Vitamin D deficiency- The optimization strategies
With vitamin D deficiency we will suffer from a wide range of health issues even if we don’t have a directly visible bone disease.
Milos Pokimica
Written By: Milos Pokimica
Medically Reviewed by: Dr. Xiùying Wáng, M.D.
Updated June 9, 2023Vitamin D is an essential vitamin with many different functions. It is a prohormone, steroid with a hormone-like activity that regulates about 3% of the human genome (Carlberg, 2019). More than 2,000 genes overall. It is essential for different life functions, for instance, one of them is calcium development. Besides calcium metabolism, immune system regulation will be one of vitamin D’s most essential functions. Science so far doesn’t have research for every gene that vitamin D can activate but it is important to understand that without vitamin D level optimization even if we don’t have blatant vitamin D deficiency, we will suffer from a wide range of health issues even if we don’t have a directly visible bone disease. Vitamin D deficiency is a worst-case scenario.
Also, we need to understand that optimizing vitamin D levels is important for the long-term prevention of osteoporosis. Osteoporosis starts long before and lasts for a long time until the visible effects can be diagnosed. Having high bone density in younger years and preventing vitamin D deficiency throughout our entire life will have an impact on bone density in old age. Visible symptoms of vitamin D deficiency rickets that include bone deformities and bone pain, slow growth, fractures, and seizures are already the last stages of chronic deficiency disease. It cannot be cured with vitamin D supplementation and with additional calcium because the damage is already done. Prevention is the only way. The way osteoporosis can be treated is with additional medications that will promote calcium metabolism in the bones. Problem is that taking medication for osteoporosis has other side effects. Some medication like Reclast (zoledronic acid) is even taken intravenously every two years to help prevent it. Vitamin D is a vitamin and that means it is essential for life there is no way that we can avoid that simple fact even if we disregard the effects it has on bone disease. Not optimizing our vitamin D levels is the same as having any other nutrient deficiency of any other essential nutrient with one difference and that is that it takes a little longer time for its effects to be visible but at the same time once when we lose our bone density it is hard to bring it back.
There is one other difference between vitamin D and every other essential nutrient. That difference is that we create our own vitamin D if we have sun exposure so we do not need to ingest it in the food. There is some vitamin D in the foods that we eat and some food products are fortified with it but the level of fortification is not at the optimal level and vitamin D deficiency is rampant in most of the population. In the US around 40% of the population is in the severe vitamin D deficiency category and more than 85% are in the insufficient level category (Carlberg, 2019). Most likely if you do not have a severe deficiency you will still lack an adequate and optimal level of vitamin D for normal body functioning. What causes vitamin D deficiency is a modern way of life, it is a form of maladaptation to our current environment.
So the question arises, how much do we need for optimal health optimization?
In the medical field usual scientific practice is to recommend nutrition intake at the levels that are needed to prevent the disease. It is not an accepted scientific method to recommend the levels that are the most optimal and that we are adapted to in our evolution. It is only the levels that scientists believe are necessary to prevent a pure form of vitamin D deficiency.
Up until recently, the official RDA for vitamin D was considered to be 200 international units a day and that was an average intake for most people. And before that, there was an accepted belief that 100 IU of vitamin D3 is enough to prevent flagrant signs and symptoms of rickets. Because the number of 100 units was enough to prevent bone disease scientists with no real experimentation recommended 200 units just to be safe. They believed that that was more than adequate to satisfy the body’s vitamin D requirement. Then there was a line of experiments when the Institute of Medicine decided to make a recommendation on specific blood levels of vitamin D that should prevent rickets. They calculated that to get to this level most people would require about 600 IUs a day.
Today the RDA is 600 IU a day and that is an official recommendation. With this new RDA, around 40% of Americans still have vitamin D deficiency. The problem is that even these 600 IU’s are far less than what would be the most optimal level in an evolutionary sense. The level that will promote the most health and longevity effects. One way the medicine can determent the most optimal level is by testing for the hormone in the blood called PTH. Our bodies secrete PTH in situations when the body detects that we don’t have adequate levels of active vitamin D3 for bone metabolism in an effort to raise its levels. When levels in the bloodstream go below 20 nanograms/ml our body will start to produce PTH to protect our bones from softening. And this is just bones.
Vitamin D affects our entire genome and most of the organs and their functioning from the brain to muscle tissue. Measuring just its effects on calcium metabolism is still not the optimal strategy.
“Body requires 5- to 10-fold higher intakes than is currently recommended by health agencies. There is now overwhelming and compelling scientific and epidemiologic data suggesting that the human body requires a blood level of 25(OH)D above 30 ng/mL for maximum health. To increase the blood level to the minimum 30 ng/mL requires the ingestion of at least 1000 IU of vitamin D per day for adults.”
(Holick, 2010)
It is also important for immune system function and prevention of autoimmune diseases from allergies to asthma to multiple sclerosis, prevention of cancers of a different type, periodontal disease prevention, depression, obesity, diabetes type 2, and overall mortality. (Glade, 2013)
“Adequate vitamin D status seems to be protective against musculoskeletal disorders (muscle weakness, falls, fractures), infectious diseases, autoimmune diseases, cardiovascular disease, type 1 and type 2 diabetes mellitus, several types of cancer, neurocognitive dysfunction and mental illness, and other diseases, as well as infertility and adverse pregnancy and birth outcomes. Vitamin D deficiency/insufficiency is associated with all-cause mortality.”
(Pludowski et al., 2013)
At one point in the 20th century, even wire cages were affixed to tenement buildings so that people can put babies in there so that babies could benefit from the sun.
Beyond rickets prevention, if we manage to prevent all of the diseases that are caused by vitamin D deficiency, it is still important vitamin for all-cause mortality, meaning it will promote longevity even if we don’t have any disease risk. We will live longer if we have normal and optimized levels. But what exactly are the optimal levels? One way is to measure the level of vitamin D and compare it to different rates of diseases but that does not directly mean that is the optimal level because it is just observation. Vitamin D deficiency might not be the cause. What is needed is clinical trials where you give people D supplements to prove that vitamin D is effective.
In the last 50 years, there are hundreds of clinical trials involving more than 100,000 people so we have the knowledge now. Vitamin D does help in disease prevention, it does promote longevity and it is cheap. The effects are also potent for example 13% in terms of reduction of total mortality (Chowdhury, 2014). The level of reduction that everyday exercise will cause is 11% so the effects are even more pronounced than everyday exercise. Also, the effect is cumulative. And also this is on top of all the benefits we will have on chronic diseases that can deteriorate the quality of life and are not life-threatening like allergies for example. Keep in mind that taking supplemental vitamin D is no excuse to eat one more donut. Healthy eating will have a cumulative effect on vitamin D optimization. In most studies, the levels of vitamin D are also not completely optimized so the reduction in mortality can be higher if we take an adequate level of supplementation. Also, the positive effects are only correlated with supplementation with active D3 type. It is the type derived from plants and animals and not vitamin D2, the type derived from mushrooms.
So how much? The answer is it depends. Two different individuals can get the same dose but will have different levels in the bloodstream. Then it depends on sun exposure, it depends on dietary intake. The optimal level of supplementation can be only measured with a blood test in individual cases. When scientists give recommendations they will be based on relative numbers for the percentage of the population. For example, they will say take “this” amount of it and 3 out of 5 people will have more “that” that level in the bloodstream. It is not the rule but more in line with recommendations. You will have to do a blood test if you want to know the exact level in your blood.
The problem with vitamins is that you can take too much. In the case of vitamin D and its benefits is not as dangerous vitamin as vitamin A for example. If you overdose on vitamin A you can have serious problems. For example, supplemental vitamin E promotes cancer while dietary vitamin E prevents cancer even at the optimal level. We have to analyze the optimal level and then we have to find the optimal supplementation strategy that will in our individual case put us to that optimal level.
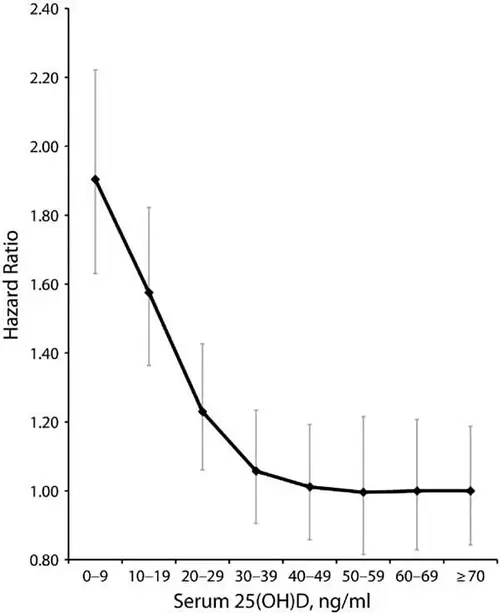
With vitamin D it was believed to be a U shape curve. Most of the benefits in the studies will get at around 70 to 80 nmol/L (Bischoff-Ferrari, 2008). This is the optimal level in the blood. For cancer prevention, the level can be as high as 90-120 nmol/l. More than that will have no additional health benefits. Also, very high levels are correlated with a slight increase in mortality. The risk and increase are not substantial but the apparent sweet spot is around 75 or 80 nanomoles per liter [nmol/L] and more than that you will just be wasting money.
Because vitamin D is a hormone not a vitamin per se there was a debate in the scientific community about its toxic level. The good news is that in order to go to the toxic level we will have to do a serious supplemental overdosing in levels of more than 10,000 IU a day for an extended period. In real-life conditions, although it is still a U-shaped curve it is practically an L curve (Garland et al., 2014).
We can get to an optimal dose without the risk of overdosing and that is good news. We don’t have to do testing and worry about overdose as long as we don’t go above the levels of 10,000 IU a day for an extended period of time. Testing is not recommended and it is not necessary, it is expensive and not accurate. If you do testing there will be a variation in results from 2 to 5 times in different laboratories. You can get a result of 30 ng/ml or 120 ng/ml. In all practical sense, testing is useless. So how much should we take?
An intake of no less than 1000 IU of vitamin D3 (cholecalciferol) per day for all adults may bring at least 50% of the population up to 75 nmol/l (30ng/ml). This means 5 out of 10 people will be at an optimal level depending on their skin color, level of sun exposure, and dietary intake and this is for a population in the US. Because essentially there is no risk of excessive intake of vitamin D the supplementation for 100 percent of the population for everyone to be in the optimal range including individuals with zero sun exposure and zero dietary intake, the dose will be 2200IU. For most of the population anywhere in the world to have a value of 80nmol/L or higher may require a daily oral intake of 2200IU.
Because the government doesn’t want people to overdose themselves even if there is no real risk the tolerable upper intake level is currently set at 2000IU/day.
Actual toxicity is not seen below serum values of 250nmol/L, a value that would be produced only at continuing oral intakes in excess of 10,000IU/day.
The margin of toxicity is extensive. So how much should you take? Because it is one of the cheapest supplements the answer is at least 2200IU a day and more if you are obese and more the older you are. If you are 70 years old you will need 3,500IU to reach the same level.
There might be some risks of toxicity if you overdose that science has not determent yet especially in you have some sort of condition. It also has the potential to lower vitamin A levels. That is the reason you don’t want to overdose. There is no need for it. But again overdosing on vitamin D is very hard to do. For example, in a situation where we are exposed to the sun, our body is able to create thousands of units of it in minutes and is able to store it as well. We cannot naturally overdose ourselves with sun exposure. It will just be stored for later use. That means our body will be able to mobilize its own reserves if our daily intake falters temporarily. It is an oil-soluble vitamin and that is the reason obese people need more, in some cases two times more of it to reach the same blood levels. It is a reason for wide confusion and public recommendations that can range from 600IU to 10,000IU.
References:
- Carlberg C. (2019). Nutrigenomics of Vitamin D. Nutrients, 11(3), 676. https://doi.org/10.3390/nu11030676
- Parva, N. R., Tadepalli, S., Singh, P., Qian, A., Joshi, R., Kandala, H., Nookala, V. K., & Cheriyath, P. (2018). Prevalence of Vitamin D Deficiency and Associated Risk Factors in the US Population (2011-2012). Cureus, 10(6), e2741. https://doi.org/10.7759/cureus.2741
- Holick M. F. (2010). Vitamin D: extraskeletal health. Endocrinology and metabolism clinics of North America, 39(2), . https://doi.org/10.1016/j.ecl.2010.02.016
- Glade M. J. (2013). Vitamin D: health panacea or false prophet?. Nutrition (Burbank, Los Angeles County, Calif.), 29(1), 37–41. https://doi.org/10.1016/j.nut.2012.05.010
- Pludowski, P., Holick, M. F., Pilz, S., Wagner, C. L., Hollis, B. W., Grant, W. B., Shoenfeld, Y., Lerchbaum, E., Llewellyn, D. J., Kienreich, K., & Soni, M. (2013). Vitamin D effects on musculoskeletal health, immunity, autoimmunity, cardiovascular disease, cancer, fertility, pregnancy, dementia and mortality-a review of recent evidence. Autoimmunity reviews, 12(10), 976–989. https://doi.org/10.1016/j.autrev.2013.02.004
- Chowdhury, R. (2014). Vitamin D and risk of cause specific death: systematic review and meta-analysis of observational cohort and randomised intervention studies. Database of Abstracts of Reviews of Effects (DARE): Quality-assessed Reviews – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK200718/
- Bischoff-Ferrari H. A. (2008). Optimal serum 25-hydroxyvitamin D levels for multiple health outcomes. Advances in experimental medicine and biology, 624, 55–71. https://doi.org/10.1007/978-0-387-77574-6_5
- Garland, C. F., Kim, J. J., Mohr, S. B., Gorham, E. D., Grant, W. B., Giovannucci, E. L., Baggerly, L., Hofflich, H., Ramsdell, J. W., Zeng, K., & Heaney, R. P. (2014). Meta-analysis of all-cause mortality according to serum 25-hydroxyvitamin D. American journal of public health, 104(8), e43–e50. https://doi.org/10.2105/AJPH.2014.302034
Do you have any questions about nutrition and health?
I would love to hear from you and answer them in my next post. I appreciate your input and opinion and I look forward to hearing from you soon. I also invite you to follow us on Facebook, Instagram, and Pinterest for more diet, nutrition, and health content. You can leave a comment there and connect with other health enthusiasts, share your tips and experiences, and get support and encouragement from our team and community.
I hope that this post was informative and enjoyable for you and that you are prepared to apply the insights you learned. If you found this post helpful, please share it with your friends and family who might also benefit from it. You never know who might need some guidance and support on their health journey.
– You Might Also Like –

Learn About Nutrition
Milos Pokimica is a doctor of natural medicine, clinical nutritionist, medical health and nutrition writer, and nutritional science advisor. Author of the book series Go Vegan? Review of Science, he also operates the natural health website GoVeganWay.com
Medical Disclaimer
GoVeganWay.com brings you reviews of the latest nutrition and health-related research. The information provided represents the personal opinion of the author and is not intended nor implied to be a substitute for professional medical advice, diagnosis, or treatment. The information provided is for informational purposes only and is not intended to serve as a substitute for the consultation, diagnosis, and/or medical treatment of a qualified physician or healthcare provider.NEVER DISREGARD PROFESSIONAL MEDICAL ADVICE OR DELAY SEEKING MEDICAL TREATMENT BECAUSE OF SOMETHING YOU HAVE READ ON OR ACCESSED THROUGH GoVeganWay.com
NEVER APPLY ANY LIFESTYLE CHANGES OR ANY CHANGES AT ALL AS A CONSEQUENCE OF SOMETHING YOU HAVE READ IN GoVeganWay.com BEFORE CONSULTING LICENCED MEDICAL PRACTITIONER.
In the event of a medical emergency, call a doctor or 911 immediately. GoVeganWay.com does not recommend or endorse any specific groups, organizations, tests, physicians, products, procedures, opinions, or other information that may be mentioned inside.
Editor Picks –
Milos Pokimica is a health and nutrition writer and nutritional science advisor. Author of the book series Go Vegan? Review of Science, he also operates the natural health website GoVeganWay.com
Latest Articles –
Top Health News — ScienceDaily
- The overlooked nutrition risk of Ozempic and Wegovyon February 4, 2026
Popular weight-loss drugs like Ozempic and Wegovy can dramatically curb appetite, but experts warn many users are flying blind when it comes to nutrition. New research suggests people taking these medications may not be getting enough guidance on protein, vitamins, and overall diet quality, increasing the risk of muscle loss and nutrient deficiencies.
- A 25-year study found an unexpected link between cheese and dementiaon February 4, 2026
A massive Swedish study tracking nearly 28,000 people for 25 years found an unexpected link between full-fat dairy and brain health. Among adults without a genetic risk for Alzheimer’s, eating more full-fat cheese was associated with a noticeably lower risk of developing the disease, while higher cream intake was tied to reduced dementia risk overall. The findings challenge decades of low-fat dietary advice but come with important caveats.
- MIT’s new brain tool could finally explain consciousnesson February 4, 2026
Scientists still don’t know how the brain turns physical activity into thoughts, feelings, and awareness—but a powerful new tool may help crack the mystery. Researchers at MIT are exploring transcranial focused ultrasound, a noninvasive technology that can precisely stimulate deep regions of the brain that were previously off-limits. In a new “roadmap” paper, they explain how this method could finally let scientists test cause-and-effect in consciousness research, not just observe […]
- Why heart disease risk in type 2 diabetes looks different for men and womenon February 4, 2026
Scientists are digging into why heart disease risk in type 2 diabetes differs between men and women—and sex hormones may be part of the story. In a large Johns Hopkins study, men with higher testosterone had lower heart disease risk, while rising estradiol levels were linked to higher risk. These hormone effects were not seen in women. The results point toward more personalized approaches to heart disease prevention in diabetes.
- Sound machines might be making your sleep worseon February 4, 2026
Sound machines may not be the sleep saviors many believe. Researchers found that pink noise significantly reduced REM sleep, while simple earplugs did a better job protecting deep, restorative sleep from traffic noise. When pink noise was combined with outside noise, sleep quality dropped even further. The results suggest that popular “sleep sounds” could be doing more harm than good—particularly for kids.
- This unexpected plant discovery could change how drugs are madeon February 3, 2026
Plants make chemical weapons to protect themselves, and many of these compounds have become vital to human medicine. Researchers found that one powerful plant chemical is produced using a gene that looks surprisingly bacterial. This suggests plants reuse microbial tools to invent new chemistry. The insight could help scientists discover new drugs and produce them more sustainably.
- A hidden cellular process may drive aging and diseaseon February 3, 2026
As we age, our cells don’t just wear down—they reorganize. Researchers found that cells actively remodel a key structure called the endoplasmic reticulum, reducing protein-producing regions while preserving fat-related ones. This process, driven by ER-phagy, is tied to lifespan and healthy aging. Because these changes happen early, they could help trigger later disease—or offer a chance to stop it.
PubMed, #vegan-diet –
- Diet type and the oral microbiomeon February 2, 2026
CONCLUSION: The diet-oral microbiome-systemic inflammation axis is bidirectional and clinically relevant. Understanding both direct ecological regulation and indirect metabolic effects is essential to support precision nutrition strategies aimed at maintaining oral microbial balance and systemic inflammatory risk mitigation.
- Consensus document on healthy lifestyleson January 22, 2026
Proteins are a group of macronutrients that are vital to our lives, as they perform various functions, including structural, defensive and catalytic. An intake of 1.0-1.2 g/kg/body weight per day would be sufficient to meet our needs. Carbohydrate requirements constitute 50 % of the total caloric value and should be obtained mainly in the form of complex carbohydrates. In addition, a daily intake of both soluble and insoluble fiber is necessary. Regular consumption of extra virgin olive oil […]
- Vitamin B12 and D status in long-term vegetarians: Impact of diet duration and subtypes in Beijing, Chinaon January 21, 2026
CONCLUSIONS: This study reveals a dual challenge among Beijing long-term vegetarians: vitamin B12 deficiency was strongly associated with the degree of exclusion of animal products from the diet (veganism), while vitamin D deficiency was highly prevalent and worsened with longer diet duration. The near-universal vitamin D deficiency observed in this study suggests that, in the Beijing context, the risk may extend beyond dietary choice, potentially reflecting regional environmental factors;…
- Nutritional evaluation of duty meals provided to riot police forces in Germanyon January 13, 2026
Background: The primary role of the German riot police is maintaining internal security. Due to challenging working conditions, riot police forces face an elevated risk of various diseases. During duty, forces are provided with meals. A balanced diet can reduce the risk of some of these diseases and contribute to health-promoting working conditions. Aim: First evaluation of the nutritional quality of duty meals in Germany based on German Nutrition Society recommendations (DGE). Methods: In…
- Iodineon January 1, 2006
Iodine is an essential trace nutrient for all infants that is a normal component of breastmilk. Infant requirements are estimated to be 15 mcg/kg daily in full-term infants and 30 mcg/kg daily in preterm infants.[1] Breastmilk iodine concentration correlates well with maternal urinary iodine concentration and may be a useful index of iodine sufficiency in infants under 2 years of age, but there is no clear agreement on a value that indicates iodine sufficiency, and may not correlate with […]
Random Posts –
Featured Posts –
Latest from PubMed, #plant-based diet –
- From paddy soil to dining table: biological biofortification of rice with zincby Lei Huang on February 4, 2026
One-third of paddy soils are globally deficient in zinc (Zn) and 40% of Zn loss in the procession from brown rice to polished rice, which results in the global issue of hidden hunger, e.g., the micronutrient deficiencies in the rice-based population of developing countries. In the recent decades, biofortification of cereal food crops with Zn has emerged as a promising solution. Herein, we comprehensively reviewed the entire process of Zn in paddy soil to human diet, including the regulatory…
- Molecular Characterization of Tobacco Necrosis Virus A Variants Identified in Sugarbeet Rootsby Alyssa Flobinus on February 3, 2026
Sugarbeet provides an important source of sucrose; a stable, environmentally safe, and low-cost staple in the human diet. Viral diseases arising in sugarbeet ultimately impact sugar content, which translates to financial losses for growers. To manage diseases and prevent such losses from occurring, it is essential to characterize viruses responsible for disease. Recently, our laboratory identified a tobacco necrosis virus A variant named Beta vulgaris alphanecrovirus 1 (BvANV-1) in sugarbeet…
- Nutrition in early life interacts with genetic risk to influence preadult behaviour in the Raine Studyby Lars Meinertz Byg on February 3, 2026
CONCLUSIONS: Nutrition in early life and psychiatric genetic risk may interact to determine lasting child behaviour. Contrary to our hypothesis, we find dietary benefits in individuals with lower ADHD PGS, necessitating replication. We also highlight the possibility of including genetics in early nutrition intervention trials for causal inference.
- Effect of the gut microbiota on insect reproduction: mechanisms and biotechnological prospectsby Dilawar Abbas on February 2, 2026
The insect gut microbiota functions as a multifunctional symbiotic system that plays a central role in host reproduction. Through the production of bioactive metabolites, gut microbes interact with host hormonal pathways, immune signaling, and molecular regulatory networks, thereby shaping reproductive physiology and fitness. This review summarizes recent advances in understanding how gut microbiota regulate insect reproduction. Accumulating evidence demonstrates that microbial metabolites…
- Rationale and design of a parallel randomised trial of a plant-based intensive lifestyle intervention for diabetes remission: The REmission of diabetes using a PlAnt-based weight loss InteRvention…by Brighid McKay on February 2, 2026
CONCLUSIONS: This trial will provide high-quality clinical evidence on the use of plant-based ILIs to address the epidemics of obesity and diabetes to inform public health policies and programs in Canada and beyond.
- Diet type and the oral microbiomeby Daniel Betancur on February 2, 2026
CONCLUSION: The diet-oral microbiome-systemic inflammation axis is bidirectional and clinically relevant. Understanding both direct ecological regulation and indirect metabolic effects is essential to support precision nutrition strategies aimed at maintaining oral microbial balance and systemic inflammatory risk mitigation.