Homemade Natural Mouthwash: Proven, Stronger & Less Toxic
Homemade natural mouthwash is stronger than chlorhexidine, less toxic and if swallowed might give you some nausea but also a high burst in ORAC value.
Milos Pokimica
Written By: Milos Pokimica
Medically Reviewed by: Dr. Xiùying Wáng, M.D.
Updated January 8, 2024Key Takeaways:
– Chlorhexidine is an antiseptic agent that can kill many kinds of germs and prevent them from growing back. It is used as a standard antiseptic for commercial mouthwashes.
– Some studies have suggested that chlorhexidine may have genotoxic effects. Tests have shown that chlorhexidine can induce DNA damage in various organs and tissues, such as leukocytes (white blood cells), liver, kidney, and oral mucosa (the lining of the mouth) (Ribeiro, 2008).
– Chlorhexidine can also affect liver and energy metabolism.
– The chlorhexidine mouthwash reduced the oral nitrite production by 90% and the plasma nitrite levels by 25%. Oral bacteria have the ability to reduce nitrate to nitrite, which is then swallowed and absorbed into the bloodstream. This was associated with an increase in blood pressure.
– Green tea has been shown to have anti-inflammatory, antibacterial, and anticarcinogenic properties, which may help prevent or treat periodontitis and caries.
– Green tea treatment had a large positive effect size in reducing Streptococcus mutans, which is a major cause of caries.
– Green tea is more effective in reducing plaque than chlorhexidine. Green tea also had the highest effect on reducing gingivitis and gingival bleeding compared to chlorhexidine. Green tea also had the best effect on reducing clinical attachment level and probing pocket depth, which are indicators of periodontal disease severity.
– Emblica officinalis fruit extract (Amla) has the potential to prevent tooth decay by inhibiting the virulence factors of Streptococcus mutans.
– Amla reduced the adherence of Streptococcus mutans to the tooth by 50% at certain concentrations. Amla also reduced the biofilm formation by 50% at lower concentrations. Also, amla decreased the glucan synthesis and the stickiness of the bacterium.
– Oil of oregano besides its antioxidant properties and anti-cancer properties is one of nature’s most powerful antibiotics.
– Origanum oil and monolaurin (coconut oil) may be useful as natural alternatives or supplements to antibiotics for preventing and treating not just Staphylococcus infections but bacterial infections in general including in the mouth for dental health.
– The essential oil of oregano was able to stop the growth of all the Candida isolates ever tested. It could also kill most of them at a slightly higher concentration.
– Research has also shown that oregano oil may be effective against types of bacteria that can become resistant to antibiotics. It can also reduce the pain, inflammation, and irritation in your throat and improve your immune system. It is used for tooth pain and sensitive teeth.
– Clove essential oil is the most potent of essential oils in terms of raw ORAC value score.
– Clove essential oil is also a natural painkiller and this is a reason why it is used for toothache. The eugenol works like other local anesthetics, by temporarily blocking the nerves that carry the pain signal to the brain.
– Clove oil is one of the most potent essential oils for inhibition of the different fungi tested.
– Tea tree oil has been used for centuries as a natural remedy for various skin conditions, infections, and wounds. It has also been shown to have strong anti-inflammatory and antiseptic properties that can help with gingivitis.
– The tea tree oil mouth rinse showed a better improvement than the chlorhexidine mouth rinse in reducing plaque, bleeding, and pocket depth, which are all indicators of gingivitis.
– Methylene blue can kill bacteria, fungi, and parasites that are resistant to conventional drugs.
– Methylene blue targets three main aspects of Candida albicans: its mitochondria, its redox cycle, and its membrane.
– Methylene blue prevents Candida albicans from switching to hyphae, keeping it in the less dangerous yeast form.
– Most of the bacteria in the mouth and in the gut are unable to digest xylitol or erythritol. This blocks their energy production and kills them.
– Erythritol inhibits the growth of S. mutans more than the xylitol at the same concentration. Erythritol is also less toxic.
– Consuming artificial sweeteners is not healthy. Research has associated artificial sweeteners with a wide range of health conditions such as cancers and DNA damage, hepatotoxicity, migraines, and low birth weight.
– If you eat artificial sweeteners, they will alter the microbiome or in other words the bacteria that grow in your gut and in your mouth.
– Different studies have shown that rinsing your mouth with Aloe vera juice can reduce plaque as effectively as chlorhexidine. Moreover, aloe vera does not cause any side effects, unlike chlorhexidine.
– Make and use the homemade natural mouthwash after brushing at least two times a day instead of chlorhexidine. It is a very potent solution and less toxic and if swallowed might give you some nausea but also a high burst in ORAC value.
Chlorhexidine Mouthwash.
Have you ever wondered what that purple liquid your dentist gives you to rinse your mouth is? It’s called chlorhexidine, and it’s one of the weapons used against bacteria in your mouth.
Chlorhexidine is an antiseptic agent that can kill many kinds of germs and prevent them from growing back. It can help you keep your teeth and gums healthy by reducing plaque, inflammation, and bleeding (Varoni et al., 2012). It can also make your breath fresher and your smile brighter.
Chlorhexidine is not a substitute for brushing and flossing. It’s a supplement that can boost your oral hygiene, especially if you have trouble cleaning your teeth properly.
Chlorhexidine comes in different forms and strengths, depending on your needs and preferences. You can use it as a mouthwash, a gel, an aerosol, a spray, or a disk. You can find it over the counter or get it prescribed by your dentist.
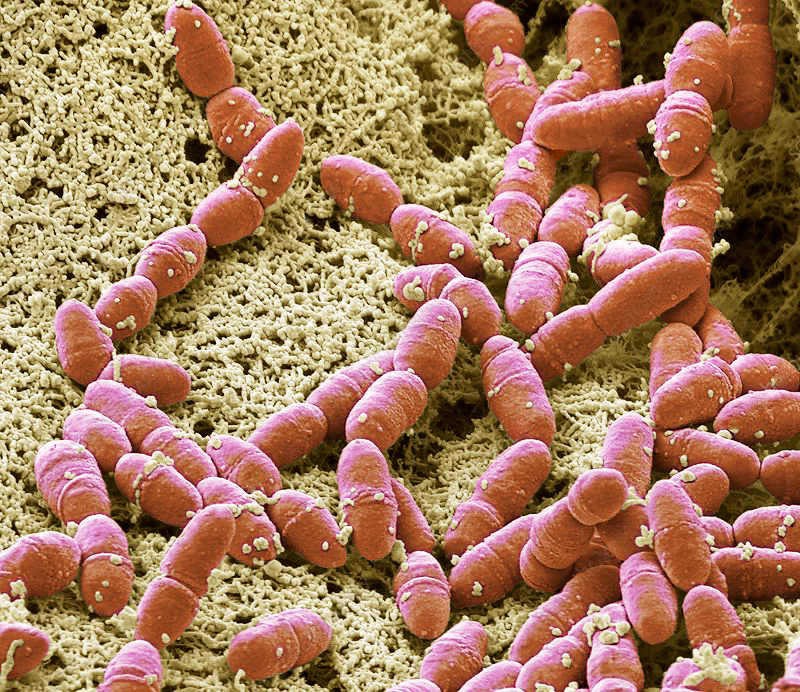
Chlorhexidine works by damaging the cell membranes of the germs, making them leaky and unstable.
This causes the vital fluids and components inside the cells to escape, leading to the death of the germs. Chlorhexidine is effective against both gram-positive and gram-negative bacteria, which are two major groups of bacteria that differ in their cell wall structure. Chlorhexidine can also kill fungi, which are organisms that cause infections such as thrush and candidiasis.
Many dentists recommend chlorhexidine as an adjunct to regular brushing and flossing, especially for patients who have gum disease, dental implants, braces, or other dental devices.
However, what if I told you that chlorhexidine could also harm your cells and damage your DNA? Would you still want to use it?
Some studies have suggested that chlorhexidine may have genotoxic effects, which means it can damage the DNA of cells and cause mutations or cancer.
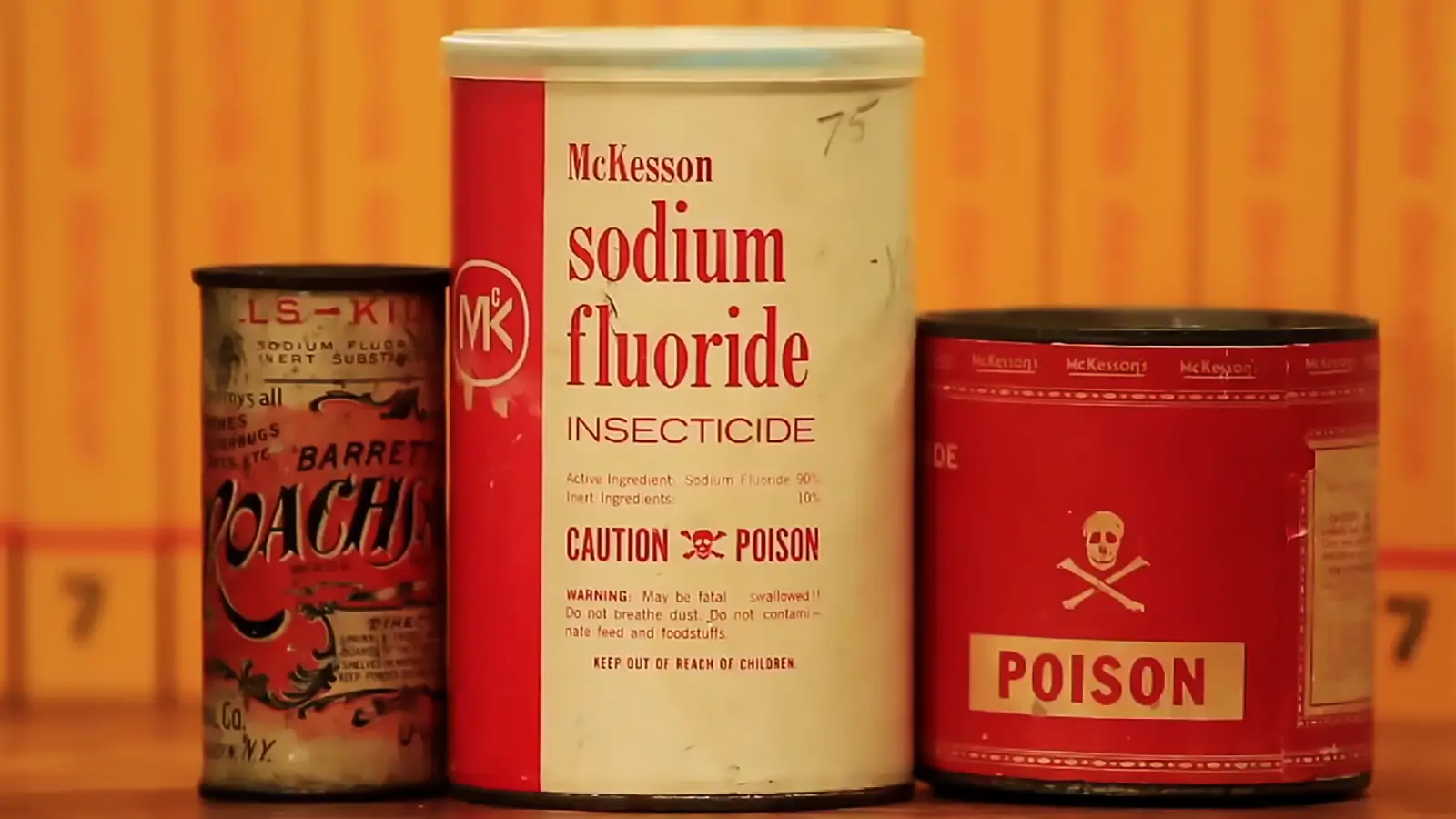
Chlorhexidine Toxicity.
How can chlorhexidine damage the DNA of cells? One possible mechanism is by generating reactive oxygen species (ROS), which are highly reactive molecules that can attack and oxidize other molecules. Chlorhexidine can increase ROS production by breaking down oxygen bonds with iron ions in a process called a Fenton-like reaction. This produces alkoxyl radicals, which are very harmful to cells. ROS can also react with unsaturated lipids on cell membranes and plasma lipoproteins, resulting in lipid peroxidation. This produces malondialdehyde (MDA), which is a toxic compound that can chemically alter proteins and nucleic acids.
The genotoxic effects of chlorhexidine have been tested in various ways, tests have shown that chlorhexidine can induce DNA damage in various organs and tissues, such as leukocytes (white blood cells), liver, kidney, and oral mucosa (the lining of the mouth) (Ribeiro, 2008).
However, the genotoxicity of chlorhexidine may depend on many factors, such as the dose, the duration, and the frequency of exposure, as well as the type of cells and tissues involved. What is the real-life exposure level of toxicity?
In this study (Grassi et al., 2007) researchers wanted to see if chlorhexidine digluconate could cause DNA damage in different types of cells in rats. They gave 10 male rats either water or chlorhexidine by mouth for 8 days, and then they collected samples of their blood, liver, kidney, and bladder cells.
They found that chlorhexidine caused significant DNA damage in the blood and kidney cells of the rats. This means that chlorhexidine could potentially affect the immune system and the kidney function of the rats. However, they did not find any DNA damage in the liver and bladder cells. This means that chlorhexidine may not affect these organs as much.
What does this mean for us humans? Well, it’s hard to say for sure. The study was done on rats, not humans, and the dose and duration of exposure may be different from what we use in dentistry.
However, this study does raise some concerns about the safety of chlorhexidine as a mouthwash. It suggests that chlorhexidine may not be as harmless as we think.
One study on humans in vivo compared different types of mouthwashes and their effects on cells (Carlin et al., 2011).
The study involved 75 volunteers who used one of five types of mouthwash: Listerine Cepacol, Plax alcohol-free, Periogard, and Plax Whitening. They used the mouthwash twice a day for two weeks and then gave samples of their cheek cells. The researchers also took blood samples from three healthy donors and exposed them to the same mouthwashes in the lab.
The results showed that Periogard and Plax Whitening caused more DNA damage and cell death than the other mouthwashes. Periogard increased the number of micronucleated cells by almost seven times, which means it caused a lot of chromosome damage. Plax Whitening had a high tail moment value, which means it caused a lot of strand breaks in the DNA. On the other hand, Listerine reduced the DNA damage caused by hydrogen peroxide, which is a strong oxidant that can harm cells. Listerine acted as an antioxidant agent that protected the cells from oxidative stress.
Liver and Energy Metabolism.
Chlorhexidine can also affect liver and energy metabolism.
A recent study (Pereira-Maróstica et al., 2023) was done on rat livers that were perfused, which means they were kept alive and functioning outside the body by pumping blood through them. The researchers added different concentrations of chlorhexidine to the blood and measured how it affected the liver’s metabolic pathways, which are the chemical reactions that produce and use energy in the cells.
They found that chlorhexidine had several negative effects on the liver’s metabolism. It inhibited both glucose synthesis and the urea cycle, which are two important processes that regulate blood sugar levels and nitrogen waste removal. It also altered the oxygen consumption of the liver cells, which is a measure of how much energy they use. At low concentrations, chlorhexidine increased oxygen consumption, which means it made the cells work harder and use more energy. At higher concentrations, chlorhexidine decreased oxygen consumption, which means it made the cells less efficient and less able to produce energy.
Chlorhexidine also reduces the cellular ATP content, which is the main source of energy for the cells. This means that chlorhexidine makes the cells weaker and less able to perform their functions. On the other hand, chlorhexidine stimulated glycolysis, which is the breakdown of glucose into lactic acid. This means that chlorhexidine makes the cells produce more acid, which can lower the pH of the blood and cause acidosis. Chlorhexidine also enhances the leakage of cellular enzymes, such as lactate dehydrogenase and fumarase, which are normally found inside the cells and help with metabolism. This means that chlorhexidine damages the cell membranes and causes cell death.
The researchers also tested how chlorhexidine affected isolated mitochondria, which are the parts of the cell that produce most of the ATP. They found that chlorhexidine inhibited pyruvate carboxylation, oxidases, and oxygen uptake, which are all essential steps in ATP production. They also found that chlorhexidine promoted uncoupling, which means it disrupted the balance between electron transport and ATP synthesis in the mitochondria. This means that chlorhexidine wastes energy and heat instead of making ATP.
The results of this study suggest that chlorhexidine is not as safe as we think and that it can have serious consequences for our liver and our energy metabolism.
It can cause hypoglycemia (low blood sugar), lactic acidosis (high blood acid), ammonia (high blood ammonia), as well as cell membrane disruption and cell death. These effects can impair our liver function and our overall health.
Therefore, we should be careful about how we use chlorhexidine.

Nitric Oxide.
You probably know that oral bacteria can cause bad breath, tooth decay, gum disease, and even heart problems. But did you know that they can also help lower your blood pressure? It may sound too good to be true, but there is a scientific explanation behind this.
It all has to do with nitric oxide, a molecule that relaxes and widens your blood vessels, making it easier for blood to flow. Nitric oxide is produced by your body from an amino acid called l-arginine. But there is another way to get nitric oxide: from the food you eat.
Some foods, like spinach and beetroot, are rich in nitrate, a chemical that can be converted to nitrite and then to nitric oxide. But this conversion does not happen in your stomach or intestines. It happens in your mouth, thanks to the bacteria that live there.
When you eat nitrate-rich foods, some of the nitrate is absorbed into your blood and then transported to your salivary glands. There, it is secreted into your saliva and mixed with the bacteria in your mouth. These bacteria have the ability to reduce nitrate to nitrite, which is then swallowed and absorbed into your blood. From there, it can be further reduced to nitric oxide in various tissues, especially under low oxygen conditions.
This process is called the enterosalivary circulation of nitrate, and it is a natural way to boost your nitric oxide levels and lower your blood pressure. But what happens if you disrupt the bacteria in your mouth? For example, by using an antiseptic mouthwash that kills them. Will this affect your blood pressure?
That’s what a group of researchers wanted to find out. They conducted a study with 19 healthy volunteers who used a chlorhexidine-based mouthwash for 7 days (Kapil et al., 2013). They measured their blood pressure, oral nitrite production, and plasma nitrite levels before and after the mouthwash treatment.
The mouthwash reduced the oral nitrite production by 90% and the plasma nitrite levels by 25%. This was associated with an increase in blood pressure by 2–3 .5 mm Hg. The effect was seen within one day of using the mouthwash and lasted for the entire 7-day period.
This study suggests that oral bacteria play an important role in regulating your blood pressure by producing nitrite from nitrate. By killing them with mouthwash, you may be interfering with this natural mechanism and increasing your risk of hypertension. So, before you reach for that bottle of mouthwash, think twice about how it may affect your heart health.
Highlights:
- Oral bacteria convert dietary nitrate to nitrite, which can be recycled to nitric oxide.
- This boosts the nitric oxide levels and lowers the blood pressure.
- Mouthwash kills the oral bacteria and reduces the nitrite and nitric oxide production.
- This increases the blood pressure by disrupting the enterosalivary circulation of nitrate.
- Oral bacteria are important for maintaining normal blood pressure and heart health.
- Mouthwash may have adverse effects by disturbing the nitric oxide/nitrite balance.
Green Tea.
Green tea is not only a delicious and refreshing beverage, but also a natural source of polyphenols, which are powerful antioxidants that can protect your body from various diseases.
But did you know that green tea can also benefit your oral health?
In this article, we will review the evidence from clinical trials that have tested the effects of green tea on periodontitis and caries, two common oral diseases that affect millions of people worldwide.
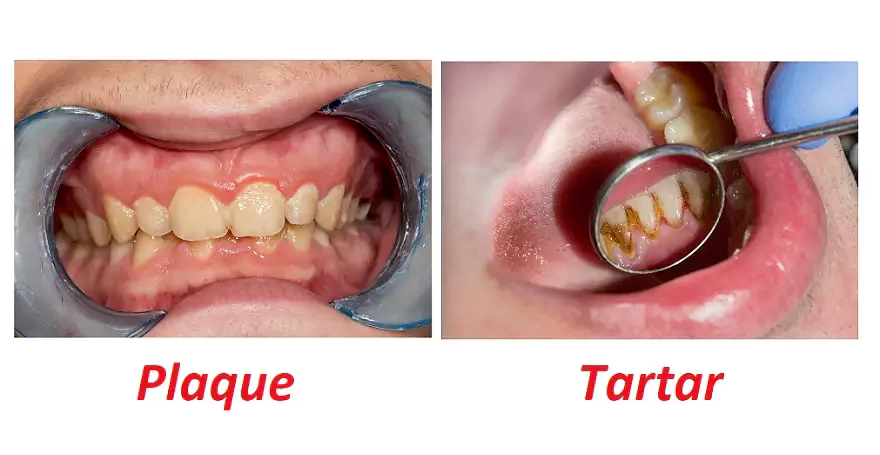
Periodontitis is a chronic inflammation of the gums and the supporting tissues of the teeth, which can lead to tooth loss and increased risk of systemic diseases such as diabetes and cardiovascular disease. Caries is a decay of the tooth enamel caused by bacteria that produce acids that dissolve the minerals in the teeth. Both periodontitis and caries are influenced by many factors, such as oral hygiene, diet, and lifestyle.
Green tea has been shown to have anti-inflammatory, antibacterial, and anticarcinogenic properties, which may help prevent or treat periodontitis and caries.
However, the quality and quantity of the evidence are still unclear. In a recent systematic review of the literature, researchers looked to find randomized clinical trials that compared the efficacy of green tea versus control groups in various aspects of oral health (Mazur et al., 2021).
Results showed that green tea treatment had a medium positive effect size in reducing plaque index, gingival index, gingival bleeding index, and bleeding on probing compared to the control group. However, when we split the studies into subgroups according to the type of control group (water, placebo, or chlorhexidine), they found that green tea had a small negative effect in the chlorhexidine group.
This means that chlorhexidine, which is a common antiseptic mouthwash, was more effective than green tea in improving oral hygiene and gingival health. However, this was a small difference, and green tea unlike chlorhexidine is not toxic, and the concentration of the tea extract used in studies is generally medium to low.
Green tea treatment also had a medium positive effect size in reducing clinical attachment level and a large positive effect size in reducing probing pocket depth compared to the control group.
These findings indicate that green tea can help reduce the severity of periodontitis by preventing or reversing the loss of attachment and the formation of deep pockets around the teeth.
Green tea treatment did not have a significant effect on caries compared to the control group. This may be due to the short duration or low frequency of green tea intake in some studies, or to confounding factors such as fluoride exposure or dietary habits.
Green tea treatment had a small positive effect size in reducing periodontal pathogens number compared to the control group. However, this effect was not consistent across different types of pathogens. That is a reason why we need to combine green tea with other antimicrobial natural substances.
Green tea treatment had a large positive effect size in reducing Streptococcus mutans, which is a major cause of caries, but no significant effect on Lactobacillus spp., which is another cariogenic bacterium.
In conclusion, this systematic review suggests that green tea may have some beneficial effects on oral health, especially on periodontitis.
However, scientists in this review still believe that there is insufficient evidence to recommend the use of green tea formulation as the first choice treatment for gingivitis, periodontitis, and caries. This is because it lacks the complete antimicrobial properties and its effect was not consistent across different types of pathogens.
I would disagree, and by the end of this article, we will use green tea as a base for our solution, plus a range of other proven natural substances to create our own mouthwash that would be extremely more powerful than commercial chlorhexidine products and less genotoxic.
The benefit of green tea is that it is a natural product and we don’t need to use a weak solution. We can increase the concentration of tea extract in a solution much higher than the levels used in studies. For example in this study (Balappanavar et al., 2013), scientists compared the effectiveness of green tea, neem, and chlorhexidine mouthwashes on oral health.
They conducted a randomized blinded controlled trial with 30 healthy human volunteers of age group 18-25 years to evaluate and compare the effectiveness of 0.5% tea, 2% neem, and 0.2% chlorhexidine mouthwashes on oral health.
The subjects were instructed to rinse their mouths with 10 ml of their assigned mouthwash twice a day for three weeks. They skipped the third week for group A because chlorhexidine is not recommended for long-term use because of genotoxicity.
Results showed that all three mouthwashes reduced plaque and gingival scores over the three-week trial period.
Tea was the most effective in reducing plaque, followed by neem and chlorhexidine.
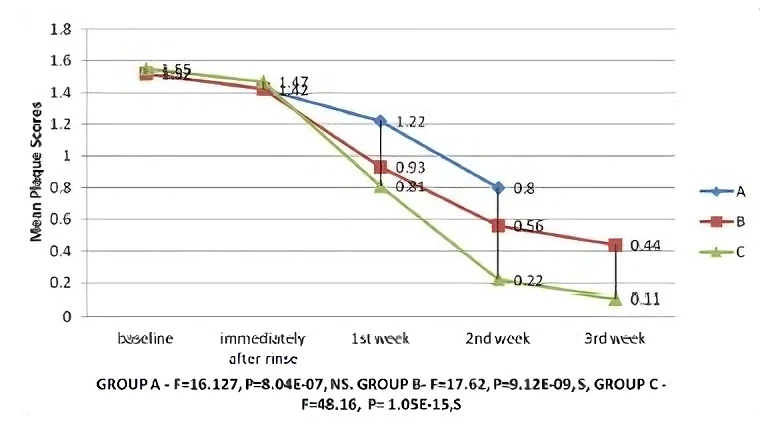
Tea also had the highest effect on reducing gingivitis and gingival bleeding compared to neem and chlorhexidine.
Tea also had the best effect on reducing clinical attachment level and probing pocket depth, which are indicators of periodontal disease severity. Neem was second best, while chlorhexidine had no significant effect.
They did not find any significant difference among the three mouthwashes in reducing caries. This may be because caries is influenced by many other factors besides oral hygiene, such as diet or in other words the amount of free sugar in the diet someone will consume.
However, the study did find that tea and neem increased salivary pH more than chlorhexidine.
Salivary pH is a measure of acidity or alkalinity in the mouth. A higher pH means a more alkaline environment that inhibits bacterial growth and acid production which causes tooth decay.
The study also found that tea and neem reduced periodontal pathogens number more than chlorhexidine. Periodontal pathogens are bacteria that cause gum disease by invading the tissues around the teeth.
Tea has a large effect on reducing Streptococcus mutans, which is a major cause of caries.
Neem had a moderate effect on reducing Streptococcus mutans as well as Lactobacillus spp., which is another cariogenic bacterium.
Finally, the study found that tea and neem improved oral hygiene index simplified (OHI-S) more than chlorhexidine. OHI-S is a measure of oral cleanliness and debris accumulation on the teeth. Tea and neem reduced the amount of debris and improved the appearance of the teeth.
In conclusion, this study suggests that tea and neem are natural and effective mouthwashes that can improve oral health by reducing plaque, gingivitis, periodontal disease, and bacterial load. They also have advantages over chlorhexidine, such as increasing salivary pH, improving oral hygiene, and having fewer side effects. Therefore, the study recommends the use of 0.5% tea or 2% neem mouthwash as an alternative or adjunct to chlorhexidine mouthwash for oral health maintenance.
Keep in mind that 0.5% tea solution is just the potency of regular tea we would drink. This is not a high-level tea extract concentration someone would expect to be used as an antiseptic. It is just regular tea they use for testing and 0.2% chlorhexidine is the standard mouthwash solution you will find in the store.
If we look into commercial green tea mouthwashes for example if we look into ingredient lists for the Listerine Green Tea Zero, we would find that it has less than 1% of Camellia Sinensis Leaf Extract (Green Tea). If you look into the image below you will see it has a translucent almost yellow color.
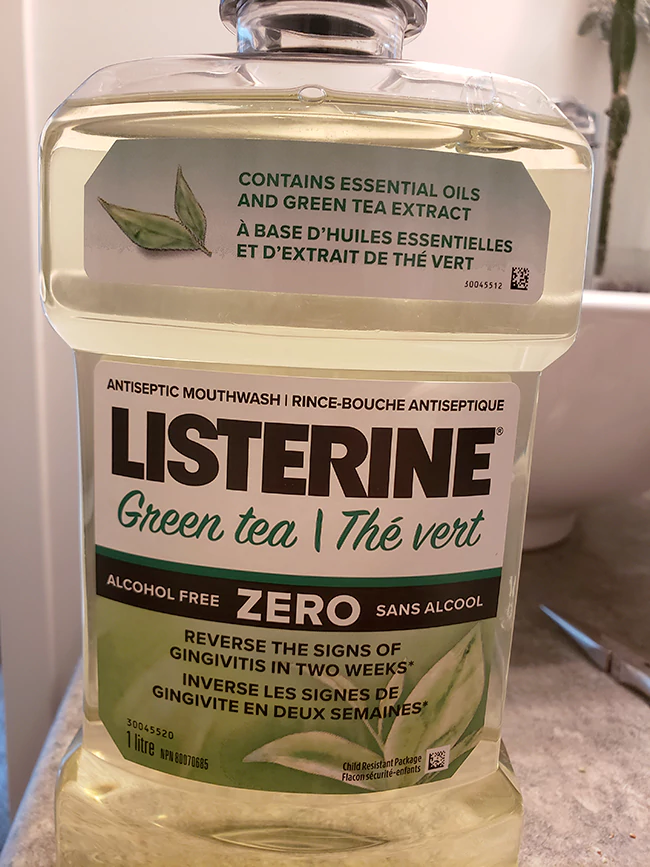
It also has fluoride, and two synthetically manufactured phytochemicals Thymol (Oil of oregano) and Eucalyptol.
Natural herbal tea and essential oils have hundreds of different phytochemicals that are present in the plants that work in synergistic ways and single monotherapy is always less effective than when we use whole plants as a source. However, essential oils are much more expensive to produce.
Also, I do not understand the reason why would Johnson & Johnson use such a low-potency product. Green tea is not that expensive. Probably they use what is found to be at the same level of effectiveness as a regular chlorhexidine mouthwash to save on the cost. Johnson & Johnson is the same company that knew about the cancer risk of their talcum powder but still decided to misinform and represent talcum powder as an absolutely safe product and was sanctioned to pay 550 million dollars in damages to 22 women.
You don’t have to do this at home. You can make it as potent as you want. You can aim at much higher tea concentrations and darker colors. You don’t have to use matcha for the mouthwash or branded tea bags. Green tea is cheap if you go to the health food store and buy it in bulk.

Amla.
Streptococcus mutans love to feed on the sugar you eat. As it does so, it produces acid that erodes your tooth enamel and causes cavities. But that’s not all. It also makes sticky substances called glucans from the sugars it consumes and forms a sticky layer of slime called biofilm on the teeth. Biofilm or plague protects it from the saliva and immune system.
This bacteria can also enter the bloodstream and cause inflammation in the heart valves, leading to a condition called endocarditis.
One possible solution to deal with this bacteria is to inhibit its ability to make glucans, which are essential for its survival and biofilm formation. This is what many researchers have tried to do by testing different agents that can block the enzymes that make glucans. These enzymes are called glucosyltransferases.
One of the agents that has shown promising results in inhibiting glucosyltransferases is a plant extract from Phyllanthus emblica, also known as amla.
Amla is a sour fruit that grows in India and other parts of Asia, and it has been used for centuries in Ayurvedic medicine for various health benefits. It is rich in antioxidants, vitamin C, and other phytochemicals that have anti-inflammatory, anti-microbial, and anti-cancer properties.
Amla is that it is one of the world’s most powerful antioxidants with an ORAC score of 261,530 and it is as potent as cloves.
But how does amla work against Streptococcus mutans and its biofilm formation? That is what the scientists in this study decided to investigate (Hasan et al., 2012). They extracted the active compounds from the amla fruit using water and alcohol and tested their effects on different aspects of the bacterium’s life cycle.
They found that both the water and alcohol extracts of amla reduced the adherence of Streptococcus mutans to the tooth by 50% at certain concentrations. They also reduced the biofilm formation by 50% at lower concentrations. Also, they decreased the glucan synthesis and the stickiness of the bacterium.
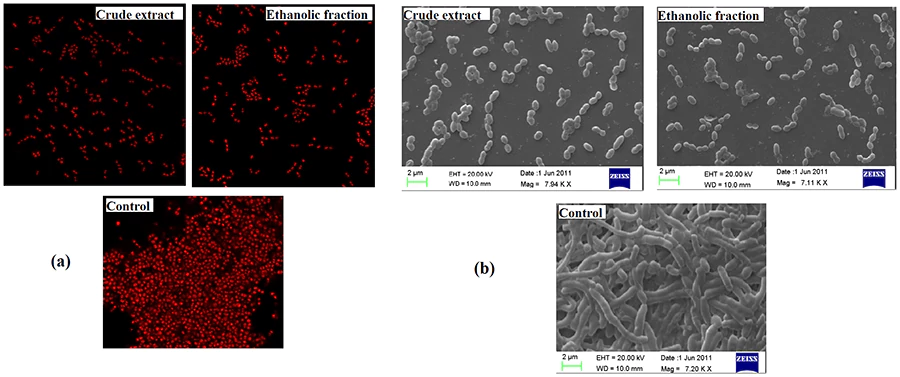
The gene expression analysis showed that the extracts suppressed the genes that are important for biofilm formation. The microscopic images confirmed that the extracts disrupted the biofilm structure compared to the control. Therefore, they concluded that Emblica officinalis fruit extracts (Amla) have the potential to prevent tooth decay by inhibiting the virulence factors of Streptococcus mutans.
So, what does this mean for you? It means that you might want to add some amla to your diet or oral hygiene routine. Amla is available in various forms, such as fresh fruit, dried powder, juice, or capsules. You can also find toothpaste or mouthwashes that contain amla extract as an ingredient. However, before you do so, make sure to consult your dentist or doctor first, as amla might interact with some medications or have some side effects.
You can read more about Amla in this article Amla: Proven Benefits, Nutrition And Clinical Significance.
Oil of Oregano.
Oil of oregano besides its antioxidant properties and anti-cancer properties is one of nature’s most powerful antibiotics.
It contains carvacrol and thymol, two antibacterial and antifungal compounds.
In fact, research shows oregano oil is effective against many clinical strains of bacteria, including Escherichia coli and Pseudomonas aeruginosa both of which are common causes of urinary tract and respiratory tract infections.
In studies, it was shown to be as effective as antibiotics (Preuss et al., 2005).
Another example would be lauric acid, which is found in large amounts in coconuts and can turn into monolaurin in the body. Lauric acid is found in breast milk and it has antimicrobial properties for the baby. Monolaurin has a similar effect as Origanum oil and can inhibit the growth of pathogenic microbes. Oil pulling with coconut oil is one more tactic people use traditionally for inflamed gums and oral health.
Coconut oil as a mouthwash can be used but it would be harder to make a mixture with green tea and amla because in its natural state coconut oil is solid and solid oil and water don’t mix well.
It could be warmed up and mixed with other essential oils for oil pulling. It could be used as a standalone product.
Monolaurin is available as a supplement in capsules and poetically it could be added or dissolved into the mouthwash recipe but the problem is that it is practically insoluble in water. I personally never used it and I don’t know how would it work if added to the mouthwash or in the mouth directly.
Staphylococcus aureus is a common cause of skin infections, food poisoning, and even life-threatening diseases. In the study (Preuss et al., 2005), the researchers compared the effectiveness of Origanum oil, carvacrol, other essential oils, and monolaurin against two strains of Staphylococcus aureus in the laboratory. They found that Origanum oil was the most potent of the essential oils tested and could kill both strains of bacteria at a very low concentration (0.25 mg/mL). Monolaurin had a similar potency as Origanum oil. When they combined both substances, they could kill the bacteria at an even lower concentration (0.125 mg/mL each).
The researchers also tested these substances in mice that were infected with Staphylococcus aureus. They gave the mice either Origanum oil, monolaurin, vancomycin (a common antibiotic), or a combination of Origanum oil and monolaurin by mouth every day for 30 days.
They found that all the untreated mice died within a week. The mice that received Origanum oil alone had a survival rate of about 43% (6 out of 14). The mice that received vancomycin or monolaurin alone had a survival rate of about 50% (7 out of 14 and 4 out of 8, respectively). The mice that received both Origanum oil and monolaurin had the highest survival rate of about 63% (5 out of 8).
These results suggest that Origanum oil and monolaurin may be useful as natural alternatives or supplements to antibiotics for preventing and treating not just Staphylococcus aureus infections but bacterial infections in general including in the mouth for dental health.
Besides bacteria, Origanum oil also kills fungi and viruses. A test-tube study of the effectiveness of oregano oil on 16 different strains of Candida, both standard strains and some from dogs and a monkey, concluded that oregano oil may be a good alternative treatment for Candida yeast infections (Cleff et all., 2010).
The essential oil of oregano was able to stop the growth of all the Candida isolates tested.
It could also kill most of them at a slightly higher concentration. The researchers analyzed the composition of the essential oil and found that it contained mainly 4-terpineol (47.95%), carvacrol (9.42%), thymol (8.42%) and terpineol (7.57%). These compounds are known to have antifungal effects.
The researchers concluded that the essential oil of oregano may be a useful natural alternative or supplement to antifungal drugs for treating candidiasis, which is an infection caused by Candida. Candida lives in symbiosis with Streptococcus mutans in the mouth. If we want to stop biofilm from forming and prevent tooth decay we have to realize that we fight both fungi and bacteria and their symbiotic relationship.
Research has also shown that oregano oil may be effective against types of bacteria that can become resistant to antibiotics. It is very potent.
Because of its potency, it can be used as an addition to homemade natural mouthwash for more than dental care. Traditionally oregano oil is used for sore throat, and for strep throat as a gargle. If it is ingested it would exert a powerful antifungal, antibacterial, anti-inflammatory, and antioxidant effect systemically however as a mouthwash it would also exert all of its effects topically. It is a superior product to commonly prescribed antibiotics because it has also antifungal effects and anti-inflammatory effects as a strong antioxidant.
It can also reduce the pain, inflammation, and irritation in your throat and improve your immune system. It is used for tooth pain and sensitive teeth.
However, it can cause some side effects, especially in higher concentrations, such as irritation, burning, nausea, vomiting, or allergic reactions. When using it we should find the most effective and powerful dosage to have maximum benefits without causing ourselves a chemical burn. If you use oil of oregano for oral ingestion you should also be careful as it can have side effects or interactions with some medications. It can interact with blood thinners, antidiabetic drugs, or antihistamines. You should also avoid using oregano oil if you are pregnant or breastfeeding.
The only question still unanswered in the research is whether the oregano oil kills all types of bacteria or is selective. Antibiotics will kill everything and will wreak havoc in our gastrointestinal tract killing both good and bad bacteria but the oil of oregano might not be as bad. There are some indications that it would not be as toxic to probiotic bacteria as regular antibiotics and if this is correct it would make oil of oregano a superior product to regular antibiotics. More research needs to be done in this field.

Clove Essential Oil.
Traditionally cloves have been used to fight inflamed gums both as an antibiotic and as a pain reliever for toothache. Today we can look at cloves and clove oil as one of the most potent sources of antioxidants.
Clove essential oil is so potent because the cloves themselves are one of the most potent antioxidant herbs with an ORAC value of 290,283. It should not come as a surprise that oil extract will be four times as powerful.
Even among essential oils, it is a superstar. Second on the essential oil list on the ORAC potency is myrrh essential oil with a 65% lower value.
Clove essential oil is the most potent of essential oils in terms of raw ORAC value score. Clove oil has an ORAC value of 1,078,700.
At the same time the most popular of them all. It is so popular that we can find this oil almost at every health food store or pharmacy. People like this oil not because it is one of the most antioxidant-rich substances in existence but because it has a very nice aroma. It is sweet as vanilla and spicy as pepper at the same time. It has the best scent according to most consumers.
We can use Clove essential oil for our recipes or medicine however, it is extremely concentrated and should never be taken in undiluted form. If it touches the skin it can cause irritation. If you try to consume this oil it will cause damage to gums and dental tissue and will burn your mouth and throat. When it reaches the stomach, it can cause abdominal pain, diarrhea, and vomiting.
Also, it has very potent anticoagulant/antiplatelet activity in the bloodstream and can cause increased bleeding due to less blood clotting. If you have heart disease you can add this oil as a substitute for warfarin.
It is also a natural painkiller and this is a reason why it is used for toothache. One of the myths you will hear is that clove oil kills nerves. That’s not how its numbing mechanism works. Before a Lidocaine or Novocain injection, dentists use to swab your gums with clove oil for 5 minutes for some preliminary anesthetic action (today they use more effective chemicals).
The eugenol works like other local anesthetics, by temporarily blocking the nerves that carry the pain signal to your brain. There is no “killing” of the nerves involved, as some people believe. Clove oil for toothache is as powerful a remedy as any other prescribed medicine.
However, if we do not have active pain and don’t need to use clove oil for toothache, why would we want to include it in a natural mouthwash recipe? And the answer is because of its antioxidant properties. Antioxidants just by themselves are able to fight and lower inflammation in the gums and also to kill bacteria and fungi.
Today there are a number of studies that have found a range of different benefits of cloves both in terms of ground cloves and as oil. They work and are the same in a sense.
In this study (Chamdit & Siripermpool, 2012) researchers have found that clove oil had the ability to kill staph bacteria cells in liquid culture and in biofilm. Most antibiotics aren’t effective at penetrating the biofilm and killing staph bacteria but according to this study, clove oil seems to be able to.
I’m talking about Staphylococcus aureus, or staph for short, which can cause infections in your skin, lungs, blood, or bones. Staph can be very hard to treat, especially when it forms a biofilm.
The researchers found that clove oil was more potent than lemongrass oil against staph in liquid form. It could stop the growth of all the bacteria at a concentration of 2.0% to 3.0%, and kill most of them at a concentration of 2.4% to 5.0%. Lemongrass oil was less effective, but still had some activity against some of the bacteria. However, when the bacteria formed a biofilm, both oils became less potent. They needed higher concentrations to inhibit or kill the bacteria in biofilm form. The researchers also found that combining clove oil and lemongrass oil had a synergistic effect against staph. This means that they worked better together than alone. They could kill staph faster and more efficiently when used together.
These results suggest that clove oil and lemongrass oil may be useful as natural alternatives or supplements to antibiotics for treating staph infections. Or even better use a clove essential oil with other strong antimicrobial essential oils like oregano oil. They may be able to penetrate and destroy the biofilm that makes bacteria resistant to most drugs, especially in the plague formed in the mouth.
We could also add lemongrass oil to the mouthwash because of its lemon-refreshing taste and smell, and we could also add mint. This is not necessary and would only be done for taste preferences.
What about fighting candida? A 2017 study (Schroder et al., 2017) looked at the antifungal activity of several essential oils against a range of fungal species isolated from environmental air samples. The researchers tested three essential oils that are known for their antifungal capabilities: clove, lavender, and eucalyptus. They wanted to see how effective they were against different types of fungi that were isolated from environmental air samples.
They placed small disks soaked with the oils on a special agar plate that supported fungal growth. They then observed how the oils affected the growth of the fungi around the disks. They compared the results with some common household cleaning agents, such as vinegar, bleach, and limonene, as well as a chemical antifungal agent, phenol.
The researchers found that clove oil was the most potent of the essential oils tested. It could inhibit or kill almost all the fungi tested, even after 14 days of incubation. Eucalyptus and lavender oils also showed some antifungal potential, but they were less effective and less persistent than clove oil.
All the essential oils performed better than vinegar, which had little or no antifungal activity. Bleach and limonene had some antifungal activity, but they were less potent and less persistent than the essential oils. Phenol was the most potent and persistent antifungal agent, but it was also very toxic and not suitable for indoor use nonetheless for consumption.
Tea Tree Oil.
Gingivitis is a very common problem that can affect anyone, regardless of age or oral hygiene habits. It can cause symptoms like redness, swelling, bleeding, and bad breath. It can also lead to more serious complications like periodontitis and tooth loss if left untreated.
That’s why it is crucial to take good care of your oral health and use products that can prevent and treat gingivitis effectively. One of the most widely used products for this purpose is chlorhexidine mouth rinse. It has been proven to be very effective in reducing gingivitis when used as an adjunct to mechanical oral hygiene procedures, such as brushing and flossing.
If you are looking for a natural and safe alternative to chlorhexidine, you may want to consider tea tree oil. Tea tree oil is an essential oil extracted from the leaves of the Melaleuca alternifolia tree, a plant native to Australia.
Tea tree oil has been used for centuries as a natural remedy for various skin conditions, infections, and wounds. It has also been shown to have strong anti-inflammatory and antiseptic properties that can help with gingivitis.
Tea tree oil contains two main components that give it its therapeutic benefits: terpineol-4 and 1,8-cineol. Terpineol-4 is responsible for the antimicrobial activity of tea tree oil, while 1,8-cineol is responsible for its anti-inflammatory activity.
Tea tree oil has a broad spectrum of action against many microorganisms, including those that cause gingivitis. It can kill bacteria like Streptococcus mutans, Porphyromonas gingivalis, Fusobacterium nucleatum, and Prevotella intermedia. It can also inhibit the growth of Candida albicans, a fungus that can cause oral thrush.
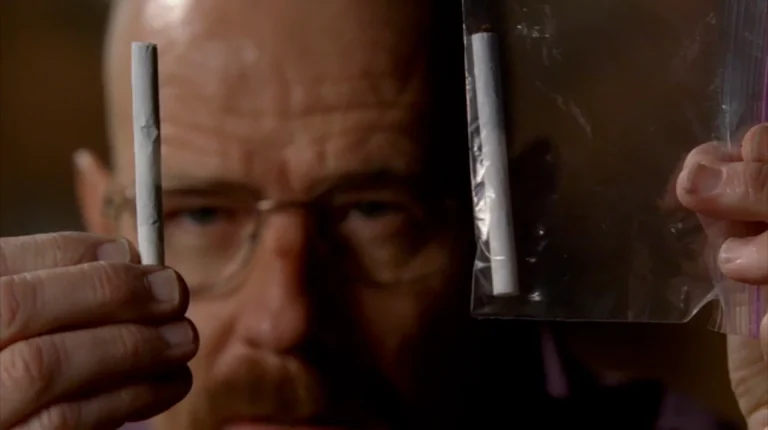
A recent study (Ripari et al., 2020) compared the efficacy of tea tree oil mouth rinse with chlorhexidine mouth rinse in treating gingivitis. The researchers compared two types of mouthwash: one containing tea tree oil and one containing chlorhexidine 0.12%. The researchers randomly selected patients who had clinically evident gingivitis and asked them to use one of the mouth rinses at home for 14 days. They also measured several clinical parameters before and after the treatment to evaluate the improvement.
The researchers randomly assigned the patients to one of the two groups.
In group A, the patients received a bottle with 10 mL of pure tea tree oil for oral use and a plastic dropper. They were asked to add three drops of tea tree oil to less than half a glass of water and rinse their mouth with it after brushing their teeth three times a day. This way, they would consume a total of nine drops of tea tree oil per day. Some patients, who had busy schedules, preferred to take four drops in the morning after breakfast and three drops in the evening after brushing their teeth. The important thing was to use the same amount of tea tree oil every day for 14 days.
In group B, the patients received 14 packages with 10 mL of chlorhexidine 0.12% each. Each package contained enough mouthwash for two rinses per day. They were asked to rinse their mouth with half a package (5 mL) in the morning and half a package (5 mL) in the evening after brushing their teeth. This way, they would use one package of chlorhexidine per day for 14 days. The rinsing had to last 60 seconds for both mouthwashes.
Both groups had to avoid eating and drinking for at least 30 minutes after using the mouthwashes. They also had to follow their usual oral hygiene habits, such as brushing and flossing.
The tea tree oil mouth rinse showed a better improvement than the chlorhexidine mouth rinse in reducing plaque, bleeding, and pocket depth, which are all indicators of gingivitis.
However, in my view, this solution is pretty weak. Three drops of tea tree oil to less than half a glass of water is the potency I use for consumption as an antioxidant supplement. You can read more about the benefits of essential oil for consumption in this article Essential Oils as Antioxidant Supplements: Rules and Strategies.
If we are making solutions for gingivitis and tooth decay prevention we don’t need to be concerned about nausea and other side effects except for direct chemical burn of the gums. Mouthwash would be spitted out and in my view, we should use the most potent and stronger solution that we can that would not cause us chemical burn. Three drops in half of a glass are not as potent as I would like personally. It is the potency of regular tea brew, not antiseptic salutation for gingivitis prevention.
Moreover, the tea tree oil mouthwash did not cause any dental dyschromia or taste alteration, unlike the chlorhexidine mouthwash so we can use higher concentrations. Some of the patients who used chlorhexidine complained about a bad taste in their mouth and noticed some yellowish stains on their teeth.
The study concluded that tea tree oil could be an effective nontoxic substitute for chlorhexidine in treating gingivitis. Although more research is needed to confirm these findings, this study suggests that tea tree oil has great potential as a natural and safe product for oral health.
If you are looking for a way to treat your gingivitis without using harsh chemicals or spending a lot of money, you may want to give tea tree oil a try. You can find tea tree oil mouth rinse in many health stores or online. You can also make your own by adding a few drops of tea tree oil to water.
Methylene Blue.
Methylene blue is a blue dye that has been used for over a century for various purposes, such as staining cells, treating malaria, and improving memory.
It is a powerful synthetic antioxidant. It improves mitochondrial function and the ability of our cells to produce energy.
Methylene blue can also fight against some of the most stubborn and dangerous infections.
Methylene blue can kill bacteria, fungi, and parasites that are resistant to conventional drugs.
Methylene blue is a powerful weapon against antibiotic-resistant Lyme disease. Lyme disease is caused by a type of bacteria called Borrelia burgdorferi, which is transmitted by ticks. Unfortunately, some strains of Borrelia burgdorferi have become resistant to the standard antibiotics used to treat Lyme disease, making it harder to cure. However, MB can overcome this resistance and kill Borrelia burgdorferi in the lab (Feng et al., 2015).
Methylene blue can also enhance the effectiveness of antibiotics against Bartonella infections.
Bartonella is another type of bacteria that can cause diseases such as cat scratch fever, trench fever, and endocarditis. They are also transmitted by ticks, fleas, and other animals. Some Bartonella infections can be treated with antibiotics, but others are more difficult to eradicate. However, studies have shown that combining MB with antibiotics is more effective than antibiotics alone to treat some types of Bartonella infections (Zheng et al., 2020).
Methylene blue is not only effective against bacteria but also against parasites that cause malaria. There are many drugs available to treat malaria, but some strains of Plasmodium have developed resistance to them, making them less effective. However, methylene blue can kill Plasmodium falciparum in laboratory tests, in mice, and monkeys. It can also overcome the resistance that some strains of P. falciparum and P. vivax have developed to other antimalarials (Gut et al., 2017).
Methylene blue can also act as an antifungal agent by causing oxidative stress in fungal cells.
This could be a useful way to treat Candida albicans infections and avoid drug resistance, which is a major problem in fungal therapy. Many antifungal drugs are available to treat Candida albicans infections, but some strains of Candida albicans have become resistant to them, making them harder to treat.
Methylene blue targets three main aspects of Candida albicans: its mitochondria, its redox cycle, and its membrane.
Mitochondria are the parts of the cell that produce energy, and the redox cycle is the process of transferring electrons between molecules. Methylene blue disrupts both of these processes, causing the fungal cells to lose energy and balance. Methylene blue also damages the membrane. It makes the membrane leaky and weak, making it easier for other drugs or the immune system to attack the fungal cells.
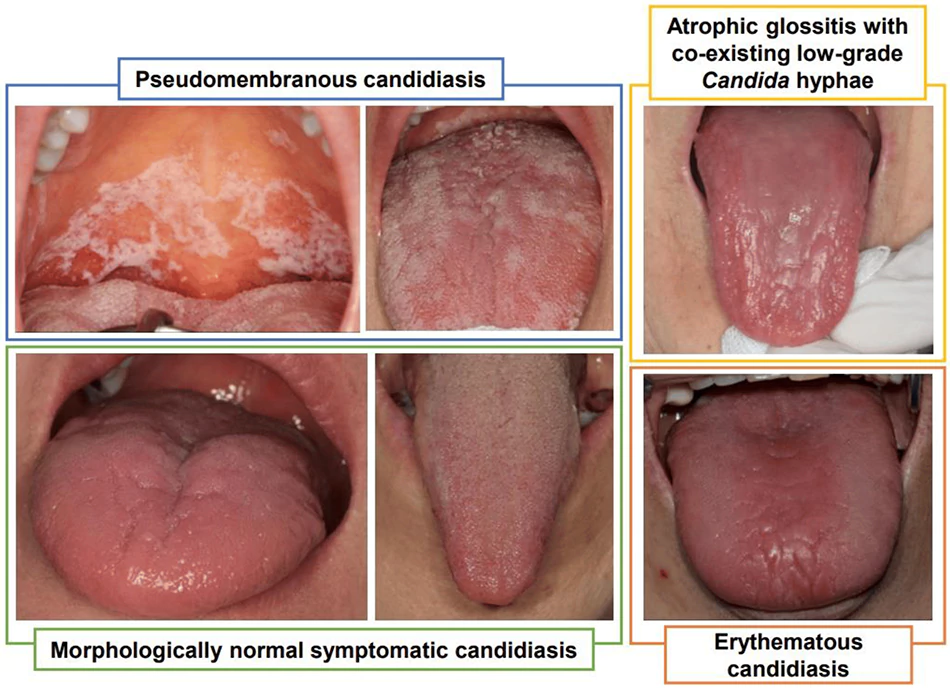
Another important feature of Candida albicans is its ability to change shape from yeast to hyphae. Yeast are round and single cells, while hyphae are long and branching structures. Hyphae help Candida albicans invade tissues and escape the immune system, making it more virulent or harmful.
Methylene blue prevents Candida albicans from switching to hyphae, keeping it in the less dangerous yeast form.
In this study (Ansari et al., 2016), they tested methylene blue ability to kill fungal cells by damaging their mitochondria and membranes. They found that methylene blue worked well against C. albicans and two other types of Candida that can also cause infections.
They also found that methylene blue was not affected by the drug pumps that Candida uses to get rid of antifungal drugs.
They showed that Candida cells treated with methylene blue could not grow well on a sugar-free source, which means that their mitochondria were impaired. They also showed that Candida cells treated with methylene blue became more sensitive to a detergent called SDS (sodium dodecyl sulfate), which breaks down their membranes. They also measured the amount of ergosterol, a type of fat that is important for the membranes of fungal cells. They found that methylene blue reduced the ergosterol level by 66%, which means that it changed the composition of the membranes. Moreover, the study showed that methylene blue prevented Candida from changing its shape from yeast to hyphae. This is a key feature of Candida’s virulence, or ability to cause disease.
This study shows that methylene blue is a promising antifungal agent that can target different aspects of Candida’s growth and survival.
However, if we use it as a natural mouthwash or as a gargle it has the potential to stain our teeth and mouth. This is the main reason why if you want to include it in a natural mouthwash recipe, I would not go any further than using just one drop. I found out that one drop would slightly color the solution and for me, it did not stain my teeth or mouth.
The way I use methylene blue is exactly the opposite. I use it to directly stain my tongue as a topical remedy for oral thrush. If I see a candida or oral thrush developing I would use methylene blue after the natural mouthwash. If I start to have candida on my tongue I would use methylene blue directly to the tongue and I would leave it there. I would avoid contact with my teeth by swallowing. This would stain my tongue without making contact with my mouth or teeth. I found out it is potent enough to help keep candida on the tongue from developing. This could be a potential addition for tongue scraping.
If you want to read more about Methylene blue you can read it in this article Methylene Blue: Therapeutic Uses and Clinical Significance.

Erythritol vs. Xylitol Mouthwash.
Xylitol and Erythritol are artificial sweeteners that have some benefits for teeth and gums.
Most of the bacteria in the mouth and in the gut are unable to digest xylitol or erythritol. Some can but most cannot.
When these bacteria eat erythritol or xylitol, they cannot get digested so they are stuck with it. Bacteria cannot get rid of it so they are stuck with it and can’t absorb regular glucose anymore. This blocks their energy production and kills them.
When you chew gum with xylitol or use it as a sweetener, you are not only reducing the food supply for the harmful bacteria by depriving them of free sugar but also wiping them out physically.
One study found that chewing gum with xylitol reduced the levels of bad bacteria in the mouth by around 25% (Bahador et al., 2012).
The study involved 24 volunteers. The volunteers chewed gum with either xylitol or sorbitol for three weeks, twice a day, after meals. Sorbitol is another natural sweetener, but it doesn’t have the same anti-bacterial effect as xylitol.
The xylitol gum reduced the number of S. mutans and S. sobrinus significantly. Percent reduction of logarithmic values amongst S. mutans and S. sobrinus by xylitol were 27% and 21%.
However, the xylitol gum did not reduce the number of S. sanguinis and S. mitis. This means that xylitol did not affect the beneficial bacteria that protect your mouth.
The conclusion of this study is that xylitol can help you prevent tooth decay by reducing the harmful bacteria in your mouth, without harming the beneficial bacteria.
In this systematic review (Söderling & Pienihäkkinen, 2021) the researchers found 424 articles about xylitol, but only 14 of them met their criteria for quality and relevance.
The results were clear. In 13 out of 14 studies, xylitol gum reduced plaque accumulation. In six studies, xylitol gum also reduced plaque more than sorbitol gum. This suggests that xylitol has a specific effect on plaque accumulation, not just a mechanical effect of chewing.
However, what about erythritol?
To find out more about erythritol’s effect, we can look into this study with teenagers (De Cock et al., 2016). They gave them chewable tablets with xylitol, erythritol, sorbitol, or nothing for six months. They measured the plaque weight and the S. mutans levels in the plaque and saliva before and after the study. The study found that both xylitol and erythritol reduced the plaque weight and the S. mutans levels significantly. In fact, erythritol was even better than xylitol at reducing plaque weight after six months.
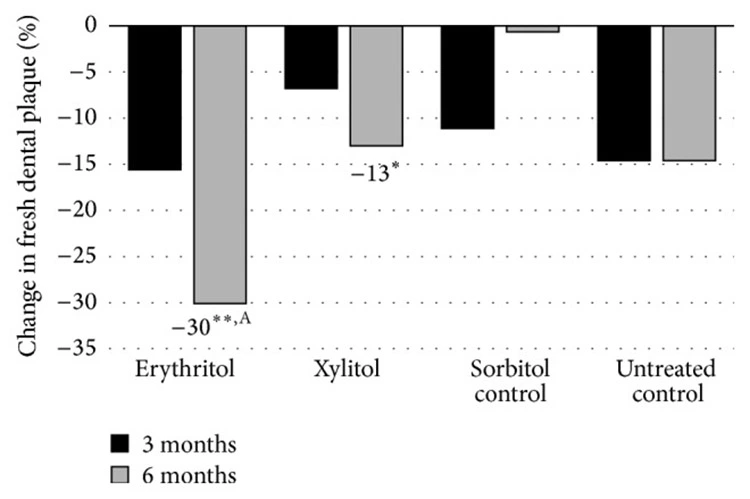
To explain why erythritol was so effective, they did some experiments in the lab with different strains of S. mutans. They exposed them to different concentrations of erythritol, sorbitol, xylitol, or maltitol for up to five hours and measured how much the bacteria grew.
They found that erythritol inhibited the growth of S. mutans more than the other sugar alcohols at the same concentration. This means that erythritol has a special property that makes it harder for S. mutans to survive.
This larger study (Honkala et al., 2014) involved 485 children from Estonia who were in the first or second grade at the start of the experiment for three years. The researchers gave them four candies to eat three times a day at school. The candies contained either erythritol, xylitol, or sorbitol (as a control).
They found that the children who ate erythritol candy had fewer and less serious cavities than the children who ate xylitol or sorbitol candy. The erythritol group also took longer to develop new cavities or to worsen existing ones.
The study concluded that erythritol can protect your teeth from decay better than xylitol.
So, what does this all mean for you? Well, it means that if you want to prevent tooth decay, you might want to choose products that contain erythritol over xylitol.
There is only one problem and this is a reason why I don’t include these sugars in the natural mouthwash recipe.
Consuming artificial sweeteners is not healthy at all.
Research has associated artificial sweeteners with a wide range of health conditions such as cancers and DNA damage, hepatotoxicity, migraines, and low birth weight.

Sugar alcohols like sorbitol and xylitol unlike erythritol are not absorbed, so they ferment in the colon and draw fluid into it and can have a laxative effect.
If you eat artificial sweeteners, they will alter the microbiome or in other words the bacteria that grow in your gut and in your mouth.
Erythritol is absorbed in the intestine without fermentation and does not have a laxative effect. It seems that it does not interact with metabolism and is excreted unchanged in the urine. It was considered to be the safest or the safest artificial sweetener.
The problem with erythritol is that a couple of new recent studies also found erythritol to be toxic. So the science is conflicting even on the topic of Erythritol.
If you want to use it in a natural mouthwash recipe be careful not to swallow. The rest of the ingredients are health-promoting but erythritol might not be. Even in the natural mouthwash, some part of it would get absorbed into the bloodstream so this is a decision you have to make for yourself.
Regarding potency for dental health, erythritol may be a more potent choice than xylitol. Erythritol is also less toxic. Erythritol is also safer for dogs.
Aloe Vera Mouthwash.
Aloe vera is a plant that has been used for centuries for its healing properties. It can soothe burns, heal wounds, treat infections, and relieve pain. It can also help your oral health by killing the harmful bacteria that cause plaque and cavities.
Different studies have shown that rinsing your mouth with Aloe vera juice can reduce plaque as effectively as chlorhexidine (Gupta et al., 2014), (Pattnaik et al., 2021).
In this study (Gupta et al., 2014), the researchers measured the amount and severity of plaque on the children’s teeth before and after the four-day period.
The study involved 300 healthy children who were divided into three groups. They all had their teeth cleaned by a dentist and then stopped brushing their teeth for four days. During this time, they rinsed their mouth three times a day with either Aloe vera juice, chlorhexidine mouthwash, or saline water (placebo).
A study found that both aloe vera and chlorhexidine groups had significantly less plaque than the placebo group.
There was no difference between aloe vera and chlorhexidine groups in terms of plaque reduction. Moreover, aloe vera did not cause any side effects, unlike chlorhexidine.
The study concluded that aloe vera is a safe and effective alternative to chlorhexidine for preventing plaque formation. Aloe vera can also benefit your overall health by boosting your immune system, improving your digestion, and hydrating your skin.
You will need fresh aloe vera juice or gel.
Natural Mouthwash Recipe.
Natural mouthwash properties:
- An antibiotic to kill bacteria.
- An antifungal to stop fungal growth.
- An antioxidant to ease pain and inflammation.
- A local anesthetic to relieve pain.
- A non-toxic solution even if swallowed and safe for children.
Natural mouthwash ingredients:
- 1 cup of distilled water.
- 3 to 5 teaspoons of green tea levees.
- 1 to 2 teaspoons of amla powder.
- 5 to 10 drops of oregano oil.
- 5 to 10 drops of clove oil.
- 5 to 10 drops of tea tree oil.
Optional ingredients:
- 1 to 2 drops of methylene blue (do not use more).
- 5 to 10 grams (teaspoon) of Aloe Vera gel.
- 5 to 10 grams (teaspoon) Erythritol.
- Mint and/or lemongrass essential oil for the taste.
Boil the water, add green tea levees and amla powder, and simmer for 10 minutes.
Remove from the heat and let the tea cool down.
Strain the water into the sterilized glass bottle or at least a glass bottle that is washed with alcohol and add the rest of the essential oils.
Ideally, use an air-tight or a vacuum glass bottle container and store it in a cool and dark place. If it is not used within a week throw the mouthwash away and make a new batch.
The concentration of the solution depends on your situation. If you have inflamed gums and cavities use the stronger solution with more of the optional ingredients that you can tolerate. For regular maintenance of oral health, 5 drops of essential oils are enough.
Use the natural mouthwash after brushing at least two times a day. This is a very potent solution and if swallowed might give you some nausea but also a high burst in ORAC value.
FAQ
References:
- Varoni, E., Tarce, M., Lodi, G., & Carrassi, A. (2012). Chlorhexidine (CHX) in dentistry: state of the art. Minerva stomatologica, 61(9), 399–419.
- Grassi, T. F., Camargo, E. A., Salvadori, D. M., Marques, M. E., & Ribeiro, D. A. (2007). DNA damage in multiple organs after exposure to chlorhexidine in Wistar rats. International journal of hygiene and environmental health, 210(2), 163–167. https://doi.org/10.1016/j.ijheh.2006.09.001
- Ribeiro D. A. (2008). Do endodontic compounds induce genetic damage? A comprehensive review. Oral surgery, oral medicine, oral pathology, oral radiology, and endodontics, 105(2), 251–256. https://doi.org/10.1016/j.tripleo.2007.07.045
- Erciyas, A. F., Erciyas, K., & Sarıkaya, R. (2010). Genotoxicity of two mouthwash products in the Drosophila Wing-Spot Test. Food and chemical toxicology : an international journal published for the British Industrial Biological Research Association, 48(10), 2577–2580. https://doi.org/10.1016/j.fct.2010.06.004
- Carlin, V., Matsumoto, M. A., Saraiva, P. P., Artioli, A., Oshima, C. T., & Ribeiro, D. A. (2012). Cytogenetic damage induced by mouthrinses formulations in vivo and in vitro. Clinical oral investigations, 16(3), 813–820. https://doi.org/10.1007/s00784-011-0559-2
- Pereira-Maróstica, H. V., Ames-Sibin, A. P., Pateis, V. O., de Souza, G. H., Silva, B. P., Bracht, L., Comar, J. F., Peralta, R. M., Bracht, A., & Sá-Nakanishi, A. B. (2023). Harmful effects of chlorhexidine on hepatic metabolism. Environmental toxicology and pharmacology, 102, 104217. https://doi.org/10.1016/j.etap.2023.104217
- Pereira-Maróstica, H. V., Ames-Sibin, A. P., Pateis, V. O., de Souza, G. H., Silva, B. P., Bracht, L., Comar, J. F., Peralta, R. M., Bracht, A., & Sá-Nakanishi, A. B. (2023). Harmful effects of chlorhexidine on hepatic metabolism. Environmental toxicology and pharmacology, 102, 104217. https://doi.org/10.1016/j.etap.2023.104217
- Mazur, M., Ndokaj, A., Jedlinski, M., Ardan, R., Bietolini, S., & Ottolenghi, L. (2021). Impact of Green Tea (Camellia Sinensis) on periodontitis and caries. Systematic review and meta-analysis. The Japanese dental science review, 57, 1–11. https://doi.org/10.1016/j.jdsr.2020.11.003
- Balappanavar, A. Y., Sardana, V., & Singh, M. (2013). Comparison of the effectiveness of 0.5% tea, 2% neem and 0.2% chlorhexidine mouthwashes on oral health: a randomized control trial. Indian journal of dental research : official publication of Indian Society for Dental Research, 24(1), 26–34. https://doi.org/10.4103/0970-9290.114933
- Hasan, S., Danishuddin, M., Adil, M., Singh, K., Verma, P. K., & Khan, A. U. (2012). Efficacy of E. officinalis on the cariogenic properties of Streptococcus mutans: a novel and alternative approach to suppress quorum-sensing mechanism. PloS one, 7(7), e40319. https://doi.org/10.1371/journal.pone.0040319
- Preuss, H. G., Echard, B., Dadgar, A., Talpur, N., Manohar, V., Enig, M., Bagchi, D., & Ingram, C. (2005). Effects of Essential Oils and Monolaurin on Staphylococcus aureus: In Vitro and In Vivo Studies. Toxicology mechanisms and methods, 15(4), 279–285. https://doi.org/10.1080/15376520590968833
- Cleff, M. B., Meinerz, A. R., Xavier, M., Schuch, L. F., Schuch, L. F., Araújo Meireles, M. C., Alves Rodrigues, M. R., & de Mello, J. R. (2010). In vitro activity of origanum vulgare essential oil against candida species. Brazilian journal of microbiology : [publication of the Brazilian Society for Microbiology], 41(1), 116–123. https://doi.org/10.1590/S1517-838220100001000018
- Chamdit, S. (2012). Antimicrobial Effect of Clove and Lemongrass Oils against Planktonic Cells and Biofilms of Staphylococcus aureus.
- Schroder, T., Gaskin, S., Ross, K., & Whiley, H. (2017). Antifungal activity of essential oils against fungi isolated from air. International journal of occupational and environmental health, 23(3), 181–186. https://doi.org/10.1080/10773525.2018.1447320
- Ripari, F., Cera, A., Freda, M., Zumbo, G., Zara, F., & Vozza, I. (2020). Tea Tree Oil versus Chlorhexidine Mouthwash in Treatment of Gingivitis: A Pilot Randomized, Double Blinded Clinical Trial. European journal of dentistry, 14(1), 55–62. https://doi.org/10.1055/s-0040-1703999
- Bahador, A., Lesan, S., & Kashi, N. (2012). Effect of xylitol on cariogenic and beneficial oral streptococci: a randomized, double-blind crossover trial. Iranian journal of microbiology, 4(2), 75–81.
- Söderling, E., & Pienihäkkinen, K. (2022). Effects of xylitol chewing gum and candies on the accumulation of dental plaque: a systematic review. Clinical oral investigations, 26(1), 119–129. https://doi.org/10.1007/s00784-021-04225-8
- de Cock, P., Mäkinen, K., Honkala, E., Saag, M., Kennepohl, E., & Eapen, A. (2016). Erythritol Is More Effective Than Xylitol and Sorbitol in Managing Oral Health Endpoints. International journal of dentistry, 2016, 9868421. https://doi.org/10.1155/2016/9868421
- Honkala, S., Runnel, R., Saag, M., Olak, J., Nõmmela, R., Russak, S., Mäkinen, P. L., Vahlberg, T., Falony, G., Mäkinen, K., & Honkala, E. (2014). Effect of erythritol and xylitol on dental caries prevention in children. Caries research, 48(5), 482–490. https://doi.org/10.1159/000358399
- Gupta, R. K., Gupta, D., Bhaskar, D. J., Yadav, A., Obaid, K., & Mishra, S. (2014). Preliminary antiplaque efficacy of aloe vera mouthwash on 4 day plaque re-growth model: randomized control trial. Ethiopian journal of health sciences, 24(2), 139–144. https://doi.org/10.4314/ejhs.v24i2.6
- Pattnaik, N., Mohanty, R., Satpathy, A., Nayak, R., Shamim, R., & Praharaj, A. K. (2021). Aloe vera mouthwashes can be a natural alternative to chemically formulated ones – A randomized-controlled trial. Journal of Taibah University Medical Sciences, 17(3), 424–432. https://doi.org/10.1016/j.jtumed.2021.10.006
- Cho, E., Park, Y., Kim, K. Y., Han, D., Kim, H. S., Kwon, J., & Ahn, H. (2021). Clinical characteristics and relevance of oral candida biofilm in Tongue smears. Journal of Fungi, 7(2), 77. https://doi.org/10.3390/jof7020077
- Kapil, V., Haydar, S. M., Pearl, V., Lundberg, J. O., Weitzberg, E., & Ahluwalia, A. (2013). Physiological role for nitrate-reducing oral bacteria in blood pressure control. Free Radical Biology and Medicine, 55, 93–100. https://doi.org/10.1016/j.freeradbiomed.2012.11.013
- Ansari, M. A., Fatima, Z., & Hameed, S. (2016). Antifungal Action of Methylene Blue Involves Mitochondrial Dysfunction and Disruption of Redox and Membrane Homeostasis in C. albicans. The open microbiology journal, 10, 12–22. https://doi.org/10.2174/1874285801610010012
Related Posts
Do you have any questions about nutrition and health?
I would love to hear from you and answer them in my next post. I appreciate your input and opinion and I look forward to hearing from you soon. I also invite you to follow us on Facebook, Instagram, and Pinterest for more diet, nutrition, and health content. You can leave a comment there and connect with other health enthusiasts, share your tips and experiences, and get support and encouragement from our team and community.
I hope that this post was informative and enjoyable for you and that you are prepared to apply the insights you learned. If you found this post helpful, please share it with your friends and family who might also benefit from it. You never know who might need some guidance and support on their health journey.
– You Might Also Like –

Learn About Nutrition
Milos Pokimica is a doctor of natural medicine, clinical nutritionist, medical health and nutrition writer, and nutritional science advisor. Author of the book series Go Vegan? Review of Science, he also operates the natural health website GoVeganWay.com
Medical Disclaimer
GoVeganWay.com brings you reviews of the latest nutrition and health-related research. The information provided represents the personal opinion of the author and is not intended nor implied to be a substitute for professional medical advice, diagnosis, or treatment. The information provided is for informational purposes only and is not intended to serve as a substitute for the consultation, diagnosis, and/or medical treatment of a qualified physician or healthcare provider.NEVER DISREGARD PROFESSIONAL MEDICAL ADVICE OR DELAY SEEKING MEDICAL TREATMENT BECAUSE OF SOMETHING YOU HAVE READ ON OR ACCESSED THROUGH GoVeganWay.com
NEVER APPLY ANY LIFESTYLE CHANGES OR ANY CHANGES AT ALL AS A CONSEQUENCE OF SOMETHING YOU HAVE READ IN GoVeganWay.com BEFORE CONSULTING LICENCED MEDICAL PRACTITIONER.
In the event of a medical emergency, call a doctor or 911 immediately. GoVeganWay.com does not recommend or endorse any specific groups, organizations, tests, physicians, products, procedures, opinions, or other information that may be mentioned inside.
Editor Picks –
Milos Pokimica is a health and nutrition writer and nutritional science advisor. Author of the book series Go Vegan? Review of Science, he also operates the natural health website GoVeganWay.com
Latest Articles –
Top Health News — ScienceDaily
- The overlooked nutrition risk of Ozempic and Wegovyon February 4, 2026
Popular weight-loss drugs like Ozempic and Wegovy can dramatically curb appetite, but experts warn many users are flying blind when it comes to nutrition. New research suggests people taking these medications may not be getting enough guidance on protein, vitamins, and overall diet quality, increasing the risk of muscle loss and nutrient deficiencies.
- A 25-year study found an unexpected link between cheese and dementiaon February 4, 2026
A massive Swedish study tracking nearly 28,000 people for 25 years found an unexpected link between full-fat dairy and brain health. Among adults without a genetic risk for Alzheimer’s, eating more full-fat cheese was associated with a noticeably lower risk of developing the disease, while higher cream intake was tied to reduced dementia risk overall. The findings challenge decades of low-fat dietary advice but come with important caveats.
- MIT’s new brain tool could finally explain consciousnesson February 4, 2026
Scientists still don’t know how the brain turns physical activity into thoughts, feelings, and awareness—but a powerful new tool may help crack the mystery. Researchers at MIT are exploring transcranial focused ultrasound, a noninvasive technology that can precisely stimulate deep regions of the brain that were previously off-limits. In a new “roadmap” paper, they explain how this method could finally let scientists test cause-and-effect in consciousness research, not just observe […]
- Why heart disease risk in type 2 diabetes looks different for men and womenon February 4, 2026
Scientists are digging into why heart disease risk in type 2 diabetes differs between men and women—and sex hormones may be part of the story. In a large Johns Hopkins study, men with higher testosterone had lower heart disease risk, while rising estradiol levels were linked to higher risk. These hormone effects were not seen in women. The results point toward more personalized approaches to heart disease prevention in diabetes.
- Sound machines might be making your sleep worseon February 4, 2026
Sound machines may not be the sleep saviors many believe. Researchers found that pink noise significantly reduced REM sleep, while simple earplugs did a better job protecting deep, restorative sleep from traffic noise. When pink noise was combined with outside noise, sleep quality dropped even further. The results suggest that popular “sleep sounds” could be doing more harm than good—particularly for kids.
- This unexpected plant discovery could change how drugs are madeon February 3, 2026
Plants make chemical weapons to protect themselves, and many of these compounds have become vital to human medicine. Researchers found that one powerful plant chemical is produced using a gene that looks surprisingly bacterial. This suggests plants reuse microbial tools to invent new chemistry. The insight could help scientists discover new drugs and produce them more sustainably.
- A hidden cellular process may drive aging and diseaseon February 3, 2026
As we age, our cells don’t just wear down—they reorganize. Researchers found that cells actively remodel a key structure called the endoplasmic reticulum, reducing protein-producing regions while preserving fat-related ones. This process, driven by ER-phagy, is tied to lifespan and healthy aging. Because these changes happen early, they could help trigger later disease—or offer a chance to stop it.
PubMed, #vegan-diet –
- Diet type and the oral microbiomeon February 2, 2026
CONCLUSION: The diet-oral microbiome-systemic inflammation axis is bidirectional and clinically relevant. Understanding both direct ecological regulation and indirect metabolic effects is essential to support precision nutrition strategies aimed at maintaining oral microbial balance and systemic inflammatory risk mitigation.
- Consensus document on healthy lifestyleson January 22, 2026
Proteins are a group of macronutrients that are vital to our lives, as they perform various functions, including structural, defensive and catalytic. An intake of 1.0-1.2 g/kg/body weight per day would be sufficient to meet our needs. Carbohydrate requirements constitute 50 % of the total caloric value and should be obtained mainly in the form of complex carbohydrates. In addition, a daily intake of both soluble and insoluble fiber is necessary. Regular consumption of extra virgin olive oil […]
- Vitamin B12 and D status in long-term vegetarians: Impact of diet duration and subtypes in Beijing, Chinaon January 21, 2026
CONCLUSIONS: This study reveals a dual challenge among Beijing long-term vegetarians: vitamin B12 deficiency was strongly associated with the degree of exclusion of animal products from the diet (veganism), while vitamin D deficiency was highly prevalent and worsened with longer diet duration. The near-universal vitamin D deficiency observed in this study suggests that, in the Beijing context, the risk may extend beyond dietary choice, potentially reflecting regional environmental factors;…
- Nutritional evaluation of duty meals provided to riot police forces in Germanyon January 13, 2026
Background: The primary role of the German riot police is maintaining internal security. Due to challenging working conditions, riot police forces face an elevated risk of various diseases. During duty, forces are provided with meals. A balanced diet can reduce the risk of some of these diseases and contribute to health-promoting working conditions. Aim: First evaluation of the nutritional quality of duty meals in Germany based on German Nutrition Society recommendations (DGE). Methods: In…
- Iodineon January 1, 2006
Iodine is an essential trace nutrient for all infants that is a normal component of breastmilk. Infant requirements are estimated to be 15 mcg/kg daily in full-term infants and 30 mcg/kg daily in preterm infants.[1] Breastmilk iodine concentration correlates well with maternal urinary iodine concentration and may be a useful index of iodine sufficiency in infants under 2 years of age, but there is no clear agreement on a value that indicates iodine sufficiency, and may not correlate with […]
Random Posts –
Featured Posts –
Latest from PubMed, #plant-based diet –
- From paddy soil to dining table: biological biofortification of rice with zincby Lei Huang on February 4, 2026
One-third of paddy soils are globally deficient in zinc (Zn) and 40% of Zn loss in the procession from brown rice to polished rice, which results in the global issue of hidden hunger, e.g., the micronutrient deficiencies in the rice-based population of developing countries. In the recent decades, biofortification of cereal food crops with Zn has emerged as a promising solution. Herein, we comprehensively reviewed the entire process of Zn in paddy soil to human diet, including the regulatory…
- Molecular Characterization of Tobacco Necrosis Virus A Variants Identified in Sugarbeet Rootsby Alyssa Flobinus on February 3, 2026
Sugarbeet provides an important source of sucrose; a stable, environmentally safe, and low-cost staple in the human diet. Viral diseases arising in sugarbeet ultimately impact sugar content, which translates to financial losses for growers. To manage diseases and prevent such losses from occurring, it is essential to characterize viruses responsible for disease. Recently, our laboratory identified a tobacco necrosis virus A variant named Beta vulgaris alphanecrovirus 1 (BvANV-1) in sugarbeet…
- Nutrition in early life interacts with genetic risk to influence preadult behaviour in the Raine Studyby Lars Meinertz Byg on February 3, 2026
CONCLUSIONS: Nutrition in early life and psychiatric genetic risk may interact to determine lasting child behaviour. Contrary to our hypothesis, we find dietary benefits in individuals with lower ADHD PGS, necessitating replication. We also highlight the possibility of including genetics in early nutrition intervention trials for causal inference.
- Effect of the gut microbiota on insect reproduction: mechanisms and biotechnological prospectsby Dilawar Abbas on February 2, 2026
The insect gut microbiota functions as a multifunctional symbiotic system that plays a central role in host reproduction. Through the production of bioactive metabolites, gut microbes interact with host hormonal pathways, immune signaling, and molecular regulatory networks, thereby shaping reproductive physiology and fitness. This review summarizes recent advances in understanding how gut microbiota regulate insect reproduction. Accumulating evidence demonstrates that microbial metabolites…
- Rationale and design of a parallel randomised trial of a plant-based intensive lifestyle intervention for diabetes remission: The REmission of diabetes using a PlAnt-based weight loss InteRvention…by Brighid McKay on February 2, 2026
CONCLUSIONS: This trial will provide high-quality clinical evidence on the use of plant-based ILIs to address the epidemics of obesity and diabetes to inform public health policies and programs in Canada and beyond.
- Diet type and the oral microbiomeby Daniel Betancur on February 2, 2026
CONCLUSION: The diet-oral microbiome-systemic inflammation axis is bidirectional and clinically relevant. Understanding both direct ecological regulation and indirect metabolic effects is essential to support precision nutrition strategies aimed at maintaining oral microbial balance and systemic inflammatory risk mitigation.