits: citrus fruits (oranges, lemons), dried fruits (raisins, dates), strawberries, bananas, papaya, pineapple
- Avocado
- Nuts: peanuts, cashews, walnuts
- Spices: cinnamon, cloves, nutmeg, curry powder
- Shellfish: shrimp, mussels, crab
- Mushrooms: white mushrooms, shiitake mushrooms, truffles
- Olives: green olives, black olives
If you love these foods like I do, don’t worry. You don’t have to give them up completely on a low histamine diet. You just have to be careful about how much you eat and how often you eat them. If you want to avoid histamine-liberators and I will suggest one more time that there is no evidence for this in scientific studies, then you may want to look for alternatives that are lower in levels or have natural antihistamines.
For example:
- Instead of listed fruits, try berries (blueberries, raspberries), kiwi, apples, pear
- Instead of nuts, try seeds (sunflower seeds, pumpkin seeds), coconut flakes
- Instead of listed spices, try ginger, garlic, turmeric
- Instead of shellfish, try tofu
- Instead of olives, try capers
Summary:
While the existence of histamine-liberating foods is unproven, fruits like citrus, seafood, nuts, and mushrooms are often avoided in low-histamine diets due to potential histamine release. Consider substitutes when managing histamine intake.
How Long Should You Follow a Low-Histamine Diet?
A low histamine diet can provide relief for people with histamine intolerance in as little as a few days. However, this does not mean that you should follow full-scale restrictions forever. A low histamine diet can be very restrictive and may increase the risk of nutritional deficiencies if followed for too long if not properly planned.
Instead of following a low histamine diet indefinitely, it is better to use it as a tool to find out your personal tolerance level.
The best way to do this is to start with a strict low histamine diet for 2 weeks, and then gradually reintroduce higher-histamine foods one by one while monitoring your symptoms. This will help you identify which foods trigger your reactions and which ones you can tolerate without any problems. You can then adjust your diet accordingly and enjoy more food options without compromising your health.
Summary:
While a low-histamine diet can quickly ease symptoms, use it for 2 weeks to identify triggers and then reintroduce foods for a personalized, less restrictive approach.
Conclusion.
A low histamine diet can help you manage your symptoms if you have histamine intolerance.
But it is not a simple or easy diet to follow. It requires careful planning, monitoring, and adjusting. It also requires consulting with a nutrition professional and a healthcare provider to make sure you are doing it right and safely.
We can say that low histamine diets might help some people who have an intolerance. But we can also say that there is a lot of confusion about what foods to avoid. Only 32% of the foods that are excluded by low histamine diets have histamine in them. The rest of the foods might have other biogenic amines that could affect levels in your body. We don’t know for sure how this works or how much it matters. We also don’t know if some foods can make your body release more. This is a popular idea, but there is no solid proof for it. So we need more research to understand how different foods affect histamine intolerance. We need to find out which foods are really bad for histamine-intolerant people and which ones are safe to eat. This way, we can make low-histamine diets more effective and easier to follow.
That’s why I hope this article has been helpful to you. I’ve given you some general tips and guidelines on how to eat low histamine for better health. I’ve also given you some examples of foods to avoid and foods to eat on this diet.
But remember that these are not absolute rules. You may find that some foods affect you more than others or not at all. You may also find that some foods are fine in small amounts but not in large amounts.
So listen to your body and use these guidelines as a starting point for your low histamine diet.
And if you need more help or advice, don’t hesitate to contact me.
Thank you for reading and happy eating.
When you think of antihistamines, you’re probably only thinking about getting rid of a runny nose, congestion, or a common cold. However, we’re learning that antihistamines can be used for nausea, insomnia, and even… depression?
FAQ
References:
- , W. J., Schenk, M., Lackner, S., Enko, D., Mangge, H., & Forster, F. (2019). Diamine oxidase supplementation improves symptoms in patients with histamine intolerance. Food science and biotechnology, 28(6), 1779–1784. https://doi.org/10.1007/s10068-019-00627-3
- Chung, B. Y., Park, S. Y., Byun, Y. S., Son, J. H., Choi, Y. W., Cho, Y. S., Kim, H. O., & Park, C. W. (2017). Effect of Different Cooking Methods on Histamine Levels in Selected Foods. Annals of dermatology, 29(6), 706–714. https://doi.org/10.5021/ad.2017.29.6.706
- Teresa, M., Luz, M., & Carmen, M. (2021). Low-Histamine Diets: Is the Exclusion of Foods Justified by Their Histamine Content? Nutrients, 13(5), 1395. https://doi.org/10.3390/nu13051395
- Lavizzari, T., Veciana-Nogués, M. T., Weingart, O., Bover-Cid, S., Mariné-Font, A., & Vidal-Carou, M. C. (2007). Occurrence of biogenic amines and polyamines in spinach and changes during storage under refrigeration. Journal of agricultural and food chemistry, 55(23), 9514–9519. https://doi.org/10.1021/jf071307l
- Wagner, N., Dirk, D., Peveling-Oberhag, A., Reese, I., Rady-Pizarro, U., Mitzel, H., & Staubach, P. (2017). A Popular myth – low-histamine diet improves chronic spontaneous urticaria – fact or fiction? Journal of the European Academy of Dermatology and Venereology, 31(4), 650-655. https://doi.org/10.1111/jdv.13966
- Rosell-Camps, A., Zibetti, S., Pérez-Esteban, G., Vila-Vidal, M., Ferrés-Ramis, L., & García-Teresa-García, E. (2013). Histamine intolerance as a cause of chronic digestive complaints in pediatric patients. Revista espanola de enfermedades digestivas, 105(4), 201–206. https://doi.org/10.4321/s1130-01082013000400004
- Mušič, E., Korošec, P., Šilar, M., Adamič, K., Košnik, M., & Rijavec, M. (2013). Serum diamine oxidase activity as a diagnostic test for histamine intolerance. Wiener klinische Wochenschrift, 125(9-10), 239–243. https://doi.org/10.1007/s00508-013-0354-y
- Wantke, F., Götz, M., & Jarisch, R. (1993). Histamine-free diet: treatment of choice for histamine-induced food intolerance and supporting treatment for chronic headaches. Clinical and experimental allergy : journal of the British Society for Allergy and Clinical Immunology, 23(12), 982–985. https://doi.org/10.1111/j.1365-2222.1993.tb00287.x
- Son, J. H., Chung, B. Y., Kim, H. O., & Park, C. W. (2018). A Histamine-Free Diet Is Helpful for Treatment of Adult Patients with Chronic Spontaneous Urticaria. Annals of dermatology, 30(2), 164–172. https://doi.org/10.5021/ad.2018.30.2.164
- Joneja, J. M. V., & Carmona-Silva, C. (2001). Outcome of a Histamine-restricted Diet Based on Chart Audit. Journal of Nutritional & Environmental Medicine, 11(4), 249–262. https://doi.org/10.1080/13590840120103094
- King, W., McCargar, L., Joneja, J. M., & Barr, S. I. (2000). Benefits of a Histamine-Reducing Diet for Some Patients with Chronic Urticaria and Angioedema. Canadian journal of dietetic practice and research : a publication of Dietitians of Canada = Revue canadienne de la pratique et de la recherche en dietetique : une publication des Dietetistes du Canada, 61(1), 24–26. [PubMed]
- Maintz, L., Benfadal, S., Allam, J., Hagemann, T., Fimmers, R., & Novak, N. (2006). Evidence for a reduced histamine degradation capacity in a subgroup of patients with atopic eczema. The Journal of Allergy and Clinical Immunology, 117(5), 1106–1112. https://doi.org/10.1016/j.jaci.2005.11.041
- Böhn, L., Störsrud, S., Törnblom, H., Bengtsson, U., & Simrén, M. (2013). Self-reported food-related gastrointestinal symptoms in IBS are common and associated with more severe symptoms and reduced quality of life. The American journal of gastroenterology, 108(5), 634–641. https://doi.org/10.1038/ajg.2013.105
- Teresa, M., Luz, M., & Carmen, M. (2018). Biogenic Amines in Plant-Origin Foods: Are they Frequently Underestimated in Low-Histamine Diets? Foods, 7(12), 205. https://doi.org/10.3390/foods7120205 [PDF]
- Publication, E. (2011). Scientific Opinion on risk based control of biogenic amine formation in fermented foods. EFSA Journal, 9(10), 2393. https://doi.org/10.2903/j.efsa.2011.2393
- ARUNLAKSHANA, O., MONGAR, J. L., & SCHILD, H. O. (1954). Potentiation of pharmacological effects of histamine by histaminase inhibitors. The Journal of physiology, 123(1), 32–54. https://doi.org/10.1113/jphysiol.1954.sp005032
- MONGAR, J. L. (1957). EFFECT OF CHAIN LENGTH OF ALIPHATIC AMINES ON HISTAMINE POTENTIATION AND RELEASE. British Journal of Pharmacology and Chemotherapy, 12(2), 140-148. https://doi.org/10.1111/j.1476-5381.1957.tb00112.x
- Hui, J. Y., & Taylor, S. L. (1985). Inhibition of in vivo histamine metabolism in rats by foodborne and pharmacologic inhibitors of diamine oxidase, histamine N-methyltransferase, and monoamine oxidase. Toxicology and Applied Pharmacology, 81(2), 241-249. https://doi.org/10.1016/0041-008X(85)90160-7
- Vlieg-Boerstra, B. J., van der Heide, S., Oude Elberink, J. N., Kluin-Nelemans, J. C., & Dubois, A. E. (2005). Mastocytosis and adverse reactions to biogenic amines and histamine-releasing foods: what is the evidence?. The Netherlands journal of medicine, 63(7), 244–249.[PubMed]
- Schnedl, W. J., Schenk, M., Lackner, S., Enko, D., Mangge, H., & Forster, F. (2019). Diamine oxidase supplementation improves symptoms in patients with histamine intolerance. Food science and biotechnology, 28(6), 1779–1784. https://doi.org/10.1007/s10068-019-00627-3
- Capozzi, V., Russo, P., Ladero, V., Fernández, M., Fiocco, D., Alvarez, M. A., Grieco, F., & Spano, G. (2012). Biogenic Amines Degradation by Lactobacillus plantarum: Toward a Potential Application in Wine. Frontiers in Microbiology, 3. https://doi.org/10.3389/fmicb.2012.00122
- Oksaharju, A., Kankainen, M., Kekkonen, R. A., Lindstedt, K. A., Kovanen, P. T., Korpela, R., & Miettinen, M. (2011). Probiotic Lactobacillus rhamnosus downregulates FCER1 and HRH4 expression in human mast cells. World journal of gastroenterology, 17(6), 750–759. https://doi.org/10.3748/wjg.v17.i6.750
- Forsythe, P., Wang, B., Khambati, I., & Kunze, W. A. (2012). Systemic Effects of Ingested Lactobacillus Rhamnosus: Inhibition of Mast Cell Membrane Potassium (IKCa) Current and Degranulation. PLoS ONE, 7(7). https://doi.org/10.1371/journal.pone.0041234
- Dev, S., Mizuguchi, H., Das, A. K., Matsushita, C., Maeyama, K., Umehara, H., Ohtoshi, T., Kojima, J., Nishida, K., Takahashi, K., & Fukui, H. (2008). Suppression of histamine signaling by probiotic Lac-B: a possible mechanism of its anti-allergic effect. Journal of pharmacological sciences, 107(2), 159–166. https://doi.org/10.1254/jphs.08028fp
- Mokhtar, S. M., Mostafa, G. a. E., Taha, R. A., & Eldeep, G. S. S. (2012). Effect of different starter cultures on the biogenic amines production as a critical control point in fresh fermented sausages. European Food Research and Technology, 235(3), 527–535. https://doi.org/10.1007/s00217-012-1777-9
- Rai, K. P., Pradhan, H. R., Sharma, B. K., & Rijal, S. K. (2014). Histamine in Foods: Its Safety and Human Health Implications. Journal of Food Science and Technology Nepal, 8, 1–11. https://doi.org/10.3126/jfstn.v8i0.11720
- Priyadarshani, W. M. D., & Rakshit, S. K. (2011). Screening selected strains of probiotic lactic acid bacteria for their ability to produce biogenic amines (histamine and tyramine). International Journal of Food Science and Technology, 46(10), 2062–2069. https://doi.org/10.1111/j.1365-2621.2011.02717.x
- Herrero-Fresno, A., Martínez, N., Sánchez-Llana, E., Díaz, M., Fernández, M., Martin, M. C., Ladero, V., & Alvarez, M. A. (2012). Lactobacillus casei strains isolated from cheese reduce biogenic amine accumulation in an experimental model. International journal of food microbiology, 157(2), 297–304. https://doi.org/10.1016/j.ijfoodmicro.2012.06.002
- Stratton, J. E., Hutkins, R. W., Sumner, S. S., & Taylor, S. L. (1992). Histamine and Histamine-Producing Bacteria in Retail Swiss and Low-Salt Cheeses. Journal of Food Protection, 55(6), 435-439. https://doi.org/10.4315/0362-028X-55.6.435
- Rossi, F., Gardini, F., Rizzotti, L., La Gioia, F., Tabanelli, G., & Torriani, S. (2011). Quantitative analysis of histidine decarboxylase gene (hdcA) transcription and histamine production by Streptococcus thermophilus PRI60 under conditions relevant to cheese making. Applied and environmental microbiology, 77(8), 2817–2822. https://doi.org/10.1128/AEM.02531-10
- Gezginc, Y., Akyol, I., Kuley, E., & Özogul, F. (2013). Biogenic amines formation in Streptococcus thermophilus isolated from home-made natural yogurt. Food Chemistry, 138(1), 655-662. https://doi.org/10.1016/j.foodchem.2012.10.138
- Obara, I., Telezhkin, V., Alrashdi, I., & Chazot, P. L. (2020). Histamine, histamine receptors, and neuropathic pain relief. British journal of pharmacology, 177(3), 580–599. https://doi.org/10.1111/bph.14696
- Prinz, C., Zanner, R., Gerhard, M., Mahr, S., Neumayer, N., Höhne-Zell, B., & Gratzl, M. (1999). The mechanism of histamine secretion from gastric enterochromaffin-like cells. The American journal of physiology, 277(5), C845–C855. https://doi.org/10.1152/ajpcell.1999.277.5.C845
- Pinzer, T. C., Tietz, E., Waldmann, E., Schink, M., Neurath, M. F., & Zopf, Y. (2018). Circadian profiling reveals higher histamine plasma levels and lower diamine oxidase serum activities in 24% of patients with suspected histamine intolerance compared to food allergy and controls. Allergy, 73(4), 949–957. https://doi.org/10.1111/all.13361
- Maintz, L., & Novak, N. (2007). Histamine and histamine intolerance. The American journal of clinical nutrition, 85(5), 1185–1196. https://doi.org/10.1093/ajcn/85.5.1185
- Jing, H., Wang, Z., & Chen, Y. (2012). Effect of oestradiol on mast cell number and histamine level in the mammary glands of rat. Anatomia, histologia, embryologia, 41(3), 170–176. https://doi.org/10.1111/j.1439-0264.2011.01120.x
- Vasiadi, M., Kempuraj, D., Boucher, W., Kalogeromitros, D., & Theoharides, T. C. (2006). Progesterone inhibits mast cell secretion. International journal of immunopathology and pharmacology, 19(4), 787–794. https://doi.org/10.1177/039463200601900408
- Comas-Basté, O., Sánchez-Pérez, S., Veciana-Nogués, M. T., Latorre-Moratalla, M., & Vidal-Carou, M. D. C. (2020). Histamine Intolerance: The Current State of the Art. Biomolecules, 10(8), 1181. https://doi.org/10.3390/biom10081181
- Maintz, L., & Novak, N. (2007). Histamine and histamine intolerance. The American journal of clinical nutrition, 85(5), 1185–1196. https://doi.org/10.1093/ajcn/85.5.1185
- Schink, M., Konturek, P. C., Tietz, E., Dieterich, W., Pinzer, T. C., Wirtz, S., Neurath, M. F., & Zopf, Y. (2018). Microbial patterns in patients with histamine intolerance. Journal of physiology and pharmacology : an official journal of the Polish Physiological Society, 69(4), 10.26402/jpp.2018.4.09. https://doi.org/10.26402/jpp.2018.4.09
- Barcik, W., Pugin, B., Brescó, M. S., Westermann, P., Rinaldi, A., Groeger, D., Van Elst, D., Sokolowska, M., Krawczyk, K., Frei, R., Ferstl, R., Wawrzyniak, M., Altunbulakli, C., Akdis, C. A., & O’Mahony, L. (2019). Bacterial secretion of histamine within the gut influences immune responses within the lung. Allergy, 74(5), 899–909. https://doi.org/10.1111/all.13709
- Kofler, L., Ulmer, H., & Kofler, H. (2011). Histamine 50-skin-prick test: a tool to diagnose histamine intolerance. ISRN allergy, 2011, 353045. https://doi.org/10.5402/2011/353045
- Izquierdo-Casas, J., Comas-Basté, O., Latorre-Moratalla, M. L., Lorente-Gascón, M., Duelo, A., Soler-Singla, L., & Vidal-Carou, M. C. (2019). Diamine oxidase (DAO) supplement reduces headache in episodic migraine patients with DAO deficiency: A randomized double-blind trial. Clinical nutrition (Edinburgh, Scotland), 38(1), 152–158. https://doi.org/10.1016/j.clnu.2018.01.013
- Yacoub, M. R., Ramirez, G. A., Berti, A., Mercurio, G., Breda, D., Saporiti, N., Burastero, S., Dagna, L., & Colombo, G. (2018). Diamine Oxidase Supplementation in Chronic Spontaneous Urticaria: A Randomized, Double-Blind Placebo-Controlled Study. International archives of allergy and immunology, 176(3-4), 268–271. https://doi.org/10.1159/000488142
- Hirschowitz B. I. (1985). Histamine and the gut. New England and regional allergy proceedings, 6(1), 21–27. https://doi.org/10.2500/108854185779048942
- Hagel, A. F., Layritz, C. M., Hagel, W. H., Hagel, H. J., Hagel, E., Dauth, W., Kressel, J., Regnet, T., Rosenberg, A., Neurath, M. F., Molderings, G. J., & Raithel, M. (2013). Intravenous infusion of ascorbic acid decreases serum histamine concentrations in patients with allergic and non-allergic diseases. Naunyn-Schmiedeberg’s archives of pharmacology, 386(9), 789–793. https://doi.org/10.1007/s00210-013-0880-1
- Shulpekova, Y. O., Nechaev, V. M., Popova, I. R., Deeva, T. A., Kopylov, A. T., Malsagova, K. A., Kaysheva, A. L., & Ivashkin, V. T. (2021). Food Intolerance: The Role of Histamine. Nutrients, 13(9), 3207. https://doi.org/10.3390/nu13093207
- Smolinska, S., Winiarska, E., Globinska, A., & Jutel, M. (2022). Histamine: A Mediator of Intestinal Disorders-A Review. Metabolites, 12(10), 895. https://doi.org/10.3390/metabo12100895
- Martner-Hewes, P. M., Hunt, I. F., Murphy, N. J., Swendseid, M. E., & Settlage, R. H. (1986). Vitamin B-6 nutriture and plasma diamine oxidase activity in pregnant Hispanic teenagers. The American journal of clinical nutrition, 44(6), 907–913. https://doi.org/10.1093/ajcn/44.6.907
- Sharma, S. C., & Jande, M. B. (1989). Inhibition of mast cell histamine release by copper. Archives internationales de pharmacodynamie et de therapie, 299, 254–268.[PubMed]
- Johnston C. S. (1996). The antihistamine action of ascorbic acid. Sub-cellular biochemistry, 25, 189–213. https://doi.org/10.1007/978-1-4613-0325-1_10
- Zimatkin, S. M., & Anichtchik, O. V. (1999). Alcohol-histamine interactions. Alcohol and alcoholism (Oxford, Oxfordshire), 34(2), 141–147. https://doi.org/10.1093/alcalc/34.2.141
- Mou, Z., Yang, Y. Y., Hall, A. J., & Jiang, X. (2021). The taxonomic distribution of histamine-secreting bacteria in the human gut microbiome. BMC Genomics, 22(1). https://doi.org/10.1186/s12864-021-08004-3
- Moro, J., Tomé, D., Schmidely, P., Demersay, T. C., & Azzout-Marniche, D. (2020). Histidine: A Systematic Review on Metabolism and Physiological Effects in Human and Different Animal Species. Nutrients, 12(5), 1414. https://doi.org/10.3390/nu12051414
Do you have any questions about nutrition and health?
I would love to hear from you and answer them in my next post. I appreciate your input and opinion and I look forward to hearing from you soon. I also invite you to follow us on Facebook, Instagram, and Pinterest for more diet, nutrition, and health content. You can leave a comment there and connect with other health enthusiasts, share your tips and experiences, and get support and encouragement from our team and community.
I hope that this post was informative and enjoyable for you and that you are prepared to apply the insights you learned. If you found this post helpful, please share it with your friends and family who might also benefit from it. You never know who might need some guidance and support on their health journey.
– You Might Also Like –

Learn About Nutrition
Milos Pokimica is a doctor of natural medicine, clinical nutritionist, medical health and nutrition writer, and nutritional science advisor. Author of the book series Go Vegan? Review of Science, he also operates the natural health website GoVeganWay.com
Medical Disclaimer
GoVeganWay.com brings you reviews of the latest nutrition and health-related research. The information provided represents the personal opinion of the author and is not intended nor implied to be a substitute for professional medical advice, diagnosis, or treatment. The information provided is for informational purposes only and is not intended to serve as a substitute for the consultation, diagnosis, and/or medical treatment of a qualified physician or healthcare provider.NEVER DISREGARD PROFESSIONAL MEDICAL ADVICE OR DELAY SEEKING MEDICAL TREATMENT BECAUSE OF SOMETHING YOU HAVE READ ON OR ACCESSED THROUGH GoVeganWay.com
NEVER APPLY ANY LIFESTYLE CHANGES OR ANY CHANGES AT ALL AS A CONSEQUENCE OF SOMETHING YOU HAVE READ IN GoVeganWay.com BEFORE CONSULTING LICENCED MEDICAL PRACTITIONER.
In the event of a medical emergency, call a doctor or 911 immediately. GoVeganWay.com does not recommend or endorse any specific groups, organizations, tests, physicians, products, procedures, opinions, or other information that may be mentioned inside.
Editor Picks –
Milos Pokimica is a health and nutrition writer and nutritional science advisor. Author of the book series Go Vegan? Review of Science, he also operates the natural health website GoVeganWay.com
Latest Articles –
Top Health News — ScienceDaily
- Alzheimer’s may begin with a silent drop in brain blood flowon February 24, 2026
Subtle changes in brain blood flow and oxygen use are closely linked to hallmark signs of Alzheimer’s, including amyloid plaques and memory-related brain shrinkage. Simple, noninvasive scans may one day help spot risk earlier—by looking at the brain’s vascular health, not just its plaques.
- Scientists engineer bacteria to eat cancer tumors from the inside outon February 24, 2026
Researchers are engineering bacteria to invade tumors and consume them from the inside. Because tumor cores lack oxygen, they’re the perfect breeding ground for these microbes. The team added a genetic tweak that helps the bacteria survive longer near oxygen-exposed edges — but only once enough of them are present to trigger the change. It’s a carefully programmed biological attack that could one day offer a new way to destroy cancer.
- Massive US study finds higher cancer death rates near nuclear power plantson February 24, 2026
A sweeping nationwide study has found that U.S. counties located closer to operating nuclear power plants have higher cancer death rates than those farther away. Researchers analyzed data from every nuclear facility and all U.S. counties between 2000 and 2018, adjusting for income, education, smoking, obesity, environmental conditions, and access to health care. Even after accounting for those factors, cancer mortality was higher in communities nearer to nuclear plants, particularly among older […]
- Training harder could be rewiring your gut bacteriaon February 24, 2026
Training harder may do more than build muscle—it could transform your gut. Researchers found that intense workouts change the balance of bacteria and important compounds in athletes’ digestive systems. When training loads dropped, diet quality slipped and digestion slowed, triggering different microbial shifts. These hidden changes might influence performance in ways scientists are only beginning to understand.
- Scientists reverse muscle aging in mice and discover a surprising catchon February 24, 2026
A UCLA study in mice reveals that aging muscle stem cells accumulate a protein that slows repair but boosts survival. This protein, NDRG1, acts like a brake, preventing cells from activating quickly after injury. When researchers blocked it in older mice, muscle healing sped up dramatically — but stem cells became less resilient over time. The work suggests aging may reflect a survival trade-off rather than straightforward decline.
- Less sugar as a baby, fewer heart attacks as an adulton February 23, 2026
People whose sugar intake was restricted before birth and in early childhood had markedly lower rates of heart disease later in life. Compared to those never exposed to rationing, their risks of heart attack, stroke, heart failure, and cardiovascular death were cut by roughly 20–30%.
- Scientists create universal nasal spray vaccine that protects against COVID, flu, and pneumoniaon February 23, 2026
Scientists at Stanford Medicine have unveiled a bold new kind of “universal” vaccine that could one day protect against everything from COVID-19 and the flu to bacterial pneumonia and even common allergens. Instead of targeting a specific virus or bacterium, the nasal spray vaccine supercharges the lungs’ own immune defenses, keeping them on high alert for months. In mice, it slashed viral levels, prevented severe illness, and even blocked allergic reactions.
PubMed, #vegan-diet –
- Veganism: an extended theory of planned behavior framework incorporating ethical, environmental, and sociodemographic determinantson February 20, 2026
CONCLUSION: This study broadens the TPB by integrating ethical, normative, and psychosocial dimensions that explain vegan intentions beyond traditional predictors. Findings underscore the importance of moral identity, perceived social expectations, and contextual factors in shaping sustainable dietary behaviors.
- Association Between Diet and Metabolome in Childhood and Adolescence: A Systematic Reviewon February 11, 2026
CONCLUSION: This review identifies several metabolites consistently associated with specific dietary components across different studies in children and adolescents. These findings support the potential of metabolomics for validating dietary biomarkers and improving the accuracy of dietary assessment in pediatric populations. Although metabolomic markers reflect actual dietary intake, their implications for health outcomes remain to be explored.
- Growth Trajectories in Infants From Families With Plant-Based or Omnivorous Dietary Patternson February 5, 2026
CONCLUSIONS AND RELEVANCE: In this cohort study, infants from vegan households had growth patterns similar to those from omnivorous households, with a higher odds of early underweight that decreased by age 24 months. In the context of developed countries, these findings seem reassuring. Further research should examine vegan diet quality and the impact of nutritional counseling during pregnancy and infancy in supporting optimal infant development.
- Influences of vegan status on protein intake, lean body mass, and strength in lightly active, young women: A cross-sectional studyon February 5, 2026
CONCLUSION: These data suggest that functional indicators of body protein status may be adversely impacted by long-term adherence to vegan diets in young adult women.
- Iodineon January 1, 2006
Iodine is an essential trace nutrient for all infants that is a normal component of breastmilk. Infant requirements are estimated to be 15 mcg/kg daily in full-term infants and 30 mcg/kg daily in preterm infants.[1] Breastmilk iodine concentration correlates well with maternal urinary iodine concentration and may be a useful index of iodine sufficiency in infants under 2 years of age, but there is no clear agreement on a value that indicates iodine sufficiency, and may not correlate with […]
Random Posts –
Featured Posts –
Latest from PubMed, #plant-based diet –
- Differences in Protein Quantity and Quality Across a Spectrum of Plant-Based Meals: Analysis of a Large National Dietary Surveyby Sophie L van Oppenraaij on February 24, 2026
CONCLUSIONS: This study shows that only a small proportion of Dutch adults met both protein-related recommendations and sustainability goals, due to lower protein quantity and quality in more plant-based diets. This study emphasizes the need for professional guidance, especially in individuals with higher protein requirements, to facilitate a successful transition to a more plant-based diet.
- Dietary animal fat disrupts gut microbiota and aggravates Scl-cGVHD after allogeneic hematopoietic stem cell transferby Danielle D Millick on February 24, 2026
Allogeneic hematopoietic stem cell transplant (allo-HSCT) is an effective treatment for high-risk or relapsed acute leukemia. However, the frequent occurrence of graft-versus-host disease (GVHD) poses significant complications. Modifiable factors such as the gut microbiome and dietary regimen have the potential to influence the frequency and severity of GVHD. Previous studies in mouse models have shown a direct link between obesity and increased severity of GVHD; however, analysis of human […]
- Evaluation of biochemical, histopathological, hematological, and genotoxic effects of some indigenous weed plant extracts in albino rats toward a natural and safe alternative to synthetic insecticidesby Muhammad Asif Zahoor on February 23, 2026
CONCLUSION: These findings suggest that these weed plants have the potential to be used as biopesticides for future integrated pest management (IPM) programs.
- Comparative life cycle assessment of conventional dairy products and plant-based analog and hybrid alternatives: current status and future perspectivesby Muhammed Fidan on February 23, 2026
Conventional dairy products are associated with relatively high environmental burdens, largely driven by farm-level processes such as enteric methane emissions, feed production, and land use. These concerns have intensified interest in plant-based analog and hybrid dairy products as potential alternatives. However, environmental comparisons among these product categories remain inconsistent due to differences in functional units, methodological choices, and nutritional characteristics. This…
- Dietary Patterns and Indicators of Cognitive Functionby Hui Chen on February 23, 2026
CONCLUSIONS AND RELEVANCE: Results reveal that healthy diets, exemplified by the DASH diet for blood pressure control and diets with lower hyperinsulinemia and inflammation potentials, were associated with a lower SCD risk and better cognitive function. These findings underscore the importance of a healthy diet for maintaining long-term cognitive health.
- Adherence to the EAT-Lancet Planetary Health Diet during Pregnancy and Associations with Preterm Birth and Infant Size: a prospective analysis from the New Hampshire Birth Cohortby Leyre Notario Barandiaran on February 21, 2026
CONCLUSION: Originally proposed for chronic disease prevention and planetary sustainability, higher adherence to the PHD during pregnancy may also benefit birth outcomes, particularly lower odds of preterm birth.