Antioxidant Role in Depression and Anxiety: The Missing Piece
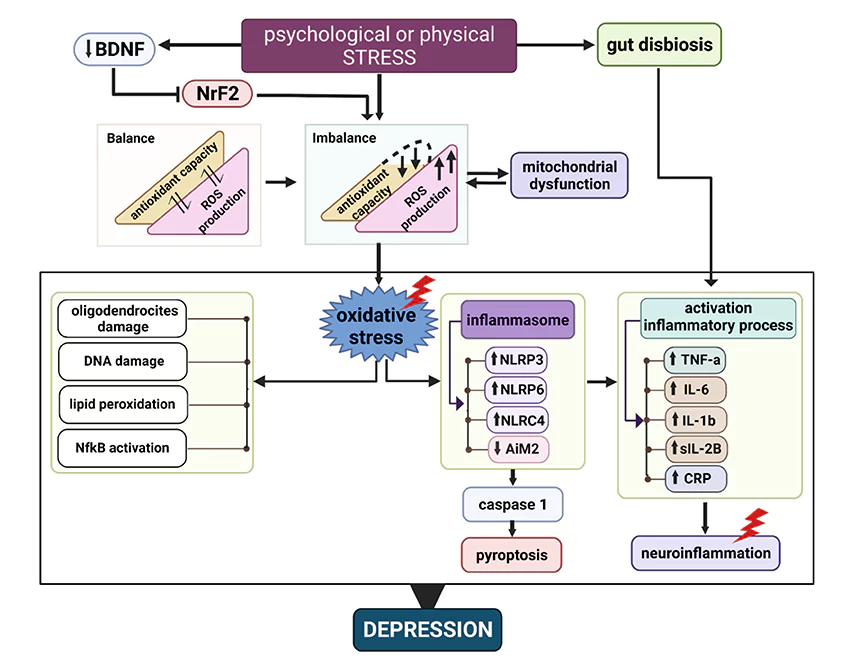
Oxidative stress with chronic inflammation in the brain is associated with the development of neuropsychiatric disorders including major depression and anxiety.
Milos Pokimica
Written By: Milos Pokimica
Medically Reviewed by: Dr. Xiùying Wáng, M.D.
Updated August 7, 2023Key Takeaways:
-Chronic inflammation in the brain caused by poor diet is a root cause of many mental illnesses.
-Hypoglycemia attacks may lead to post-traumatic stress disorder.
-The brain’s high demand for oxygen and energy makes it more susceptible to oxidative stress, which can be lethal to neurons even with small imbalances in antioxidant defense mechanisms. The brain is also highly susceptible to oxidative damage due to its rich iron and fat content, making it more vulnerable to neuropsychiatric disorders.
-Antioxidants can protect cells from oxidative damage, modulate neurotransmitters, and decrease inflammation. Studies suggest that dietary antioxidants may also support standard medication in treating these disorders in humans.
-Antidepressants and medications for bipolar disorder exhibit antioxidant qualities, while mitochondrial dysfunction caused by oxidative damage contributes to chronic diseases including neurodegenerative diseases. Antidepressants also inhibit mitochondrial MAO activity, which supports the idea of antioxidant action in treating depression and anxiety.
-The blood-brain barrier limits the entry of antioxidants into the brain, but certain carotenoids like lutein can pass through and are essential for preventing age-related brain and eye degeneration.
Anxiety.
Anxiety is very common.
It is the most dominant kind of mental disease in the US. (Steel et al., 2014), (Ettman et al., 2020). Anxiety affects more than 40 million individuals or 18% of the population. However, only about a third of people suffering from this condition seek treatment. Anxiety and depression frequently overlap, with roughly half of the depressed people also having anxiety.
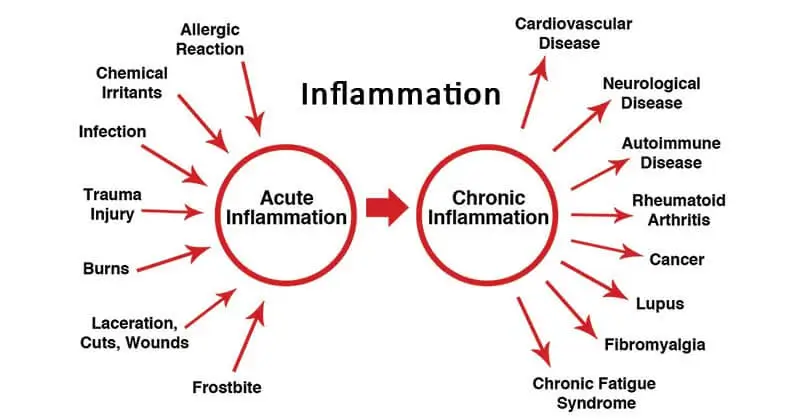
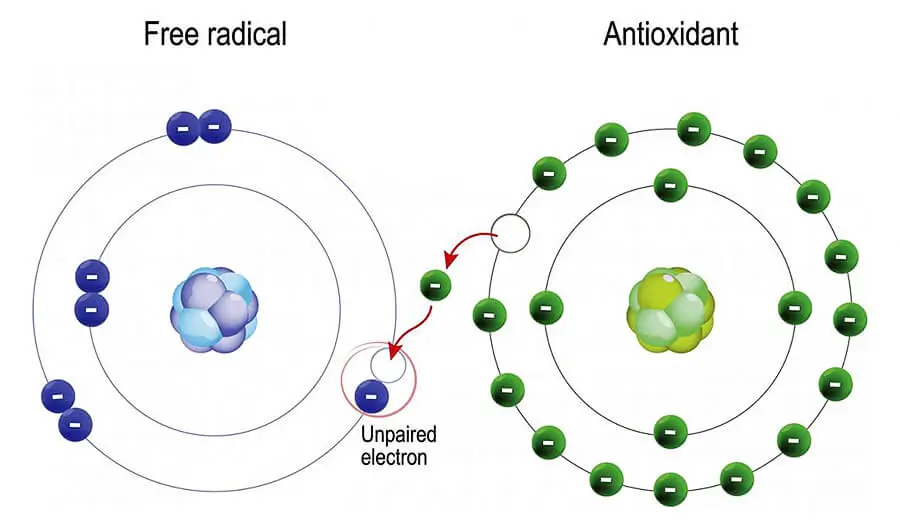
In my practice, part of what I will discuss when explaining treatment options is the important role of diet in managing all types of mental illness. It is a root cause of most mental illnesses that are not genetic if there are no underlined phycological traumas or issues. In most cases, depression is caused by chronic inflammation in the brain. According to some studies (Gautam et al., 2012), oxidative stress is a condition where there is an imbalance between the production of free radicals and the ability of the antioxidant system to neutralize them.
In addition to healthy guidelines such as avoidance of psychoactive substances and limiting or avoiding alcohol and caffeine, there are many other dietary considerations that can help relieve anxiety. For example, complex carbohydrates are metabolized more slowly and thus help maintain a more even blood sugar level. If you are suffering from chronic hypoglycemia attacks you are also suffering from post-traumatic stress disorder. When sugar drops below normal levels your brain cells begin to die off and this triggers survival mechanisms that if not corrected could leave to post-traumatic stress disorder. In experimental conditions with mice, this has been shown repeatedly.
Oxidative Stress and Neuroinflammation.
There is growing evidence that chronic inflammation in the brain may be associated with the development of a wide range of neuropsychiatric disorders. This includes not just classical cognitive decline but other neuropsychiatric disorders like depression and anxiety. This is a consequence of a pro-inflammatory diet that causes an imbalance between oxidative stress and the antioxidant defense system in the brain.
Major depression and anxiety are currently associated with a lowered total antioxidant state.
Free radicals are unstable molecules that can harm neurons and neurotransmitters, as well as other cells and organs. Oxidative stress has the potential to impair nervous system performance and have an impact on emotion, cognition, and behavior. Antioxidants are substances that can scavenge free radicals and protect cells from oxidative damage. They have the ability to modulate the activity of various neurotransmitters, including serotonin, dopamine, and glutamate, which are crucial for controlling mood and the stress response. Inflammation, another element that can add to depression and anxiety, can also be decreased by antioxidants.
The standard antidepressants that will be prescribed to patients with major depression may also produce beneficial effects outside of the regulation of neurochemistry. It is proven in research that most antidepressants act as antioxidants in the brain and one of the therapeutic effects they exhibit is normalizing the damage caused by oxidative stress. Most of these medications also come with serious side effects.
In recent years there was a wide range of studies that correlated and explained the role of oxidative stress-induced neuroinflammatory response, mitochondrial dysfunction, neuroplastic deficits, and intracellular signaling pathways in the development of depressive and anxiety disorders. Today this is accepted science. A meta-analysis that included 52 randomized controlled trials with 4049 participants and was released in 2022 provides a thorough and current review of the literature on this subject. This meta-analysis discovered that antioxidant supplementation, particularly for magnesium, zinc, selenium, coenzyme Q10, tea, coffee, and crocin, had a protective impact on depression and anxiety. (Wang et al., 2022).
Chronic inflammation as a result of oxidative stress is also correlated to neuropathies. Chronic inflammation damages all types of major groups of cellular macro-molecules not just proteins but also lipids, carbohydrates, and nucleic acids. All of this damage will eventually lead to DNA damage, mutation and cancer or cell death and cognitive decline, and neuropathy.
Metabolic rate.
Why this happens in the brain more than other organs because of the high demand of the brain for oxygen. Our brains use 20% of all the calories we eat and 20% of the oxygen we breathe. Bear in mind that a brain weighs about three pounds. This means that the metabolic rate of the brain cells is higher than other cells in the body. Deprived of oxygen brain cells die quickly.
Even the smallest imbalances in antioxidant defense mechanisms can be lethal to neurons. Because we have a limited amount of brain cells even the smallest imbalances in antioxidant defense mechanisms will lead to extensive damage if the imbalances are chronic. This also leads to imbalances in brain neurochemical processes and is correlated to depression and anxiety.
Blood-brain barrier.
The nervous system is rich in iron and fat. Iron is very reactive and oxidizes quickly. Fat, especially unsaturated fats are also very reactive to oxygen. These factors render tissues more vulnerable to oxidative damage, as do the high metabolic activity and abundant blood supply.
In a situation where most of the population is vitamin E deficient, this would translate into an increase in neuropsychiatric disorders.
The second and main problem that underlines all of the oxidative damage outside of direct nutritional deficiencies is something known as the blood-brain barrier. If you are low on vitamin E some other fat-salable antioxidant might neutralize some of the free radicals but in the brain, it is a different story.
Because neural cells are extremely sensitive and require a pure environment to function effectively, the brain has to defend itself from toxins and undesired substances far more than the rest of the body. As a result, there is a blood-brain barrier that keeps a lot of toxic substances out. At the same time, it keeps a lot of antioxidants out as well.
Only lutein and zeaxanthin from more than 20 dietary carotenoids that can be found in the bloodstream will go through the blood-brain barrier90 (Lindbergh et al., 2018), (Stringham et al., 2019). Astaxanthin is a third one.
They are also present at the highest level of accumulation inside the body. It appears that the brain and retina both actively collect xanthophylls. Lutein is a dominant one. It is likely that low lutein consumption would result in age-related brain and macular degeneration. Much more than other carotenoids.
The Role of Antioxidants in Depression: Clinical Evidence.
In spite of the fact that antidepressants increase oxidative status, and this includes almost all of them that are in use in clinical practice, the complete mechanism of antidepressant action is still not fully explained. The typical theory was formulated around the idea that antidepressants restore neurotransmitter levels to normal and this is a primary theory. They also exhibit antioxidant effects and this is considered to be a secondary effect.
Lithium and valproate, two common medications for bipolar disorder, also have antioxidant qualities.
Supplementation with antioxidants in trichotillomania, a condition related to obsessive-compulsive disorder (OCD), also reported significant improvement in symptoms.
The levels of MDA were dramatically reduced by the selective serotonin reuptake inhibitors (SSRIs) fluoxetine, sertraline, fluvoxamine, paroxetine, and citalopram. Malondialdehyde (MDA) is an end-product formed during oxidative stress, concretely lipid peroxidation. For example, in animal models the increase in brain level of MDA after endotoxin administration was decreased by the lower dose of fluoxetine. At the same time, fluoxetine increased glutathione, suggesting that it has an antioxidant effect on the brain.
Mitochondria is also a prime target for oxidative damage. The role of mitochondria is to burn oxygen or in other words oxidative phosphorylation. This creates energy in form of ATP. Mitochondrial dysfunction is the loss of efficiency in the process of ATP energy production due to oxidative damage. It is considered to be a normal part of the aging process and is effectively correlated to all known chronic diseases including cancer, cardiovascular diseases, and neurodegenerative diseases.
Inhibition of the mitochondrial MAO is one of the most studied effects of antidepressants. MAO activity contributes to mitochondrial dysfunction. Patients suffering from depression, panic disorder, and other anxiety disorders appear to respond well to both selective and nonselective MAO inhibitors. Antidepressants, which primarily function as reuptake inhibitors of serotonin and/or norepinephrine, also inhibit MAO, bringing more validity to the concept of antioxidant action in the treatment of depression and anxiety.
While to a considerably lower extent than in the case of animals, the relationship between anxiety and oxidative stress has been researched in humans as well. Most of the studies were constructed in a way to see if some dietary antioxidants might be prescribed as supportive therapy to standard medication.
The Role of Antioxidants in Anxiety.
My recommendation will be to choose high antioxidant-rich food choices if you can. If you want to eat salad eat kale instead of lettuce. If you want to eat fruit eat berries instead of bananas. If you want a beverage drink hibiscus tea instead of Coke. If you have some pro-inflammatory condition this will improve your health significantly. There are many diseases out there that are caused by inflammation but many people don’t know that they are caused by a bad pro-inflammatory diet.
Depression is just one of them (Rosenblat et al., 2014). For some people, it is bad genetics that plays a role, but for some, it is a bad diet and in both cases, antioxidant-rich food will help. If you suffer from mood disorders disregard USDA recommendations and eat as many antioxidants as you can.
“Accumulating evidence implicates inflammation as a critical mediator in the pathophysiology of mood disorders. Indeed, elevated levels of pro-inflammatory cytokines have been repeatedly demonstrated in both major depressive disorder (MDD) and bipolar disorder (BD) patients. Further, the induction of a pro-inflammatory state in healthy or medically ill subjects induces ‘sickness behavior’ resembling depressive symptomatology. Potential mechanisms involved include, but are not limited to, direct effects of pro-inflammatory cytokines on monoamine levels, dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis, pathologic microglial cell activation, impaired neuroplasticity, and structural and functional brain changes. Anti-inflammatory agents, such as acetylsalicylic acid (ASA), celecoxib, anti-TNF-α agents, minocycline, curcumin, and omega-3 fatty acids, are being investigated for use in mood disorders. Current evidence shows improved outcomes in mood disorder patients when anti-inflammatory agents are used as an adjunct to conventional therapy.“
| Antioxidant effects | Explanation of the effect | Substance | Sources |
|---|---|---|---|
| Modulate neurotransmission | Antioxidants can affect the synthesis, release, uptake, and degradation of neurotransmitters, such as serotonin, dopamine, norepinephrine, and glutamate, that are involved in mood regulation and cognitive function. | Vitamin C, vitamin E, flavonoids, polyphenols | Citrus fruits, berries, nuts, seeds, green tea, dark chocolate |
| Enhance neurogenesis | Antioxidants can stimulate the growth and differentiation of new nerve cells in the brain, especially in the hippocampus, which is responsible for memory and learning. | Vitamin C, vitamin E, β-carotene, polyphenols | Citrus fruits, berries, nuts, seeds, carrots, spinach, broccoli |
| Improve neuroplasticity | Antioxidants can increase the formation and maintenance of synaptic connections between nerve cells in the brain, which allows the brain to adapt and change in response to experience. | Vitamin C, vitamin E, flavonoids, polyphenols | Citrus fruits, berries, nuts, seeds, green tea, dark chocolate |
| Reduce neuroinflammation | Antioxidants can inhibit the activation of immune cells in the brain that can cause tissue damage and impair neuronal function. They can also modulate the production and action of inflammatory cytokines that can affect mood and behavior. | Vitamin C, vitamin E, β-carotene, selenium, CoQ10 | Citrus fruits, berries, nuts, seeds, carrots, spinach, broccoli, Brazil nuts, fish oil |
| Support mitochondrial function | Antioxidants can protect the mitochondria from oxidative damage and enhance their energy production for the cells. Mitochondria are the organelles that produce energy for the cells. They are also involved in apoptosis (programmed cell death) and calcium signaling. | Vitamin C, vitamin E, |
Other studies also found a link between antioxidants and anxiety. Pandya et al. (2013), for example, reviewed the role of antioxidants as potential therapeutic medication. We don’t need to take these medications or wait for the final conclusions. You will just need to increase your consumption of food items that are rich in antioxidants that cross the blood-brain barrier. In the study, they discussed how oxidative stress can cause neuronal damage as well as how antioxidants can modulate the brain’s cellular defense mechanisms, intracellular signaling, and physiological functions.
Another study (Bhattacharya et al., 2012) examined the effect of antioxidant supplementation on patients with generalized anxiety disorder (GAD) and depression.
They found that patients with anxiety and also patients with clinical depression both had significantly lower levels of vitamins A, C, and E in their blood serum.
It seems that both conditions have the same root cause. After giving these patients dietary supplements of these vitamins for six weeks, they observed a significant reduction in their anxiety and depression scores. They also observed a significant increase in the blood levels of antioxidants in patients, except for vitamin E in the depressed group.
These findings indicate the significance of antioxidants in anxiety and other mental health problems. They do, however, highlight some of the difficulties and limits associated with employing antioxidants as treatments, such as dose, bioavailability, interactions, adverse effects, and individual variability.
Depression as an evolutionary protective strategy.
The theory goes that depression is an evolutionary strategy for infection control.
This makes sense if we understand how evolution works. If depression does not have an evolutionary protective role for the species it will be selected against. The high rate of mood disorders in our current society is a consequence of adaptive benefits. The problem is a shift in environment and diet.
If you have a life-threatening virus you will be put into isolation to prevent the spread of infection. Depression does the same thing. In the stone age for example infection was a leading cause of death and more than half of the children died before reaching puberty. Life expectancy was 25 years of age. The theory was made that if one individual gets influenza or some other life-threatening disease the instinct of that individual will be to become irritated, depressed, and antisocial on top of all of the visible signs of sickness.
It is not the pain that causes depression but overall inflammation.
This is bad for individuals but if we look at the overall survival of the species it is beneficial. Individuals that have some sort of health issues and that have inflammation no matter what source of that inflammation might be, will as a theory goes suffer from the additional shift in brain chemistry. That will make them depressed, irritable, and angry as an instinctive underlying mechanism. The purpose is to isolate that individual until the infection is gone so that the spread of infection is minimized.
But what happens if the source of that infection is not some life-threatening virus but a bad and pro-inflammatory diet?
There are animal species like honey bees that will leave to die alone if they are sick. This is not something new. This connection was well known for almost a hundred years now. If doctors give people drugs that induce inflammation depression will be induced as well.
More than 50 percent of people that receive interferon develop severe forms of clinical depression (Pinto et al., 2016), (Su et al., 2019), (Scalori et al.,2005 ).
Lacking an adequate level of antioxidants in a diet plus the addition of all environmental toxins plus dead meat bacteria endotoxins will be pro-inflammatory and depression-inducing. Endotoxins are part of the outer membrane of the cell wall of gram-negative bacteria. They are released from bacteria when they die, their cell walls get destroyed and cannot be cooked away any further. There are a lot of dead bacteria in meat and this is one of the reasons why meat is so pro-inflammatory on top of other factors. We can cook the meat but endotoxins will remain. In experiments done in vivo after injecting endotoxins directly into human subjects, the autoimmune reaction and inflammation were significant and have led to significant increases (from baseline) in IL-6 and TNF-alpha levels as well as feelings of social disconnection and depressed mood.
Also, other experiments proved this through brain imaging. In people injected with endotoxins brain imaging showed a lack of normal excitement to pleasurable stimulation known as anhedonia.
Inflammation changes reward-related neural responses in humans forcing us to become nonresponsive to pleasurable stimulation where we will need stronger stimuli to exert the same effects and then this can create pleasure-seeking behavior, binge eating, and depressed mood.
My recommendation to patients that have any type of mood disorder In addition to healthy guidelines is to try to remove pro-inflammatory foods from their diet and includes all animal products plus a wide range of other vegan products as well and then to dramatically increase the ORAC units score of their diet. Also, you will need to correct vitamin E deficiency, take supplemental astaxanthin and increase lutein and zeaxanthin consumption (kale and spinach).
Limitations of the analysis:
- Dosage and duration: This article does not analyze the dosage or for how long one should take antioxidant supplements. Different antioxidants may have different optimal doses and durations depending on the individual’s needs and health status. For example, one study found that oral vitamin C supplementation of just 500 mg per day for 14 days significantly reduced anxiety levels in students (de Oliveira, et al., 2015). However, this dose and duration may not be suitable for everyone, especially for people that have strong forms of clinical depression. Dosage and duration may also vary depending on factors such as age, weight, diet, and medical conditions.
- Safety and side effects: The possible risks or negative effects of taking antioxidant supplements are not examined in this article. Antioxidants are usually regarded as safe and well-tolerated, but they could still have some unwanted effects or interact negatively with other types of supplements or medications. For example, high doses of vitamin E may increase the risk of bleeding or hemorrhagic stroke. Vitamin C may interfere with some chemotherapy drugs or increase the absorption of iron.
- Other factors: This article does not address any other factors that may contribute to depression and anxiety, such as genetics, environment, lifestyle, or psychological factors. Antioxidants may have some positive impacts on mental health, but they shouldn’t be used as a replacement for a correct diagnosis and effective treatment of underlying causes. A comprehensive strategy is necessary to treat complex and multifactorial disorders such as anxiety and depression. Antioxidants can be used in conjunction with traditional treatments like psychotherapy, medication, or counseling. Therefore, it is important to seek professional help if one suffers from depression and anxiety and follow a comprehensive treatment plan that addresses all aspects of mental well-being.
These studies also have some limitations and controversies that need to be addressed. For example,
- The study by de Oliveira et al. (2015) had a small sample size (n=85), a short duration (14 days), a single dose (500 mg/day), and a single outcome measure (Beck Anxiety Inventory). Moreover, the study did not control for other factors that could influence anxiety levels in students, such as academic stress, sleep quality, diet, exercise, social support, etc.
- The study by Gautam et al. (2012) did not have a placebo group or a blinding procedure, which could introduce bias and confounding. Moreover, the study did not measure the serum levels of antioxidants before and after the intervention, which could indicate the bioavailability and effectiveness of the supplements.
- The meta-analysis by Wang et al. (2022) had a high heterogeneity among the studies in terms of the types, doses, durations, and combinations of antioxidants used, as well as the populations, settings, designs, and outcome measures of the studies. Moreover, the meta-analysis did not perform a quality assessment or a publication bias analysis of the included studies, which could affect the credibility and generalizability of the results.
In addition to antioxidant supplementation, there are other ways to increase antioxidant intake and reduce oxidative stress in the body. Some of these include:
- Eating a balanced diet rich in fruits, vegetables, nuts, seeds, grains, legumes, herbs, and spices that contain various antioxidants, such as vitamin C, vitamin E, β-carotene, flavonoids, polyphenols, etc.
- Avoiding or limiting exposure to sources of oxidative stress, such as pollution, radiation, smoking, alcohol, drugs, etc.
- Engaging in regular physical activity that can enhance antioxidant defense and reduce inflammation in the body.
- Practicing stress management techniques that can lower cortisol levels and improve mood and well-being, such as meditation, yoga, breathing exercises, etc.
- Getting enough sleep and rest that can promote cellular repair and regeneration and prevent oxidative damage.
Antioxidants are not magic bullets that can cure these disorders. They should be used as complementary therapy along with conventional treatments, such as medication and psychotherapy. Moreover, antioxidants should be taken with caution and under the guidance of a healthcare provider, as they may have side effects or interactions with other drugs or conditions. Furthermore, antioxidants should be obtained from a variety of natural sources and not rely solely on supplements. By following these tips, one can optimize their antioxidant intake and reduce their risk of depression and anxiety.
Conclusion:
- Anxiety is very common.
- Anxiety and depression frequently overlap.
- In most cases, depression is caused by chronic inflammation in the brain.
- If you are suffering from chronic hypoglycemia attacks you are also suffering from post-traumatic stress disorder.
- Major depression and anxiety are currently associated with a lowered total antioxidant state.
- It is proven in research that most antidepressants act as antioxidants in the brain and one of the therapeutic effects they exhibit is normalizing the damage caused by oxidative stress.
- Chronic inflammation as a result of oxidative stress is also correlated to neuropathies.
- Even the smallest imbalances in antioxidant defense mechanisms can be lethal to neurons.
- Only lutein and zeaxanthin from more than 20 dietary carotenoids that can be found in the bloodstream will go through the blood-brain barrier. Astaxanthin is a third one.
- Depression is an evolutionary strategy for infection control.
- It is not the pain that causes depression but overall inflammation.
- More than 50 percent of people that receive interferon develop severe forms of clinical depression.
- In people injected with endotoxins brain imaging showed a lack of normal excitement to pleasurable stimulation known as anhedonia.
- Inflammation changes reward-related neural responses in humans forcing us to become nonresponsive to pleasurable stimulation where we will need stronger stimuli to exert the same effects and then this can create pleasure-seeking behavior, binge eating, and depressed mood.
- Patients that have any type of mood disorder need to remove pro-inflammatory foods from their diet and that includes all animal products plus a wide range of other vegan products as well.
- Patients that have any type of mood disorder need to dramatically increase the ORAC units score of their diet.
- Patients that have any type of mood disorder need to correct vitamin E deficiency, take supplemental astaxanthin, and increase lutein and zeaxanthin consumption (kale and spinach).
FAQ
References:
Passages selected from a book: Pokimica, Milos. Go Vegan? Review of Science: Part 3. Kindle Direct Publishing, 2020.
- Xu, Y., Wang, C., Klabnik, J. J., & O’Donnell, J. M. (2014). Novel therapeutic targets in depression and anxiety: antioxidants as a candidate treatment. Current neuropharmacology, 12(2), 108–119. https://doi.org/10.2174/1570159X11666131120231448
- Rosenblat, J. D., Cha, D. S., Mansur, R. B., & McIntyre, R. S. (2014). Inflamed moods: a review of the interactions between inflammation and mood disorders. Progress in neuro-psychopharmacology & biological psychiatry, 53, 23–34. https://doi.org/10.1016/j.pnpbp.2014.01.013
- Anders, S., Tanaka, M., & Kinney, D. K. (2013). Depression as an evolutionary strategy for defense against infection. Brain, behavior, and immunity, 31, 9–22. https://doi.org/10.1016/j.bbi.2012.12.002
- Eisenberger, N. I., Inagaki, T. K., Mashal, N. M., & Irwin, M. R. (2010). Inflammation and social experience: an inflammatory challenge induces feelings of social disconnection in addition to depressed mood. Brain, behavior, and immunity, 24(4), 558–563. https://doi.org/10.1016/j.bbi.2009.12.009
- Ali, S., Corbi, G., Maes, M., Scapagnini, G., & Davinelli, S. (2021). Exploring the Impact of Flavonoids on Symptoms of Depression: A Systematic Review and Meta-Analysis. Antioxidants (Basel, Switzerland), 10(11), 1644. https://doi.org/10.3390/antiox10111644
- Gautam, M., Agrawal, M., Gautam, M., Sharma, P., Gautam, A. S., & Gautam, S. (2012). Role of antioxidants in generalised anxiety disorder and depression. Indian journal of psychiatry, 54(3), 244–247. https://doi.org/10.4103/0019-5545.102424
- de Oliveira, I. J., de Souza, V. V., Motta, V., & Da-Silva, S. L. (2015). Effects of Oral Vitamin C Supplementation on Anxiety in Students: A Double-Blind, Randomized, Placebo-Controlled Trial. Pakistan journal of biological sciences : PJBS, 18(1), 11–18. https://doi.org/10.3923/pjbs.2015.11.18
- Gautam, M., Agrawal, M., Gautam, M., Sharma, P., Gautam, A. S., & Gautam, S. (2012). Role of antioxidants in generalised anxiety disorder and depression. Indian journal of psychiatry, 54(3), 244–247. https://doi.org/10.4103/0019-5545.102424
- Wang, H., Jin, M., Xie, M., Yang, Y., Xue, F., Li, W., Zhang, M., Li, Z., Li, X., Jia, N., Liu, Y., Cui, X., Hu, G., Dong, L., Wang, G., & Yu, Q. (2022). Protective role of antioxidant supplementation for depression and anxiety: A meta-analysis of randomized clinical trials. Journal of Affective Disorders, 323, 264–279. https://doi.org/10.1016/j.jad.2022.11.072
- Pinto, E. F., & Andrade, C. (2016). Interferon-Related Depression: A Primer on Mechanisms, Treatment, and Prevention of a Common Clinical Problem. Current neuropharmacology, 14(7), 743–748. https://doi.org/10.2174/1570159×14666160106155129
- Su, K. P., Lai, H. C., Peng, C. Y., Su, W. P., Chang, J. P., & Pariante, C. M. (2019). Interferon-alpha-induced depression: Comparisons between early- and late-onset subgroups and with patients with major depressive disorder. Brain, behavior, and immunity, 80, 512–518. https://doi.org/10.1016/j.bbi.2019.04.032
- Scalori, A., Pozzi, M., Bellia, V., Apale, P., Santamaria, G., Bordoni, T., Redaelli, A., Avolio, A., Parravicini, P., Pioltelli, P., & Roffi, L. (2005). Interferon-induced depression: prevalence and management. Digestive and liver disease : official journal of the Italian Society of Gastroenterology and the Italian Association for the Study of the Liver, 37(2), 102–107. https://doi.org/10.1016/j.dld.2004.09.018
- Steel, Z., Marnane, C., Iranpour, C., Chey, T., Jackson, J. W., Patel, V., & Silove, D. (2014). The global prevalence of common mental disorders: a systematic review and meta-analysis 1980-2013. International journal of epidemiology, 43(2), 476–493. https://doi.org/10.1093/ije/dyu038
- Ettman, C. K., Abdalla, S. M., Cohen, G. H., Sampson, L., Vivier, P. M., & Galea, S. (2020). Prevalence of Depression Symptoms in US Adults Before and During the COVID-19 Pandemic. JAMA network open, 3(9), e2019686. https://doi.org/10.1001/jamanetworkopen.2020.19686
- Lindbergh, C. A., Renzi-Hammond, L. M., Hammond, B. R., Terry, D. P., Mewborn, C. M., Puente, A. N., & Miller, L. S. (2018). Lutein and Zeaxanthin Influence Brain Function in Older Adults: A Randomized Controlled Trial. Journal of the International Neuropsychological Society : JINS, 24(1), 77–90. https://doi.org/10.1017/S1355617717000534
- Stringham, J. M., Johnson, E. J., & Hammond, B. R. (2019). Lutein across the Lifespan: From Childhood Cognitive Performance to the Aging Eye and Brain. Current developments in nutrition, 3(7), nzz066. https://doi.org/10.1093/cdn/nzz066
- Pandya, C. D., Howell, K. R., & Pillai, A. (2013). Antioxidants as potential therapeutics for neuropsychiatric disorders. Progress in neuro-psychopharmacology & biological psychiatry, 46, 214–223. https://doi.org/10.1016/j.pnpbp.2012.10.017
- Gautam, M., Agrawal, M., Gautam, M., Sharma, P., Gautam, A. S., & Gautam, S. (2012). Role of antioxidants in generalised anxiety disorder and depression. Indian journal of psychiatry, 54(3), 244–247. https://doi.org/10.4103/0019-5545.102424
Related Posts
Do you have any questions about nutrition and health?
I would love to hear from you and answer them in my next post. I appreciate your input and opinion and I look forward to hearing from you soon. I also invite you to follow us on Facebook, Instagram, and Pinterest for more diet, nutrition, and health content. You can leave a comment there and connect with other health enthusiasts, share your tips and experiences, and get support and encouragement from our team and community.
I hope that this post was informative and enjoyable for you and that you are prepared to apply the insights you learned. If you found this post helpful, please share it with your friends and family who might also benefit from it. You never know who might need some guidance and support on their health journey.
– You Might Also Like –

Learn About Nutrition
Milos Pokimica is a doctor of natural medicine, clinical nutritionist, medical health and nutrition writer, and nutritional science advisor. Author of the book series Go Vegan? Review of Science, he also operates the natural health website GoVeganWay.com
Medical Disclaimer
GoVeganWay.com brings you reviews of the latest nutrition and health-related research. The information provided represents the personal opinion of the author and is not intended nor implied to be a substitute for professional medical advice, diagnosis, or treatment. The information provided is for informational purposes only and is not intended to serve as a substitute for the consultation, diagnosis, and/or medical treatment of a qualified physician or healthcare provider.NEVER DISREGARD PROFESSIONAL MEDICAL ADVICE OR DELAY SEEKING MEDICAL TREATMENT BECAUSE OF SOMETHING YOU HAVE READ ON OR ACCESSED THROUGH GoVeganWay.com
NEVER APPLY ANY LIFESTYLE CHANGES OR ANY CHANGES AT ALL AS A CONSEQUENCE OF SOMETHING YOU HAVE READ IN GoVeganWay.com BEFORE CONSULTING LICENCED MEDICAL PRACTITIONER.
In the event of a medical emergency, call a doctor or 911 immediately. GoVeganWay.com does not recommend or endorse any specific groups, organizations, tests, physicians, products, procedures, opinions, or other information that may be mentioned inside.
Editor Picks –
Milos Pokimica is a health and nutrition writer and nutritional science advisor. Author of the book series Go Vegan? Review of Science, he also operates the natural health website GoVeganWay.com
Latest Articles –
Top Health News — ScienceDaily
- The overlooked nutrition risk of Ozempic and Wegovyon February 4, 2026
Popular weight-loss drugs like Ozempic and Wegovy can dramatically curb appetite, but experts warn many users are flying blind when it comes to nutrition. New research suggests people taking these medications may not be getting enough guidance on protein, vitamins, and overall diet quality, increasing the risk of muscle loss and nutrient deficiencies.
- A 25-year study found an unexpected link between cheese and dementiaon February 4, 2026
A massive Swedish study tracking nearly 28,000 people for 25 years found an unexpected link between full-fat dairy and brain health. Among adults without a genetic risk for Alzheimer’s, eating more full-fat cheese was associated with a noticeably lower risk of developing the disease, while higher cream intake was tied to reduced dementia risk overall. The findings challenge decades of low-fat dietary advice but come with important caveats.
- MIT’s new brain tool could finally explain consciousnesson February 4, 2026
Scientists still don’t know how the brain turns physical activity into thoughts, feelings, and awareness—but a powerful new tool may help crack the mystery. Researchers at MIT are exploring transcranial focused ultrasound, a noninvasive technology that can precisely stimulate deep regions of the brain that were previously off-limits. In a new “roadmap” paper, they explain how this method could finally let scientists test cause-and-effect in consciousness research, not just observe […]
- Why heart disease risk in type 2 diabetes looks different for men and womenon February 4, 2026
Scientists are digging into why heart disease risk in type 2 diabetes differs between men and women—and sex hormones may be part of the story. In a large Johns Hopkins study, men with higher testosterone had lower heart disease risk, while rising estradiol levels were linked to higher risk. These hormone effects were not seen in women. The results point toward more personalized approaches to heart disease prevention in diabetes.
- Sound machines might be making your sleep worseon February 4, 2026
Sound machines may not be the sleep saviors many believe. Researchers found that pink noise significantly reduced REM sleep, while simple earplugs did a better job protecting deep, restorative sleep from traffic noise. When pink noise was combined with outside noise, sleep quality dropped even further. The results suggest that popular “sleep sounds” could be doing more harm than good—particularly for kids.
- This unexpected plant discovery could change how drugs are madeon February 3, 2026
Plants make chemical weapons to protect themselves, and many of these compounds have become vital to human medicine. Researchers found that one powerful plant chemical is produced using a gene that looks surprisingly bacterial. This suggests plants reuse microbial tools to invent new chemistry. The insight could help scientists discover new drugs and produce them more sustainably.
- A hidden cellular process may drive aging and diseaseon February 3, 2026
As we age, our cells don’t just wear down—they reorganize. Researchers found that cells actively remodel a key structure called the endoplasmic reticulum, reducing protein-producing regions while preserving fat-related ones. This process, driven by ER-phagy, is tied to lifespan and healthy aging. Because these changes happen early, they could help trigger later disease—or offer a chance to stop it.
PubMed, #vegan-diet –
- Diet type and the oral microbiomeon February 2, 2026
CONCLUSION: The diet-oral microbiome-systemic inflammation axis is bidirectional and clinically relevant. Understanding both direct ecological regulation and indirect metabolic effects is essential to support precision nutrition strategies aimed at maintaining oral microbial balance and systemic inflammatory risk mitigation.
- Consensus document on healthy lifestyleson January 22, 2026
Proteins are a group of macronutrients that are vital to our lives, as they perform various functions, including structural, defensive and catalytic. An intake of 1.0-1.2 g/kg/body weight per day would be sufficient to meet our needs. Carbohydrate requirements constitute 50 % of the total caloric value and should be obtained mainly in the form of complex carbohydrates. In addition, a daily intake of both soluble and insoluble fiber is necessary. Regular consumption of extra virgin olive oil […]
- Vitamin B12 and D status in long-term vegetarians: Impact of diet duration and subtypes in Beijing, Chinaon January 21, 2026
CONCLUSIONS: This study reveals a dual challenge among Beijing long-term vegetarians: vitamin B12 deficiency was strongly associated with the degree of exclusion of animal products from the diet (veganism), while vitamin D deficiency was highly prevalent and worsened with longer diet duration. The near-universal vitamin D deficiency observed in this study suggests that, in the Beijing context, the risk may extend beyond dietary choice, potentially reflecting regional environmental factors;…
- Nutritional evaluation of duty meals provided to riot police forces in Germanyon January 13, 2026
Background: The primary role of the German riot police is maintaining internal security. Due to challenging working conditions, riot police forces face an elevated risk of various diseases. During duty, forces are provided with meals. A balanced diet can reduce the risk of some of these diseases and contribute to health-promoting working conditions. Aim: First evaluation of the nutritional quality of duty meals in Germany based on German Nutrition Society recommendations (DGE). Methods: In…
- Iodineon January 1, 2006
Iodine is an essential trace nutrient for all infants that is a normal component of breastmilk. Infant requirements are estimated to be 15 mcg/kg daily in full-term infants and 30 mcg/kg daily in preterm infants.[1] Breastmilk iodine concentration correlates well with maternal urinary iodine concentration and may be a useful index of iodine sufficiency in infants under 2 years of age, but there is no clear agreement on a value that indicates iodine sufficiency, and may not correlate with […]
Random Posts –
Featured Posts –
Latest from PubMed, #plant-based diet –
- From paddy soil to dining table: biological biofortification of rice with zincby Lei Huang on February 4, 2026
One-third of paddy soils are globally deficient in zinc (Zn) and 40% of Zn loss in the procession from brown rice to polished rice, which results in the global issue of hidden hunger, e.g., the micronutrient deficiencies in the rice-based population of developing countries. In the recent decades, biofortification of cereal food crops with Zn has emerged as a promising solution. Herein, we comprehensively reviewed the entire process of Zn in paddy soil to human diet, including the regulatory…
- Molecular Characterization of Tobacco Necrosis Virus A Variants Identified in Sugarbeet Rootsby Alyssa Flobinus on February 3, 2026
Sugarbeet provides an important source of sucrose; a stable, environmentally safe, and low-cost staple in the human diet. Viral diseases arising in sugarbeet ultimately impact sugar content, which translates to financial losses for growers. To manage diseases and prevent such losses from occurring, it is essential to characterize viruses responsible for disease. Recently, our laboratory identified a tobacco necrosis virus A variant named Beta vulgaris alphanecrovirus 1 (BvANV-1) in sugarbeet…
- Nutrition in early life interacts with genetic risk to influence preadult behaviour in the Raine Studyby Lars Meinertz Byg on February 3, 2026
CONCLUSIONS: Nutrition in early life and psychiatric genetic risk may interact to determine lasting child behaviour. Contrary to our hypothesis, we find dietary benefits in individuals with lower ADHD PGS, necessitating replication. We also highlight the possibility of including genetics in early nutrition intervention trials for causal inference.
- Effect of the gut microbiota on insect reproduction: mechanisms and biotechnological prospectsby Dilawar Abbas on February 2, 2026
The insect gut microbiota functions as a multifunctional symbiotic system that plays a central role in host reproduction. Through the production of bioactive metabolites, gut microbes interact with host hormonal pathways, immune signaling, and molecular regulatory networks, thereby shaping reproductive physiology and fitness. This review summarizes recent advances in understanding how gut microbiota regulate insect reproduction. Accumulating evidence demonstrates that microbial metabolites…
- Rationale and design of a parallel randomised trial of a plant-based intensive lifestyle intervention for diabetes remission: The REmission of diabetes using a PlAnt-based weight loss InteRvention…by Brighid McKay on February 2, 2026
CONCLUSIONS: This trial will provide high-quality clinical evidence on the use of plant-based ILIs to address the epidemics of obesity and diabetes to inform public health policies and programs in Canada and beyond.
- Diet type and the oral microbiomeby Daniel Betancur on February 2, 2026
CONCLUSION: The diet-oral microbiome-systemic inflammation axis is bidirectional and clinically relevant. Understanding both direct ecological regulation and indirect metabolic effects is essential to support precision nutrition strategies aimed at maintaining oral microbial balance and systemic inflammatory risk mitigation.